Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4722
Research Article(ISSN: 2637-4722) 
10-Year Analysis of Pediatric Blunt Abdominal Trauma: Accident Mechanisms and Prevention Volume 3 - Issue 4
Melanie Kapapa1*, Katharina Esswein2 and Alexandre Serra1
- 1Division of Pediatric Surgery, Department of Surgery, Ulm University Medical Center Eythstrasse 24, 89075 Ulm, Germany
- 2Department of Visceral, Transplant and Thoracic Surgery, Center of Operative Medicine, Medical University of Innsbruck, Innsbruck, Austria
Received: April 26, 2022 Published: May 10, 2022
Corresponding author: Melanie Kapapa, MD, MA, Department of Surgery (Division of Pediatric Surgery), Ulm University, Eythstrasse 24, 89075 Ulm, Germany
DOI: 10.32474/PAPN.2022.03.000167
Abstract
Background: This study analyzed the mechanisms and management of child blunt abdominal trauma to optimize prevention strategies.
Aim and objectives: We identify risk factors for organ injuries and their influence on increasing morbidity and mortality. Injury characteristics including age, gender, injury mechanism, clinical presentation and complications were included.
Methods: This is a retrospective cohort analysis (n=134) over 10 years at a tertiary hospital. All data was statistically evaluated including descriptive analysis accepting a confidence interval of 95%.
Results: Most common mechanisms of injuries were falls (56%), sport-related (41.8%) and road-traffic accidents (21.6%). Sonography was primarily performed in 85.8% and identified a correlation between free abdominal fluid, abnormal laboratory (p<0.001) and injury pattern (p<0.001). In 41.8% an organ laceration and in 46.3% additional injuries were found, 67.9% were boys and suffered of an intraabdominal injury (p=0.034) with higher scores for severity (p=0.014). Complications (34.4%) occurred significantly higher after spleen (p=0.001), liver (p=0.001) and gastrointestinal injuries (p=0.001) especially after child abuse.
Conclusions: Prevention is key to reduce accidental intra-abdominal and abuse-related injuries. The risk for a non-accidental etiology increases if factors like difficult social circumstances, low family income, parental substance abuse or mental illness and family violence are combined to male gender.
Keywords: Child Abuse; Pain; Pediatrics; Preventive Medicine
Key Message
What is already known on this topic: Falls are a very common occurrence in childhood and are also often trivialized by parents or other caregivers. In this case, it is imperative to look closely and take an accurate medical history, as potential risks for organ injuries can often be deduced.
What this study adds: This study, which spans a period of 10 years in a tertiary hospital, also considers cases of child abuse. In order to avoid overlooking the rare resulting injuries, which can also be fatal if they occur, it is important to train all persons involved in safe diagnosis and treatment.
How this study might affect research, practice or policy: As children have their whole lives ahead of them, it is even more important to focus on their health and to protect this vulnerable group through prevention of accidents and, in the case of child abuse, through structured support services and consistent application of existing laws. A first step would be to include children’s rights in the constitution.
Introduction
Mechanisms of blunt abdominal trauma in children are diverse and age-related [1]. In Europe and North America, the most common injuries result from road traffic accidents, followed by falls and sport-related trauma [2,3]. Toddlers suffer accidents mostly at home, whilst in older children the place of injury shifts to educational facilities and leisure activities [4]. In road traffic accidents younger children are mostly involved as pedestrians or motor-vehicle passengers, but when they get older also as active participants [5]. Since different trauma mechanisms cause different injury patterns, an early and correct diagnosis is essential and has to be based on the knowledge of the local epidemiology of trauma and injury [6, 7]. Moreover, abdominal injuries are serious and even potentially lethal, they can be difficult to diagnose and induce severe early complications, therefore the management with a specialized pediatric trauma team essential [8]. The risk of injury and severity increases with the number of injured organs and thus also the possible complication rate. Spleen and liver are the most common injured organs, followed by kidney, pancreas and gastrointestinal tract (GI) although these are rather seldom affected [2]. Specifically, common mechanisms for pancreas injuries are accidents with bicycles, while seat belt restraints, especially when incorrectly used may lead to GI injuries [8]. In non-accidental traumas, GI injuries are far more common but in these cases their diagnosis may be often delayed [9]. This study was therefore designed to assess if the epidemiology of pediatric abdominal traumas in Southwest Germany also followed the general pattern or whether there were regional differences that have to be consider in managing such patients. Specifically, we aimed to test and assess the following parameters: [1] evaluation of gender differences; [2] assessment of typical trauma mechanisms for intraabdominal injuries (IAI) and non-IAI; [3] establish the most appropriate diagnostics using laboratory parameters and radiologic imaging, [4] evaluate resulting injuries, treatment and complications; [5] verify the occurrence and percentage of child abuse in abdominal trauma [6] recommend new prevention strategies based on the analysed data.
