Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
The Different Clinical Manifestations and Diagnostic Strategies of Isolated Sphenoid Non-Invasive Fungal Sinusitis Volume 4 - Issue 2
Ali Almomen1*, Hussain Al Baharna2, Abdullah A AlShakhs3, Mohammed A Alfalah3, Mohammed AlSaeed3, Ali AlTuraifi3 and Njood Alaboud3
- 1Consultant Rhinology & Skull base surgery, King Fahad Specialist Hospital, Kingdom of Saudi Arabia
- 2ENT Consultant, Qatif Central Hospital, Kingdom of Saudi Arabia
- 3Medical Intern, Saudi Program, Kingdom of Saudi Arabia
Received: March 11, 2020; Published: April 06, 2020
Corresponding author: Ali Almomen, Consultant Rhinology & skull base surgery, King Fahad Specialist Hospital, Dammam, Kingdom of Saudi Arabia
DOI: 10.32474/SJO.2020.04.000184
Abstract
Objective: To present the different clinical manifestations and diagnostic strategies of isolated sphenoid non-invasive fungal sinusitis (SNIFS) in order to prevent delayed diagnosis and providing early management.
Method: This study is a retrospective clinical study, conducted between January 2008 to November 2019. It was done in the ENT department of two institutes: King Fahad specialist Hospital and Qatif Central Hospital, Saudi Arabia. Only patients with sole involvement of non-invasive fungal sinusitis in the sphenoid sinus were included.
Conclusion: The incidence of SNIFS is rare. However, it’s clinically important because untreated SNIFS can cause significant complications. The clinical features of SNIFS are ambiguous and nonspecific which make its diagnosis more difficult. Post-nasal discharge and headache refractory to the medical management is the most common symptom of SNIFS. CT scan is still the cornerstone of radiological diagnosis of SNIFS. Endoscopic sinus surgery is the standard care of management.
Keywords: Sphenoid sinus, Fungal ball, allergic fungal sinusitis, non-invasive fungal sinusitis, endoscopy, allergic fungal rhinosinusitis
Abbreviations: SNIFS: Sphenoid Non-Invasive Fungal Sinusitis; SAFRS: Sphenoid Allergic Fungal Rhinosinusitis; ISFB: Isolated Sphenoid Fungal Ball; FB: Fungal Ball; AFRS: Allergic Fungal Rhinosinusitis
Introduction
Histopathological, fungal rhinosinusitis can be divided into invasive and noninvasive infection. Noninvasive fungal rhinosinusitis is further subdivided into fungal ball (FB) and allergic fungal rhinosinusitis (AFRS) [1, 2]. FB is an accumulation of dense fungal hyphae, most commonly in the maxillary sinus [1]. AFRS is an immunological reaction to fungal antigen rather than a fungal infection. Interestingly, it is common in immunocompetent younger patient with atopic background, with similar findings and presentation as in chronic rhinosinusitis [3]. Sphenoid sinusitis is usually present in concurrent with other sinuses. However, in rare cases isolated sphenoid has been reported, which represent only 2.7% of all sinus diseases [3,4]. There are several important structures adjacent to sphenoid sinus which vulnerable to injury through any sphenoid sinus lesion, including the pituitary gland, optic nerve and chiasm, middle cranial fossa, internal carotid artery, cavernous sinus, the dura, pterygoid canal and nerve and cranial nerve III, IV, V1, V2, and VI [1,2]. Even though isolated sphenoid sinus lesion is rare, it’s very significant clinically due to its undetectable anatomical location, ambiguous symptoms and the complications associated with injury to the above structures [5]. The main focus of this study is to present the different clinical manifestations and diagnostic strategies of isolated sphenoid non-invasive fungal sinusitis (SNIFS), in order to prevent delayed diagnosis and providing early management. It was conducted at King Fahad Specialist Hospital (KFSHD), and Qatif Central Hospital, Eastern region, Saudi Arabia.
Method
This is a retrospective clinical study which was conducted in
the otolaryngology department of King Fahad specialist Hospital
and Qatif Central Hospital, Saudi Arabia, from January 2008 to
November 2019. Patients included were:
a) Isolated sphenoid non-invasive fungal sinusitis which
were confirmed by computed tomography (CT) and/or magnetic
resonance imaging (MRI).
b) 2- intraoperative evidence of non-invasive fungal sinusitis
within the sphenoid sinus.
Result
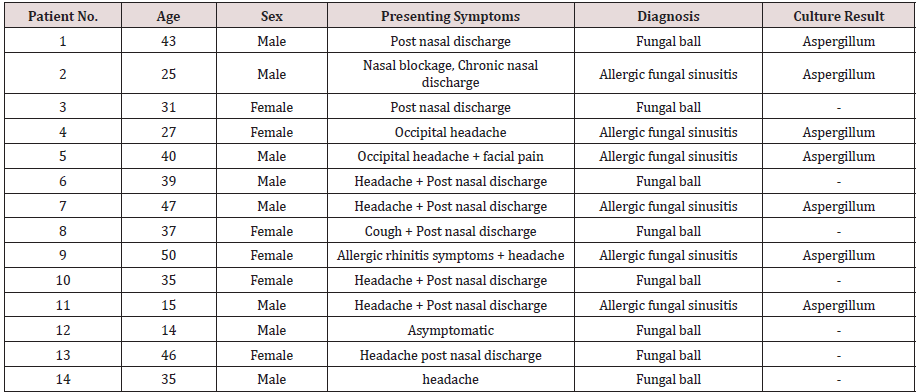
A diagnosis of isolated sphenoid fungal ball and allergic fungal rhinosinusitis had been made in 14 patients with the age ranging between 14-50 years old. 8 were males and the 6 remaining were females. The most common symptoms were headache and nasal discharge. Even though CT scan was the most important tool in the diagnosis, the conformation of the diagnosis was made either intraoperatively or by fungal culture. The management was only surgical. The only organism found was Aspergillum in these patients. Summarization of all cases found in [Table1].
