Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4722
Case Report(ISSN: 2637-4722) 
A Rare Case of a Variant of Type-C Esophageal Atresia with Double Distal Fistula (IIIb12). Is There a Need of a New Classification? Volume 4 - Issue 3
Teresa Mazaira Schreck2, Iris González Cabaleiro2, Silvia Gallego Vázquez2, Eva González Colmenero2, María Suárez Albo2, Ana Concheiro Guisan2, Pilar Fernández Eire1*
- 1*Pediatric Surgery department, Complejo Hospitalario Universitario de Vigo, Spain
- 2Neonatology department, Complejo Hospitalario Universitario de Vigo, Spain
Received: May 03, 2023 Published: May 12, 2023
Corresponding author: Pilar Fernández Eire, MD, Pediatric Surgery department, Complejo Hospitalario Universitario de Vigo, Spain
DOI: 10.32474/PAPN.2024.04.000187
Abstract
Esophageal atresia is the most common congenital anomaly of the esophagus. A wide variety of subtypes have been defined in the literature. Kluth’s classification is the most complete and descriptive one. To achieve an effective repair, it is vital to perform a tracheobronchoscopy before the operation, to study the anatomy of the respiratory tree and detect tracheoesophageal fistulas. We present the case of a preterm neonate in whom a pre- surgical bronchoscopy showed two distal tracheoesophageal fistulas, making the diagnosis of a type IIIb12 esophageal atresia (Kluth’s classification). An end-to-end anastomosis was performed, and we placed a dermal regeneration sheet to help prevent leakages. The surgery was well tolerated, and no major complications were observed. We would like to highlight the importance of performing a tracheobronchoscopy before the surgery. In our case, it allowed us to diagnose a rare case of esophageal atresia, and the complete analysis of the defect’s structure led us to a successful correction.
Keywords: Esophageal atresia; tracheobronchoscopy; tracheoesophageal fistula; Kluth’s classification; dermal regeneration sheet
Introduction
Esophageal atresia (EA) represents the most common congenital anomaly of the esophagus with an incidence of one in 2,500-4,500 live births [1]. The most widely used classification worldwide is the one described by Gross in 1953, where type C esophageal atresia represents the most common subtype in 80% of cases [2,3]. However, the best description was made by Kluth in 1976, who categorized it into 10 types (Table 1), each having 20 subtypes [4]. It is very important the understanding of the anatomy of the malformation to accomplish a successful repair and for this a pre-surgical bronchoscopy is an essential preoperative exploration. Benjamin [5] first highlighted the importance of preliminary tracheobronchoscopy (TBS) in the management of newborns affected by EA. It is useful for defining the anatomy of the respiratory tree, confirming the presence of tracheoesophageal fistula (TEF), the location and the exact site of entry [6]. We describe a patient with a type C esophageal atresia (IIIb12 according to Kluth’s classification) in whom the TBS allowed us to detect the unusual variant of EA such as double distal TEF.
Case report
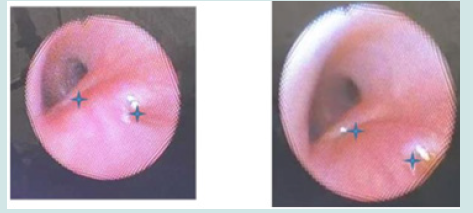
We present the case of a 31 weeks’ gestation male neonate born to a 32-year-old mother weighing 1594 g. Forty years ago, his father underwent surgery, because of the repair of a type III EA. The parents were not consanguineous. It was a trichorial-triamniotic pregnancy and prenatal ultrasound on the third trimester did not report polyhydramnios. Our patient was born at 31+3 weeks via c-section and was admitted to the Neonatal Intensive Care Unit. He required non- invasive mechanical ventilation during the first hours of life due to mild respiratory distress. The initial physical exam was normal. The diagnosis of EA was made when having difficulties passing an orogastric tube to manage secretions. An X-ray with intra-tracheal contrast was performed (Figure 1), which revealed a proximal dilated esophageal pouch and the presence of air in the stomach, the reason why a TEF was suspected. An 8 Replogle catheter was placed in the upper esophageal pouch to suction secretions. After ruling out major heart malformations, surgical correction was made on the second day of life.
Figure 1: Antero-posterior x-ray and esophagogram with water-soluble agent demonstrating EA. Dilated proximal esophageal pouch. A distal fistula is suspected due to the presence of gas in the stomach.