Methods
Design: The study was designed to assess retrospectively all children treated for blunt abdominal trauma at the tertiary Medical Center which met the inclusion criteria. Data from patients enrolled in the study was obtained from medical records, hospital files, surgical reports and radiologic examinations. The study was approved by the local ethics committee (No. FSt/Sta; Trial registration 19.07.2017).
Inclusion criteria: All patients aged 0-17 years (n=134) who were admitted with blunt abdominal trauma from January 1, 2005, to December 31, 2015, and treated primarily at the tertiary hospital were included. Patients were divided in two groups: one with an intraabdominal injury (IAI), which includes injuries of the spleen, liver, kidneys, pancreas or GI tract and a second group without these injuries, called non-IAI.
Exclusion criteria: Patients were excluded from the study if the primary treatment was not performed at the University of Ulm; if there were no anamnestic indication of abdominal trauma; if there were penetrating abdominal injuries; if the diagnostics showed diagnosis other than blunt abdominal trauma, like iatrogenic injuries; gut perforation caused by necrotic enterocolitis or focal intestinal perforation, volvulus, inguinal hernia or urachal infection and if the patient’s documentation was incomplete. A total of 31 patients were excluded from the study due to these reasons.
Patients and surveyed subjects: From the 134 patients admitted with blunt abdominal trauma and included in the study 122 were treated as inpatients (91%) while 12 as outpatients (9%).
Data Collection: Data were anonymously collected and analyzed based on the medical records, laboratory findings, surgical reports and radiologic imaging study results. The collected data were transferred into a database and analyzed. The main points of interest were patient´s age and gender, mechanism of injury, possible foreign objects involved in the accident, severity of the injuries (IAI or non-IAI), clinical-, laboratory- and radiologic findings, conservative or surgical treatment, evidence of child abuse, complications and duration of hospital stay.
Statistics: Recorded data were initially analyzed with descriptive methods and clearly outlined for initial appraisal. The mean, standard deviation, median and range were reported for quantitative parameters, while absolute and relative frequencies were calculated for qualitative parameters. Exploratory tests between interesting subsets were selected based on the underlying parameters. Given the size of the subsets, the t-test and non-parametric tests such as Wilcoxon and Kruskal-Wallis were performed in addition to ANOVA, including post-hoc testing such as Bonferroni. Significance was established as p ≤ 0.05. All statistical tests were performed using the IBM SPSS® software, version 24 (IBM, Armonk, NY, USA).
Results
Age and Gender: Our collective consisted of 76 male- (56.7%) and 58 female children (43.3%). Boys suffered more often (67.9%) an IAI (p=0.034) with higher scores for severe injury (p=0,014), and in both genders in older age (p=0.008). Mean age for blunt abdominal trauma without IAI was 7.3 years (±4,6), in children with isolated IAI 10 years (±4,6) and in children with multiple IAI 10.5 years (±5,6) (Figure 1).
