Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4722
Research Article(ISSN: 2637-4722) 
A Qualitative Analysis of Knowledge, Perception and Practices related to Human Milk Banking among Staff Nurses and Lactating mothers, in a tertiary care hospital in South India Volume 4 - Issue 1
Sathya Jegannathan, Muthukumaran Natrajan, Manikumar Solaiappan, Ramya Shanmugam, Sandeep A Tilwani*
- Department of Neonatology, Chengalpattu Medical College and Hospital, Tamil Nadu, India
Received: December 30, 2022 Published: January 05, 2023
Corresponding author: Patankar Jahoorahmad Z, Consultant Pediatrician & Newborn Surgeon, Pediatric Urology and Laparoscopy, The Children’s Hospital Mumbai, India
DOI: 10.32474/PAPN.2023.04.000176
Abstract
Background: Breast-feeding is irrefutably the best form of nourishment for neonatal age groups. Banked human milk may be a suitable alternative for infants when mothers own milk is not available. However, there is resistance among lactating mothers regarding human milk donation. So, this study was done to find knowledge gaps, perception myths and practice concerns related to staff nurses of NICU and lactating mothers.
Materials and Methods: Semi Structured interviews and Focused Group Discussions were conducted among 16 Staff Nurses and 37 lactating mothers regarding their knowledge, perceptions, and milk banking practices. These were coded using Microsoft word & Qualitative Analysis was done to understand the possible barriers to milk donation in our setting.
Results: Staff nurses opined that DHM is safe and lifesaving. Challenges faced were limited supply of DHM because of low awareness on milk donation, shortage of trained staff, and less equipment’s. They stated that although most mothers were comfortable in donating milk, few were reluctant to donate milk as they feared shortage of milk for their own babies, or pain by use of machine for milk expression. Recipient mothers accepted the use of DHM but had concerns about donor mothers’ health and hygiene and measures for ensuring milk safety. Most grandmothers and fathers were resistant towards donating milk to the bank. Staff nurses shared opinions for scale-up, like improving awareness and infrastructure, lactation counselling by skilled personnel and improvement of family support.
Conclusion: There is a need to scale up the Human Milk Banking practices in Low Middle-Income Countries. For this, behaviour change communication targeted at mothers and family members about milk donation with help of IEC materials, skill-based counselling & building trust among them is necessary.
Keywords: Lactating mothers; breast-feeding; neonatal age; infants
Introduction
India remains the highest contributor of global burden of prematurity, LBW & also of neonatal mortality worldwide. It also contributes hugely to the global burden of malnutrition among children [1]. To tackle these challenges, in a low resource country like India, KMC and early exclusive breastfeeding are two proven costeffective interventions. Non breastfed infants are at 6 times more risk of mortality compared to breastfed infants [2]. Breastfeeding is expected to prevent around 1,60,000 deaths annually in children less than 5 years of age [3]. The WHO recommends the use of donor human milk (DHM) from a human milk bank (HMB), as the next best option to mothers’ own milk [4]. As compared to formula feeds, this donor human milk not only decreases chances of necrotizing enterocolitis and sepsis, but also decreases the stay in NICU and reduces the economic burden on family [5].
As of now, India has more than 50 milk banks, but this number is grossly inadequate to meet the demand of DHM in the country. The ‘‘National Guidelines on Lactation Management Centers in Public Health Facilities’’ was implemented in 2017 by the Government of India and has set a target to make breast milk available to all babies. HMBs shall be strengthened as part of lactation support centers to encourage breastfeeding, provide safe DHM to sick and vulnerable neonates without access to mother’s own milk [6]. Department of Neonatology at Chengalpattu Medical College has around 2200 admissions annually, with around 1400 admissions for LBW. We have a functional Human Milk Bank with average available donor milk of around 3 Liters. Average daily collection is around 400-500 ml, and around 8-10 babies are on DHM support on any given day. We felt a need to scale up the collection of DHM, so as to be able to support these babies. Therefore, formative research was conducted to study the knowledge, perception and practices related to milk banking among the staff nurses and lactating mothers and thereby to understand the possible barriers to milk donation in HMB.