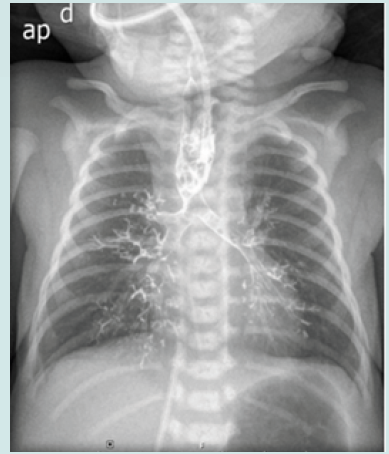
A pre-surgical bronchoscopy was carried out revealing a double distal fistula, with no signs of tracheomalacia. Both fistulas were located at the level of the trachea and opened 0.5-1 cm above the carina (Figure 2). A right thoracotomy was performed through the 4th intercostal space. We confirmed the presence of a double distal fistula and between them an esophageal segment reduced in its diameter. We carried out the cutting and closure of the fistulas and an end- to-end esophageal anastomosis with tension after resecting a minimal part of the proximal esophagus and the distal esophageal segment between fistulas. A dermal regeneration sheet (Integra®) was placed between the esophagus and closed TEFs. A transthoracic catheter was left for 24 hours. Trans anastomotic nasogastric feed commenced on the fifth postoperative day. An esophagogram was carried out (Figure 3), on the 12th post-surgical day which showed integrity of the anastomosis without leaks. After almost 3 months our patient remains asymptomatic.
Figure 3: Esophagogram performed on the 12th post-surgical day. No fistulas are observed, with satisfactory passage of contrast through the esophagus to the stomach.

Discussion
Although esophageal atresia is a surgical condition with a high overall survival rate (90%), the prognosis and the success of the intervention depend on the presence of possible associated malformations [7,8]. It is very important to study the anatomy of the esophageal atresia before surgical intervention to achieve a complete and successful repair. Preoperative TBS is the most useful exam in the diagnostic and therapeutic assessment of neonates affected by EA. It provides a more accurate anatomical definition of the anomaly than other diagnostic tools [9-11]. In our case, flexible bronchoscopy allowed the characterization of the two distal fistulas, which might otherwise have gone unnoticed. No absolute contraindications to TBS are reported in neonates. Relative contraindications include pulmonary hypertension and uncorrected bleeding diathesis. Flexible bronchoscopy provides the best assessment for epiglottic collapse, laryngomalacia, tracheomalacia and vocal cord paralysis. Our type of EA is an extremely rare variety and hardly reported in the literature in recent years. Moreover, the use of a biomaterial as an esophagotracheal coverage (Integra®) may represent a good alternative when tissues do not look so healthy. With that, our aim was to prevent leaks, and we achieved it successfully. Another of the main rarities in our case is the pattern of inheritance, since his father had presented type IIIb EA. Even though certain studies such as the one by Choinitzki et al. suggest that there is no increased risk of AE development in offspring, in recent years it has been revealed that some alteration in the FOX or Shh gene could be associated with the appearance of hereditary AE [12].
Funding
No funding or grant support.
Conflict of Interest
We declare that there is no conflict of interests.
References
- Lal DR, Gadepalli SK, Downard CD, Ostlie DJ, Minneci PC, et al. (2017) Perioperative management and outcomes of esophageal atresia and tracheoesophageal fistula. J Pediatr Surg 52(8): 1245-1251.
- Vogt EC (1929) Congenital atresia of the esophagus. AJR 22: 463.
- Gross RE (1953) Atresia of esophagus. Surgery of infancy and childhood, WB Saunders, Philadelphia, USA. pp. 75.
- Kluth D (1976) Atlas of esophageal atresia. J Pediatr Surg 11(6): 901-919.
- Benjamin B (1981) Endoscopy in esophageal atresia and tracheoesophageal fistula. Ann Otol Rhinol Laryngol 90(40 Pt 1): 376-382.
- F Parolini, G Boroni, S Stefini, Agapiti C, Bazzana T, et al. (2014) Role of preoperative tracheobronchoscopy in newborns with esophageal atresia: A review. World J Gastronitest Endosc 6(10): 482-487.
- Sistonen SJ, Pakarinen MP, Rintala RJ (2011) Long term results of esophageal atresia: Helsinki experience and review of literature. Pediatr Surg Int 27(11): 1141-1149.
- Tan Tanny SP, Comella A, Hutson JM, Omari TI, Teague WJ, et al. (2019) Thoracic Conditions Quality of life assessment in esophageal atresia patients: a systematic review focusing on long-gap esophageal atresia. J Pediatr Surg 54(12): 2473-2478.
- Ramirez-Martinez C, Peñarrieta-Daher A, Peña-Garcia M, Penchyna-Grub J, Teyssier-Morales G, et al. (2020) Type-C esophageal atresia with double distal fistula (IIIb13). J Ped Surg Case Reports 63: 101668.
- Puri A, Singh Yadav P, Saha U, Singh R, Chadha R, et al. (2013) A case series study of therapeutic implications of Type IIIb 4: a rare variant of esophageal atresia and distal tracheoesophageal fistula. J Pediatr Surg 48(7): 1463-1469.
- Negash S, Girma H, Woldeselassie HG (2020) Esophageal atresia type C with overlapping long upper pouch: a rare variant. Int J Surg Case Rep 72: 251-254.
- Choinitzki V, Zwink N, Bartels E, Baudisch F, Boemers TM, et al. (2013) Second study on the recurrence risk of isolated esophageal atresia with or without trachea-esophageal fistula among first-degree relatives: no evidence for increased risk of recurrence of EA/TEF or for malformations of the VATER/VACTERL association spectrum. Birth Defects Res Part A Clin Mol Teratol 97(12): 786-791.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...