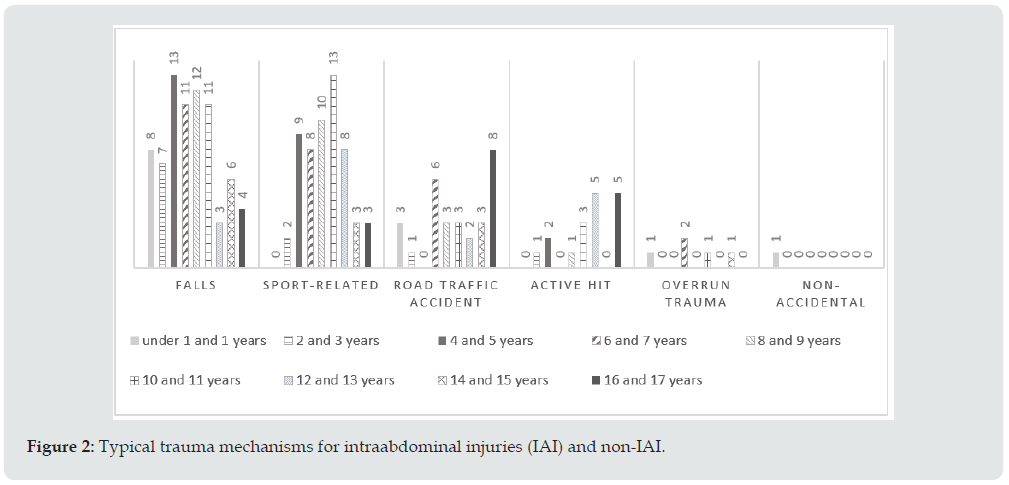
Trauma mechanism: The mechanisms for abdominal trauma were highly dependent on the age of the affected child. The most common trauma mechanism was a fall in 56% of children (n=75), usually below one meter (n=42; 56%), followed by sport-related trauma in 56 patients (41.8%), road traffic accidents in 29 (21.6%) and active hit during (related to human or animal contact) in 17 (12.7%) children. Twenty-seven children (36.2%) suffered of an IAI after a fall, 21 children (28.14%) with IAI were involved in road-traffic accidents and 19 (25.46%) with IAI suffered of sport-related traumas. The association between road traffic accidents and IAI was highly significant (p<0.001). Interestingly, eighty percent of accidents involving a domestic object, like steps or furniture, did not lead to an IAI (p=0.025). Seventy-eight children with non-IAI had a fall (61.5%) or sport-related accidents (47.4%). One child had multiple IAI after child abuse (1.3%) (Figure 2).
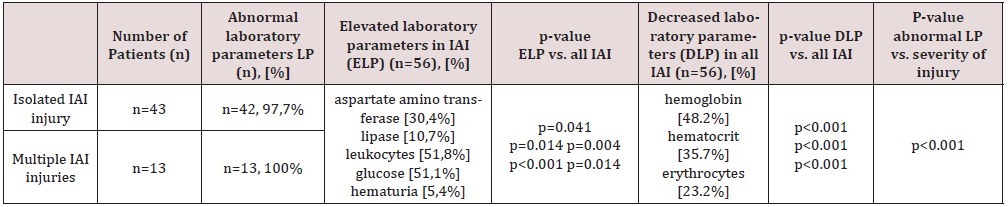
Laboratory studies: In 84.3% of the children (n=113) at least one laboratory parameter was altered, and the severity of the injury in these was also significantly higher (p<0.001). A decrease in hemoglobin (48.2% of the patients, p<0.001), hematocrit (35.7%, p<0.001) and erythrocytes (23.2%, p<0.001) was significantly more common in children with IAI (n=56). Conversely, aspartate aminotransferase (p=0.041), lipase (p=0.014), leukocytes (p=0.004) and glucose (p<0.001) were significantly elevated in these children. We have also determined a significant correlation between IAI and hematuria (p=0.014) and urinary retention (p=0,029). Children with multiple IAI had in 100% of the cases abnormal laboratory results (n=13), while in children with isolated IAI (n=43) had abnormal results in 97.7% (Table 1).
Radiologic studies: The initial imaging diagnostic was the Focused Assessment with Sonography for Trauma (FAST) in 85.8% of the children (n= 115). Computer tomography (CT) was performed in 6 children (4.7%) initially, all of them polytrauma patients. The association of free abdominal fluid and severe injury patterns was significant (p<0.001), like in multiple affected organ injuries (Data not shown).
Resulting injuries: From the collective of 134 children 41.8% had an IAI (n=56), which 76.7% were isolated (n=43) and 23.2% multiple (n=13). Affected organs were mostly the spleen (40.3%), liver (26.4%), kidney (15.3%), GI-tract (12.5%) and pancreas (5.6%). 19.5% of IAI patients were classified as polytrauma patients (n=11), they suffered in 87.5% (n=10) significantly more often liver injuries (p<0.001) and in 14.3% (n=8) an intubation at the trauma scene was necessary. Seventyeight children (58.2%) had non IAI. Additional extra-abdominal injuries were seen in 62 children (46.3%), mainly head trauma (n=39; 29.1%), thorax (n=26; 19.4%), hips (n=11; 8.2%), arm/ shoulders (n=10, 7.5%), face (n=8.6%), and neck/lumbar spine (n=2 each; 1.5%). Of these, traumas in the thorax (p=0.001), arms with shoulders (p<0.001) and legs with hips (p=0.008) were significantly associated with IAI and thus severe trauma. Additionally, extra abdominal injuries were seen frequently in combination with liver injuries (89.5%, p<0.001), GI in 55.6%, pancreas in 50%, spleen in 48.3% and kidneys in 45.5%. Visible skin alterations were reported in 35 children (26.1%), of which 40% (n=14) had IAI; seat belt restraints were causal in 8 children and of those 2 suffered a GI injury (Figure 3).
