Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4722
Mini Review(ISSN: 2637-4722) 
Rare Complication of Covid 19 in A Child Volume 4 - Issue 4
Sanjeev Sabale1, Rajesh Bagtharia2, Geeta Subramanian3 and Jeewan Rawal3*
- 1Paediatric Department, King’s College Hospital NHS Foundation Trust, UK
- 1Department of Paediatrics, Barking Havering, and Redbridge Hospitals NHS Trust, UK
- 1Consultant Paediatrician, Barking Havering, and Redbridge Hospitals NHS Trust, UK
Received:September 14, 2023; Published:September 29, 2023
Corresponding author:Jeewal Rawal, Consultant Paediatrician, Barking Havering, and Redbridge Hospitals NHS Trust, UKn
DOI: 10.32474/PAPN.2023.04.000195
Case Report
A 15-year-old boy was presented to the emergency department, with one day history of severe respiratory distress, blood-stained sputum, and right sided chest pain. He had been a healthy child previously, with no history of ill health except mild infection with Covid-19, 2 weeks prior to presentation. He was not vaccinated against Covid-19 virus. On examination, he was tachypneic and tachycardic and hypoxic with initial oxygen saturations of 88% in room air. He was afebrile and normotensive. He was in pain with a high pain score. He had moderate work of breathing, was alert and noted to be obese. On chest auscultation breath sounds were reduced on both sides with bilateral expiratory wheeze. Cardiovascular, abdominal and CNS examination were unremarkable.
Investigations Revealed the Following
a) WCC (13.0 x108 / L), CRP (37mg/dl), troponin (19 ng/l),
normal clotting, a normal chest x-ray, and ECG with sinus
tachycardia.
b) He was managed with high flow oxygen, burst therapy
with salbutamol and ipratropium nebulisers, oral steroids like
in acute asthma with antibiotic cover. He was given morphine
for his intense chest pain.
c) There was no improvement in his general condition as he
continued to have respiratory distress.
d) He was still in considerable chest pain which was out
of proportion to his respiratory distress despite morphine
administration.
Questions
1. What are the differential diagnoses?
2. What is the most likely diagnosis?
3. What investigations if any would you do to get a diagnosis?
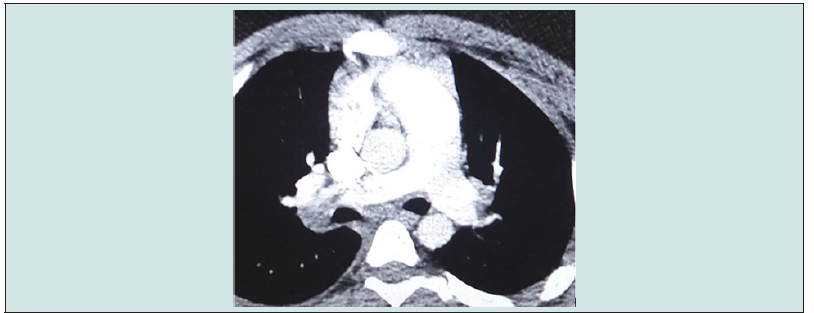
4. What are the findings in CTPA? (Figure1a)
5. How would you manage this case?
6. What additional investigations would you consider in this
case?
7. What is the likely cause of this condition?
Answers
1. This case presented as acute respiratory distress, chest
pain and hypoxia which are the symptoms of most chest related
conditions like [1].
Acute Asthma, Tracheitis, Pneumonia, Pleuritis, Pneumothorax,
Pleural effusion, Pulmonary Embolism, Chest crisis in sickle
cell disease, Acute Pericarditis, Chest. Trauma, Diabetic
ketoacidosis.
2. Pulmonary embolism was the most likely diagnosis.
Severe chest pain and haemoptysis are important clues with no
response to burst therapy for Asthma. Normal X- Ray of chest
ruled out pneumothorax, pleural effusion, and pneumonia. A
normal ECG made cardiac causes less likely.
3. He was severely hypoxic and wheezy. He was treated for
acute asthma but showed poor response. He was in severe pain
needing opioid analgesia which is unusual in acute asthma.
Therefore, a decision was made to rule out PE. An urgent CTPA
was arranged which was the most appropriate investigation
[2]. The D dimer was abnormally high - >35mg/L (0.0-0.5mg/
L).
Figure 1b reveals:
Filling defect in main pulmonary artery (yellow arrows1), Filling defect in left pulmonary artery (yellow arrows2), Filling defect in right pulmonary artery (yellow arrows3), Confirming a large volume bilateral pulmonary embolus.
5. After initial assessment and stabilisation with ABCDE,
the case was discussed with tertiary specialists. He was put on
subcutaneous Enoxiparin 100 mg twice a day. He was transferred
to PICU for main pulmonary artery thrombolysis via directed
catheter followed by heparin transfusion. He was stepped down
from intensive care and started on twice daily Dalteparin which
was subsequently converted to oral anticoagulants – Rivaroxaban
for 6 months.
a) Doppler studies of leg veins were reported normal ruling out
deep vein thrombosis.
b) Cardiac ECHO helps to define cardiac extension of the
thrombus, right ventricular strain, and dysfunction as was in
our case.
c) Thrombophilia screen, ANA, Connective Tissue Disease
antibodies were normal.
6. In children with COVID-19 infection, thromboembolic complications are exceptional but reported [4,5] more frequent in hospitalized children unlike in our case [6]. We believe COVID -19 infection triggered Pulmonary Embolism in our patient. The thrombophilia screen was negative. To the best of our knowledge, this is a rare case of paediatric pulmonary embolism following COVID-19 infection in Britain which did not require intensive care treatment.
References
- Martin samuels, Sue Weiteska (2017) Advanced paediatric life support, sixth edition.
- Daniel R Quelette, Annie Harrington, Nader Kamangar (2020) Pulmonary Embolism.
- Sirisha Emani, Andrew Torres, Fatoumata Diallo, Mamadou Diallo, Meena Nathan, et al. (2020) Abstract 16904: Hypercoagulability in Pediatric Patients Infected With SARS-Coronavirus 2. Circulation 142: A16904.
- Amal El Ouarradi, Nabila Chekhlabi, Mahassine Elharras, Ilham Bensahi, Sara Oualim, et al. (2021) Acute pulmonary embolism in a child following SARS- CoV-2 infection: a case report. Pan Afr Med J 38: 125.
- Gautam K Visveswaran, Kavita Morparia, Shalu Narang, Cindy Sturt, Michael Divita, et al. (2020) Severe Acute Respiratory Syndrome Coronavirus 2 Infection and Thrombosis: Phlegmasia Cerulea Dolens Presenting with Venous Gangrene in a Child; Chest. J Pediatr 158(6): e269-e27.
- Melissa Chima, Duane Williams, Neal J Thomas, Conrad Krawiec (2021) COVID-19-Associated Pulmonary Embolism in Pediatric Patients. Hosp Pediatr 11(6): e90-e94.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...