Materials and Methods
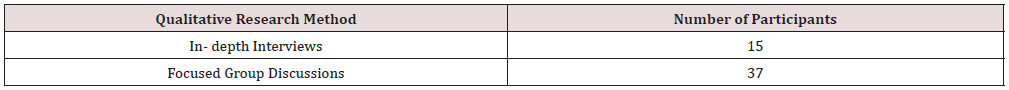
This study was conducted in the Department of Neonatology at Chengalpattu Medical College Hospital. Qualitative research methods were used for data collection. Questionnaires were based on questions asked in previous similar studies conducted by [7,8]. In- depth interviews using semi-structured questionnaire were conducted for 15 staff nurses and one lactation counsellor working in the department. We also conducted seven focused group discussions involving a total of 37 lactating mothers. The saturation point was attained after interviewing 37 mothers, decided on the basis of no new answers being found on further interviews.
These interviews and group discussions were audio taped after getting consent from the participants. The questionnaires were piloted and modified before data collection. Informed consent was taken from participants. The audio records were first translated into English from local language and then transcribed using the software “OTTER. ai”. Transcribed data quality was cross-checked with audio recordings to ensure completeness and accuracy of the transcription. Data were analyzed separately for each category of participants (staff nurses and lactating mothers) and then reanalyzed to assess similarities and differences in perceptions across respondent groups. These data were first coded in Microsoft Word. These codes were organized in major “Themes” that originated on the basis of the participant responses. Analysis of these themes provided an insight into the challenges faced by staff nurses in functioning of HMB and the barriers to milk donation among lactating mothers (Table 1).
Results
We separately analyzed the results of interviews and group discussions, to represent the knowledge, perceptions and practices related to DHM and HMB among mothers and staff nurses.
Data pertaining to Staff Nurses
Knowledge about HMB
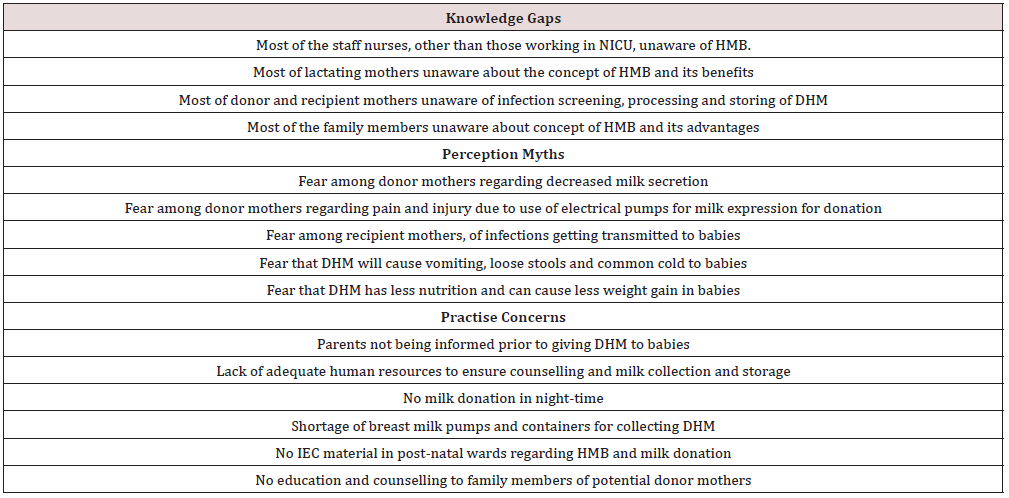
87.5% of the nurses admitted that they were not aware of the concept of HMB before it was opened in our unit. Only two nurses were aware of this concept beforehand. None of the staff nurses had worked in any other hospital with HMB before.
Perceptions about Milk Bank
All staff nurses agreed that having a milk bank is a good thing in our unit and that it is safe to use DHM, as milk is stored only after screening for microbes. They also agreed that availability of DHM has stopped the use of top feeds and formula feeds in the unit, even when mothers own milk is not available for some babies.