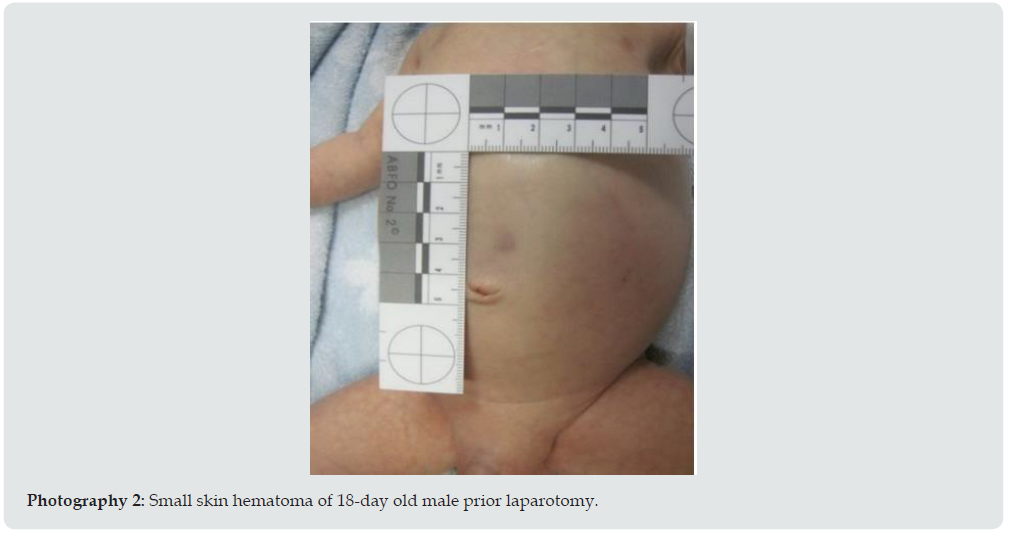
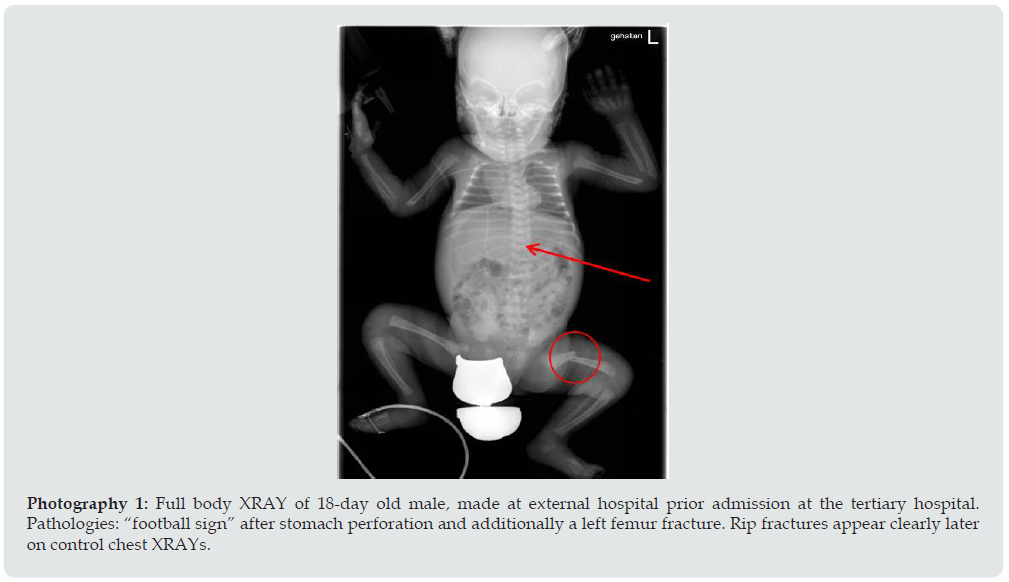
Non-accidental injuries/ child abuse and neglect: Fortunately, only two cases of non-accidental injuries were observed in our cohort: in the first one, a newborn boy was seen with a small abdominal skin hematoma after suffering multiple IAI (rupture of spleen, liver, and a 4cm tear of dorsal stomach), as well as extra abdominal injuries (ribs and femur fracture). A second child (toddler) was treated for a liver injury after falling on the pavement from the 1st floor window without supervision (Photography 1 and 2).
Figure 4: Full body XRAY of 18-day old male, made at external hospital prior admission at the tertiary hospital. Pathologies: “football sign” after stomach perforation and additionally a left femur fracture. Rip fractures appear clearly later on control chest XRAYs.
Treatment: A primary conservative therapy was performed in 60.7% (n=34) of children with IAI after injuries of the liver (n=14), kidney (n=8) and spleen (n=17). However, in 6 children with IAI (17.6%) surgical treatment was required after failure of the primary conservative therapy. Surgical treatment was performed in 22 children (39.2%) with IAI caused by spleen (34.5%), liver (26.3%) or kidney (27.3%) ruptures. The indication for surgical treatment were pathological radiologic studies (n=19; 86.4%) combined with signs of bleeding (n=10; 45.5%), indications for surgical treatment after failure of conservative treatment were clinical deterioration (n=7; 31.8%), worsening laboratory values (n=7; 31.8%) and increasing inflammatory markers (n=2; 9.1%). Surgical treatment due to extra abdominal injuries was performed in 5.2% of all patients (n=7) (Figure 4).
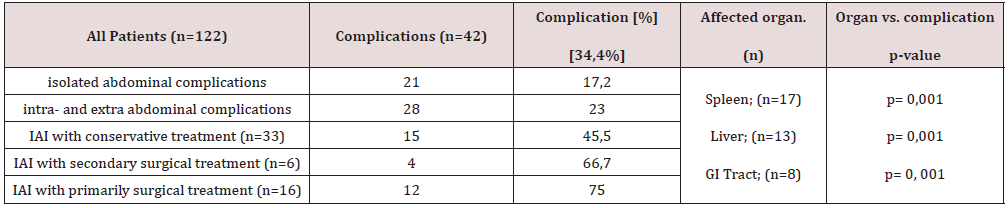
Complications: Complications were described in 34.4% of all inpatient children (n=42). Twenty-one had isolated abdominal complications (n=21; 17.2%) and 28 had additionally extraabdominal complications (23.0%). These complications were seen after conservative treatment in IAI patients in 45.5% (n=15), after secondary surgical treatment in 66.7% (n=4) and after primary surgical treatment in 75% (n=12). Complications were significantly more frequent after spleen injury (p=0.001), liver (p=0.001) and GI tract injuries (p=0.001). One polytrauma patient with multiple organ lacerations (liver, spleen and various blood vessels) after a rollover trauma died during an emergency abdominal exploration because of acute circulatory failure (Table 2).
Duration of hospital stay: Thirty children (24.6%) were treated in an intensive care unit (ICU), and the average ICU duration stay was 11.8 days (± 39.3; range 1-219; median 4 days). The mean duration of overall hospital stay was 9.78 ± 9.8 days, (range 1-44 days; median 5 days), excluding the proven case of child abuse. Hospital duration stay increased significantly with the severity of injury (p<0.001): patients with multiple IAI (n=12) stayed hospitalized on average 23 days (51.7 ± 99.5; range 11-366) while children with isolated IAI (n=42) stayed on average 14 days in the ward (16.6 ± 9.3; 3-44).
Due to the legal implications and a very lengthy treatment the hospital discharge was greatly delayed in those children with proven child abuse and neglect (366 and 44 days, respectively). Sixteen patients were discharged prematurely against medical advice after their parents interrupted the treatment (Data not shown).
Discussion
Based on the results summarized in the previous chapter we were able to test and assess all parameters described in the introduction.
Evaluation of gender differences: It is widely known that boys are up to 81% more frequently involved in accidents [2,3,5], and that a significant association between gender, intraabdominal injury and severity of injury exist [7]. In our study and that of other boys lead the IAI’s “hit list”, whether isolated or multiple, possibly due to a higher willingness to take risks [10], in accidents caused by equestrian sports girls are more often affected [3]. Every child should be informed and prepared for dangers of sports, since only an aware child can be more careful and try to avoid accidents, naturally in the extent possible due to limitations of individual age and maturity. A good example is the consequent and frequent use of a helmet and suitable protective clothing during sports like cycling, roller blading or riding.