Banking Practices
Donor human milk is mainly used for preterm and Low Birth weight babies (63%); for babies born through LSCS in the immediate post operative period till the mother has adequate secretion established (81%); for babies having poor weight gain due to inadequate milk secretion in the mothers (62.5%); for unknown abandoned babies and for babies whose mothers are sick or have expired (93.7%). 62.5% of staff nurses agreed that they do inform the parents prior to giving DHM to the babies and get their consent. However resident doctors and consultants also inform the parents during counselling that their baby is receiving DHM from milk bank. 50% of the nurses felt that the collection of milk is not sufficient to fulfil the demands of our unit and that we need to scale up the milk collection in the milk bank. Others however felt that DHM collection is sufficient, since we have stopped liberal use of DHM and have started motivating mothers to give their own milk to the babies as far as possible. All the staff nurses agreed that there is shortage of human resources for motivating mothers, collection, and storage of DHM.
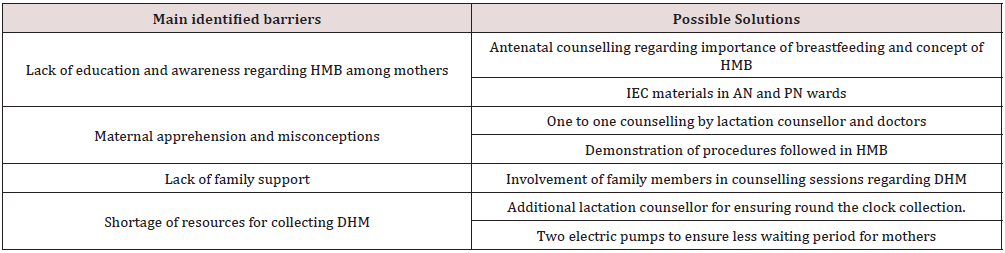
75% of them were of the opinion that if two lactation counsellors were available, they could motivate a greater number of mothers for milk donation. Also, most of the time, no DHM is accepted in nighttime, as there is no dedicated staff for HMB in night, and mothers are asked to come and donate excess milk in morning. This can also be taken care of by increasing the number of staff nurses in milk bank. “Sir, as of now we have only one lactation counsellor, who stays till 5 pm in the evening. So, if any mother comes from post-natal ward during night with engorged breast, we are not able to take excess milk from her to store in milk bank, since there is no dedicated staff for milk bank in night”. Most of the donors are from post-natal wards, mothers with engorged breasts, mothers whose babies are sick and not on full feeds. Sometimes at the time of discharge of baby from NICU, few mothers will donate milk and give to the bank as a goodwill gesture. Very rarely mothers from OPD will come to milk bank voluntarily to donate milk. Most of the staff nurses (93.7%), were aware of all the aseptic routines and agreed to follow them while collecting and storing milk. There is a shortage of equipment’s and containers for ensuring adequate milk collection as per 37.5% of staff nurses. One more electrical breast pump is needed, to ensure that mothers don’t have to wait in queue for donating milk. However, for maintenance of these extra equipment’s also, extra manpower is needed as per their opinion. “Definitely there is a shortage of the equipment’s. There is only one electric breast milk pump. So, if one more pump is there it will be better. We had two pumps initially but one of them is not working now so we have only one functional pump in our unit” (Table 2).
Perceived barriers for milk donation
Most of the mothers were reluctant to donate because of the fear of having inadequate milk secretion for their own baby, fear of weakness due to donation, fear of pain or injury due to use of machine for milk expression. There is a lack of adequate family support for the mothers as per 80% of staff nurses. Most of the time mother-in-law and husbands will oppose milk donation to milk bank. Staff nurses felt that convincing the mother-in-law is a very difficult task. “Once I saw that mother was ready to donate milk, but her mother-in-law told her that if you express excess milk for donation, you will become tired and will not be able your baby properly. So, there is no need to donate milk. You take care of your baby first”. To sustain an adequate milk supply, 93.7% of the staff nurses opined that there should be more IEC material in the form of educational videos and posters in postnatal wards and NICU, so as to encourage more mothers. Plus, additional human resources are needed to ensure round-the-clock availability of facility for milk donation (Table 3).