Assessment of typical trauma mechanisms for IAI and non- IAI: The higher incidence of falls is due to the ever-increasing mobility of children when growing up [11]. Our data showed a peak for accidents due to falls in the 2-3 years old age group, in which the involved objects were mostly domestic ones, yet these falls seldom led to an IAI. However, Unni et al. showed that even low-level falls could lead to severe injuries [12]. These home accidents are almost entirely preventable, so parents should strive for safe home environment. In all age groups riding the bicycle is a common leisure activity [13], falls are frequently [14] and not trivial [6]. In this setting the typical trauma mechanism for pancreas injuries is being hit by the handlebar [8], therefore pain after cycling abdominal trauma should always be taken seriously. This illustrates well why a thorough clinical examination, laboratory and abdominal ultrasounds are mandatory in every examination in a pediatric emergency room after abdominal trauma. In regard to other vehicle accidents, the typical trauma patterns are dependent on children´s age [5] and 3 out of 10 children with GI tract injuries were involved in a car accident as occupants [15]. In this case, the reason seems to be universally a suboptimal restraint of the child [16,17], therefore it is imperative to inform and educate parents about correct safety of children in a car by using an ageadapted seat and properly restraining seat belt.
Establish the most appropriate diagnostics using laboratory parameters and radiologic imaging: Holmes et al. identified six laboratory parameters which were highly suggestive of IAI [18]. In our study, we found a significant association of the presence of IAI with a decrease of hematocrit, hemoglobin and erythrocytes, with elevated AST, lipase, total leukocytes and glucose, particularly after a road accident, in patients with abnormal urinary output and in patients with thoracic-, shoulder-, pelvic- or leg injuries. In terms of imaging diagnostics, the sensitivity of ultrasound has been reported to differ between 41-72% [19]. Rozycki et al. described limitations especially in identifying low-grade organ injuries [20] and other showed that often initially no free fluid could be detected [21]. We do not corroborate these findings since we found free fluid in 26.9% of cases without IAI. A possible explanation for that is the variability in the experience of the examiner with pediatric ultrasound, therefore we emphasize that ultrasound should always be assessed in conjunction with other pathological findings. Holmes et al. reported that if certain parameters suggestive of an IAI were present like hypotension, haemoperitoneum and free abdominal fluid further radiological diagnostics are recommended [22]. The implementation of abdominal CT scan after trauma is useful for a quick and reliable assessment of internal organ injuries [20]. However, the radiation exposure should always be considered, and Cotton et al. described the use of CT scan in 15% of children without an IAI [23]. The sensible use of radiological diagnostics is an important element in treatment of blunt abdominal trauma. Therefore, the management should ideally be decided by an interdisciplinary team to avoid over- or under diagnosis.
Evaluate resulting injuries, treatment and complications: The precise knowledge of each individual accident mechanism is important to assess resulting injuries, since nearly every organ in the body can be affected. However, in most cases a quick assessment following the decreasing order of frequency (namely spleen -> liver -> kidneys -> GI-tract -> pancreas) may save valuable time to the begin of the therapy. Children with “seat belt sign” have a 200-fold or more risk for an intraabdominal injury [24]. Every abdominal wall bruising, either accidental or due to child abuse multiplies the risk for an IAI and therefore plays an important role in diagnostics [14,21,25]. Miller et al. has further shown that in all children with head injuries who undergo surgery there are also abnormalities in the clinical and FAST abdominal examinations [26]. Patients who die after blunting abdominal trauma often suffer of head trauma combined to injuries of liver and vessels [27]. In regard to the therapy modalities, most liver and kidney injuries can be treated conservatively with success. However, less than 50% of spleen injuries are able to be treated conservatively. Children with GI injuries have to be operated after a primary conservative in nearly 50% of the cases, mostly due to delayed diagnosis and sepsis complications. The appropriate treatment of abdominal traumas is always a challenge, as often the initially suspected injury is not the only one. Moreover, it is difficult to get adequate information on pain location or intensity from young children which may lead to a delay in diagnosis. One suggested approach to prevent this factor is to educate parents about the most common dangers and, in the event of an accident, to encourage them to provide adequate first aid and not to downplay the symptoms. As an example, an unobserved bicycle crash has to be treated as a potentially blunt abdominal trauma through handlebar until proven otherwise.