Data Pertaining to Lactating Mothers
The mean age of the participating mothers was 26(±3) years. Of the 37 participants, 6 had completed graduation, 19 had completed secondary education, 8 had primary education, while 4 had no formal education. 86.4% of mothers were comfortable donating milk to the bank. Although many were not familiar with the term ‘Human Milk Bank,’ they were aware that their donated milk is given to babies in need of mother’s milk. It was noted that readiness to donate milk increased with level of education (96% in women with secondary education and beyond versus 75% in those with primary education or less). Participant 14: “I have already donated milk twice to the bank, and I am willing to do it further, as long as I have adequate milk for my baby. If after feeding my baby, excess milk can be given to other babies in need, what better than that”.
78.3% of mothers were of the opinion that donating milk did not affect their own babies in any way because only the excess milk is donated. 11% mothers donated milk only for the reason of breast engorgement, with no will to donate otherwise to the milk bank. 75.6% of the mothers agreed to have inadequate family support for milk donation, with most of resistance being due to lack of knowledge among family members regarding milk banking. 73% of the mothers agreed to accept milk from HMB for their babies if needed, 27% of mothers were not ready to accept it initially. Acceptance was better among mothers with secondary education and beyond (84%) as against mothers with primary education or less (50%). 57% of mothers had concerns about hygiene and health of donor mothers. 83.7% of mothers were not aware of the sterilization measures followed in HMBs. A few mothers (11%) felt that DHM can cause abdominal distension, vomiting and loose stools among their babies as it is stored milk and not freshly expressed. 8% of mothers had concerns of baby getting common cold after use of DHM as it is frozen milk which is later thawed and given to babies. 16% of mothers were afraid that if the donor mother has some infection, it will get transmitted to their baby. 13.5% felt that DHM will have less nutrition for their baby as it is stored milk.
Participant 24: “The milk from milk bank is stored for many days. So obviously the nutrient content will be low, plus I am not sure whether it was stored properly in the bank in a clean manner”.
Discussion
The Government of India plans to scale up HMBs as a part of “Comprehensive Lactation Management Centre” model. We hope that this study by our unit will help to strategize, ways to increase acceptance and utilization of HMB services. This study is very useful in Indian context, as there is a huge gap between demand and supply of DHM and there are very few studies in this area. In our study, most of the staff nurses were not aware of the concept of HMB and procedures followed in it, before working in the unit. This points out the need for increasing awareness among medical professionals regarding the concept HMB and Donor human milk. Most of the staff nurses expressed positive opinions about expanding human milk banking as a lifesaving intervention for vulnerable babies. This was like the findings in a study by. done in Mumbai. However, nurses highlighted certain challenges such as limited supply of DHM because of low awareness on milk donation, shortage of trained staff, and risk of milk contamination.
Most of the staff nurses stated that mothers whose babies are sick and not on full feeds, expressed milk in limited quantities, just to suffice for their baby. This practice needs to be strongly discouraged as early expression of milk is associated with higher rates of exclusive breast feeding and other proven benefits. These findings emphasize the need for skill-based counselling of mothers starting as early as antenatal care (ANC) period, support at the time of birth and teaching milk expression in early post-natal period to increase their milk output and sustain breast milk supply for the babies after discharge, also supported these views. Having adequate number of lactation counsellors, strengthening lactation support and counselling by the service providers, especially nursing staff, will improve breastfeeding and milk expression for sufficient feeding of own babies and for donation. A supportive hospital environment will further help in reducing stress and building confidence among mothers.
[9] also pointed out that knowledge of nurses needs to be updated with the latest research. Shortage of trained and skilled staff meant that adequate time was not allocated for informing and motivating mothers and other family members for milk donation. Our study also highlights some of the concerns and fears mothers have regarding milk donation. Most of the perceptions are influenced by feelings of mother-in-law and husbands, who have minimal information about benefits of breast milk donation. Specific concerns and misconceptions of mother and families on milk donation like shortage of milk for their own babies, perceived weakness after donation, quality, and safety of donated milk, decrease in milk supply after donation can be addressed during counselling sessions through personalized approaches and greater involvement of family members during counselling had also reported similar challenges in their study.