Verify the occurrence and percentage of child abuse in abdominal trauma: In our cohort 2 children (3.5%) suffered child abuse culminating in IAI. In these cases, we confirmed the known risk-factors for child abuse, like young age, male gender [28] and a medical history which is not fitting to the injury pattern [29,30]. One newborn boy was so severely abused that he had to undergo several surgeries (56 in total) with varied complications, resulting in an extended hospital stay of 366 days (which is well known for non-accidental injuries) [9,28]. A careful anamnesis of the accident history with a critical assessment of the plausibility of the mechanism is essential to detect child abuse, especially in very young children. If child abuse is overlooked, the consequences due to serious injuries can be easily fatal, since the necessary and appropriate (surgical) treatment is often delayed.
Conclusion
Blunt abdominal trauma is common in children and can lead to various organ injuries with life-threatening complications. Depending on the affected organs, different medical management strategies are necessary. In our cohort of southern German children most patients could be treated conservatively, yet an adequate and prompt surgical intervention was required when the patients’ showed signs of clinical deterioration. Additionally, every symptom such as pain after an abdominal trauma must to be taken seriously. A thorough clinical examination, laboratory and abdominal ultrasound are the minimum requirement in a pediatric emergency room after abdominal trauma and have been shown to successfully identify IAIs in our patients. Moreover, a careful assessment of the plausibility of the accident is essential to detect cases of child abuse. In our opinion, the best way to reduce the incidence of pediatric trauma is prevention, and this should be mostly addressed to the parents, since most accidents happen at home or in the immediate proximity of a parent. Further strategies have to include parental information, in early childhood optimally during preventive examinations by their pediatrician.
Limitation- Selection
A major strength of our study is that it was performed in a representative cohort of a tertiary hospital, in which the variation of accident types is high and even polytraumatized, unstable and severely wounded patients are managed. This care is always provided by a multi-professional team, which enabled us to have reproducible and verifiable data for all the endpoints of the study in the entire period, including time and modus of accident, admission, conservative or surgically treatment, and short-term outcome including the whole pediatrics ICU stay until discharge. However, our study has also limitations since it is only a retrospective analysis and based on a single-center hospital observation. Nonetheless, a prospective study with different prevention modalities based on the data acquired in this study is currently being planned.
Acknowledgement
First and Second author are equally contributed.
References
- Pal'a A, Kapapa M, Posovszky C, Roderer G, Konig R, Woischneck D, et al. (2015) Head Injury in Children: Has a Change in Circumstances Caused an Increase in Treatment Numbers? J Child Neurol 30(9): 1153-1158.
- Wisner DH, Kuppermann N, Cooper A, Menaker J, Ehrlich P, Kooistra J, et al. (2015) Management of children with solid organ injuries after blunt torso trauma. J Trauma Acute Care Surg 79(2): 206-214.
- Adelgais KM, Kuppermann N, Kooistra J, Garcia M, Monroe DJ, Mahajan P, et al. (2014) Accuracy of the abdominal examination for identifying children with blunt intra-abdominal injuries. J Pediatr 165(6): 1230-1235.
- Kahl H, Dortschy R, Ellsasser G (2007) [Injuries among children and adolescents (1-17 years) and implementation of safety measures. Results of the nationwide German Health Interview and Examination Survey for Children and Adolescents (KiGGS)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 50(5-6): 718-727.
- Debus F, Lefering R, Frink M, Kuhne C, Mand C, Ruchholtz S (2015) [Polytrauma in children and adolescents. Choice of the primary care clinic and importance of pediatric traumatology competence centers]. Unfallchirurg 118(5): 432-438.
- Shah S, Sinclair SA, Smith GA, Xiang H (2007) Pediatric hospitalizations for bicycle-related injuries. Inj Prev 13(5): 316-321.
- Kapapa T, Konig K, Pfister U, Sasse M, Woischneck D, Heissler H, et al. (2010) Head trauma in children, part 1: admission, diagnostics, and findings. J Child Neurol 25(2): 146-156.
- De Blaauw I, Winkelhorst JT, Rieu PN, van der Staak FH, Wijnen MH, Severijnen RS, et al. (2008) Pancreatic injury in children: good outcome of nonoperative treatment. J Pediatr Surg 43(9): 1640-1643.
- Roaten JB, Partrick DA, Nydam TL, Bensard DD, Hendrickson RJ, Sirotnak AP, et al. (2006) Nonaccidental trauma is a major cause of morbidity and mortality among patients at a regional level 1 pediatric trauma center. J Pediatr Surg 41(12): 2013-2015.
- Buschmann C, Kuhne CA, Losch C, Nast Kolb D, Ruchholtz S (2008) Major trauma with multiple injuries in German children: a retrospective review. J Pediatr Orthop 28(1): 1-5.