Some of the other ways, identified in our study, to improve milk donation in HMB, are to increase the space; reduce overcrowding; availability of extra breast milk pumps to decrease the waiting time for post-natal mothers and availability of IEC material in postnatal wards to motivate mothers for milk donation. [10] studied the factors affecting breastmilk donation in Mumbai, India and reported that donation rates were higher in more educated women and highlighted the role of education in improving awareness about importance of milk donation. [11] also concluded that education level of mothers played an important role in supporting HMBs by improving maternal perceptions and acceptance of breastfeeding, DHM, and milk banking. Kimani‐Murage, et al concluded the same in their study among African women.8 Focused group discussions with mothers showed that while most of the mothers are aware about storage and donation of milk to other babies; they came to know about this only when their babies were admitted in NICU. After adequate counselling, most of the maternal concerns were reduced; but lack of family support is still a major resistance among the hesitating mothers.
This problem was also highlighted by in their study in Mumbai, India. Most of the staff nurses and lactating women believed that education to other family members especially mother-in-law and husbands will help to significantly escalate milk donation. One of the main limitations of this study is that the number of mothers interviewed is very small as compared to previously available studies in this area. However, since there are very few Indian studies in this context, with none being from South India, we feel the findings in this study will throw some light on the perceptions of mothers in this part of the country. Also, there are very few studies on this topic, where the knowledge and perceptions of staff nurses regarding Human Milk banks and DHM are studied, also highlighting the challenges faced by staff nurses in ensuring smooth functioning of Human Milk Banks.
Conclusion
With the launch of the ‘‘National Guidelines on Lactation Management Centers in Public Health Facilities,” the national government is committed to improve newborn and child health and reduce mortality by providing the best nutrition. However, for achieving this, we need to scale up the collection in HMBs by improving awareness through interactive IEC materials in hospitals and community, skill-based counselling from the ANC period with messages addressing concerns on HMB and DHM and building trust among mothers and family members.
References
- India Newborn Action Plan (2014) Ministry of Health and Family Welfare. Government of India.
- Victoria C, Bahl R, Barros Aluı´cio JD, Franca G, Horton S, et al. (2016) Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 387(10017): 475-490.
- Black RE, Allen LH, Bhutta ZA, Caulfield LE, Onis MD, et al. (2008) Maternal and child under-nutrition: Global and regional exposures and health consequences. Lancet 371(9608): 243-260.
- WHO (2011) Guidelines on Optimal Feeding of Low Birth-Weight Infants in Low- and Middle-Income Countries. Geneva: World Health Organization.
- Simmer K, Hartmann B (2009) The known and unknowns of human milk banking. Early Hum Dev 85(11): 701-704.
- Nangia S, Sachdeva RC, Sabharwal V (2018) Human milk banking: An Indian experience. Neo Rev 19(4): e201-e210.
- Mondkar J, Chugh SR, Shanbhag S, Khan A, Sinha MM, et al. (2018) Understanding barriers and facilitators for human milk banking among service providers, mothers, and influencers of preterm and sick neonates admitted at two health facilities in a metropolitan city in India. Breastfeed Med 13(10): 694-
- Kimani‐Murage EW, Wanjohi MN, Kamande EW, Macharia TN, Mwaniki E, et al. (2019) Perceptions on donated human milk and human milk banking in Nairobi, Kenya. Matern Child Nutr 15(4): e12842.
- Spatz DL, Pugh L, American Academy of Nursing Expert Panel on Breastfeeding (2007) The integration of the use of human milk and breastfeeding in baccalaureate nursing curricula. Nurs Outlook 55(5): 257-263.
- Katke RD, Saraogi MR (2014) Socio-economic factors influencing milk donation in milk banks in India: An institutional study. Int J Reprod Contracept Obstet Gynecol 3(2): 389-393.
- Goodfellow HE, Reimers P, Israel-Ballard K, Coutsoudis A (2016) Perceptions of community-based human milk bank before and after training in a resource-limited South African setting. South Afr J Child Health 10(1): 83-86.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...