- Wang MY, Kim KA, Griffith PM, Summers S, McComb JG, Levy ML, et al. (2001) Injuries from falls in the pediatric population: an analysis of 729 cases. J Pediatr Surg 36(10): 1528-1534.
- Unni P, Locklair MR, Morrow SE, Estrada C (2012) Age variability in pediatric injuries from falls. Am J Emerg Med 30(8): 1457-1460.
- Schneiders W, Rollow A, Rammelt S, Grass R, Holch M, Serra A, et al. (2007) Risk-inducing activities leading to injuries in a child and adolescent population of Germany. J Trauma 62(4): 996-1003.
- Schwebel DC, Brezausek CM (2014) Child development and pediatric sport and recreational injuries by age. J Athl Train 49(6): 780-785.
- Streck CJ, Lobe TE, Pietsch JB, Lovvorn HN (2006) Laparoscopic repair of traumatic bowel injury in children. J Pediatr Surg 41(11): 1864-1869.
- Durbin DR, Arbogast KB, Moll EK (2001) Seat belt syndrome in children: a case report and review of the literature. Pediatr Emerg Care 17(6): 474-477.
- Lutz N, Arbogast KB, Cornejo RA, Winston FK, Durbin DR, Nance ML (2003) Suboptimal restraint affects the pattern of abdominal injuries in children involved in motor vehicle crashes. J Pediatr Surg 38(6): 919-923.
- Holmes JF, Sokolove PE, Brant WE, Palchak MJ, Vance CW, Owings JT, et al. (2002) Identification of children with intra-abdominal injuries after blunt trauma. Ann Emerg Med 39(5): 500-509.
- Poletti PA, Kinkel K, Vermeulen B, Irmay F, Unger PF, Terrier F (2003) Blunt abdominal trauma: should US be used to detect both free fluid and organ injuries? Radiology 227(1): 95-103.
- Rozycki GS, Knudson MM, Shackford SR, Dicker R (2005) Surgeon-performed bedside organ assessment with sonography after trauma (BOAST): a pilot study from the WTA Multicenter Group. J Trauma 59(6): 1356-1364.
- Streck CJ, Jewett BM, Wahlquist AH, Gutierrez PS, Russell WS (2012) Evaluation for intra-abdominal injury in children after blunt torso trauma: can we reduce unnecessary abdominal computed tomography by utilizing a clinical prediction model? J Trauma Acute Care Surg 73(2): 371-376.
- Holmes JF, Brant WE, Bond WF, Sokolove PE, Kuppermann N (2001) Emergency department ultrasonography in the evaluation of hypotensive and normotensive children with blunt abdominal trauma. J Pediatr Surg 36(7): 968-973.
- Cotton BA, Beckert BW, Smith MK, Burd RS (2004) The utility of clinical and laboratory data for predicting intraabdominal injury among children. J Trauma 56(5): 1068-1074.
- Borgialli DA, Ellison AM, Ehrlich P, Bonsu B, Menaker J, Wisner DH, et al. (2014) Association between the seat belt sign and intra-abdominal injuries in children with blunt torso trauma in motor vehicle collisions. Acad Emerg Med 21(11): 1240-1248.
- Sokolove PE, Kuppermann N, Holmes JF (2005) Association between the "seat belt sign" and intra-abdominal injury in children with blunt torso trauma. Acad Emerg Med 12(9): 808-813.
- Miller D, Garza J, Tuggle D, Mantor C, Puffinbarger N (2006) Physical examination as a reliable tool to predict intra-abdominal injuries in brain-injured children. Am J Surg 192(6): 738-742.
- Stylianos S (2005) Outcomes from pediatric solid organ injury: role of standardized care guidelines. Curr Opin Pediatr 17(3): 402-406.
- Lane WG, Dubowitz H, Langenberg P, Dischinger P (2012) Epidemiology of abusive abdominal trauma hospitalizations in United States children. Child Abuse Negl 36(2): 142-148.
- Carter KW, Moulton SL (2016) Pediatric abdominal injury patterns caused by "falls": A comparison between nonaccidental and accidental trauma. J Pediatr Surg 51(2): 326-328.
- Maguire SA, Upadhyaya M, Evans A, Mann MK, Haroon MM, Tempest V, et al. (2013) A systematic review of abusive visceral injuries in childhood--their range and recognition. Child Abuse Negl 37(7): 430-45.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...