Discussion
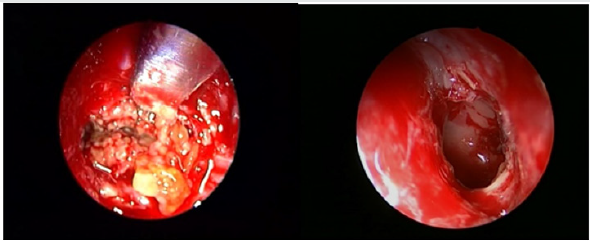
Fungal ball
The exact mechanism of spread of fungal infection only to sphenoid sinus is unknown. It has been hypothesized that ostial closure creates an anaerobic environment favorable for growth of Aspergillus, or that chronic sinusitis predisposes to the development of FB [2]. The clinical presentation of isolated sphenoid sinus lesions is often nonspecific and vague; thus, diagnosis may be delayed in many cases [6]. Up to date, headache refractory to the medical management is the most common symptom of isolated sphenoid sinus lesion; it presents in 70 to 90% of patients [7-9]. In this series, the most presenting feature was post-nasal discharge followed by headache and rarely cough. History and physical examination have little benefit in establishing the correct diagnosis. Imaging studies (CT scanning and/or MRI) and Nasal endoscopy are essential for a thorough evaluation and management [8,10]. All patient did CT scan which provided valuable information regarding the diagnosis of fungal ball and its relation to bony erosion(Figure1). MRI should only provide for patient with suspicion of invasion to surrounding structures. MRI provides more precise information regarding its relationship to the cavernous sinus, dura, optic nerve, carotid artery and pituitary gland [11]. On Nasal endoscopy the most common findings are bone thickening or sclerosis of sinus walls (Figure2). This can be secondary to the inflammatory process associated with the fungal ball and is often reversible after removing it [2,6]. Microbiology confirms fungal infection and eventually identifies fungal species. The microscopic appearance of Aspergillus on direct smear is that of a conidiophore [12]. On culture, the most frequently isolated fungus is Aspergillus fumigates. One of our fungal ball cases showed aspergillusbut the remaining 7 cases had -ve culture. The surgical management of sphenoid sinus include both endoscopic and open techniques. However, endoscopic surgery has become the fundamental approach for sphenoid sinus lesions. It can be proceeded in a trans-ethmoidal fashion or through the anterior sphenoid sinus wall directly at the site of the natural ostium [13]. It’s necessary to open the sphenoid sinus and allowing complete removal of fungal debris by suction and multiple washing. Because all patients had noninvasive fungal ball no post-operative medical treatment was necessary. Post-operative follows up was done for all patient with no complication and recurrence.
Figure 1: A computed tomography (CT) scan, coronal view of the paranasal sinuses, showing a hyperdense opacity filling the sphenoid sinus.

Figure 2: Endoscopic intraoperative view of The sphenoid sinus after sphenoidotomy showing Fungal material inside sinus cavity.
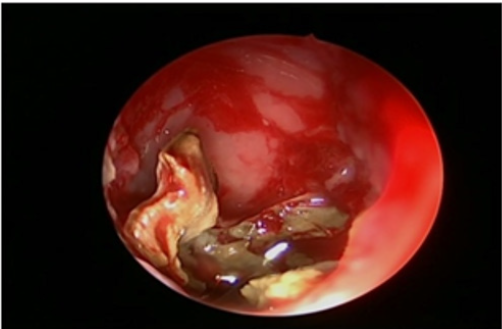
Allergic fungal sinusitis
The clinical presentation of SAFRS is often nonspecific and vague; thus, diagnosis may be delayed in many cases [6]. Up to date, headache refractory to the medical management is the most common symptom of isolated sphenoid sinus lesion; it presents in 70 to 90% of patients [7,9]. In this series, the most presenting feature was headache followed by nasal discharge. History and physical examination have little benefit in establishing the correct diagnosis. Imaging studies (CT scanning and/or MRI) and Nasal endoscopy are essential for a thorough evaluation and management [8,10]. All patient did CT scan which provided valuable information regarding the diagnosis of SAFRS and its relation to bony erosion (Figure3). Endoscopic surgery has become the fundamental approach for SAFRS. It’s includes surgical debridement of fungal material in order to open and ventilate the sinuses (Figure4), and post-operative steroid to control the recurrence. There are few reports about complication of ISAFRS. Actually, the main complication of allergic comes after sphenoid sinus involvement. The main complications are visual disturbances, diplopia and cavernous sinus thrombosis[14-15]. We have reported one case in our series with cavernous sinus thrombosis as a complication of isolated sphenoid allergic fungal sinusitis. Left sphenoidotomy was done and she was treated with Meropenem, Vancomycin, Amphotericin B and Enoxaparin and improved.
Figure 3: A computed tomography (CT) scan, coronal view showing a heterogeneous opacity filling the sphenoid sinus.
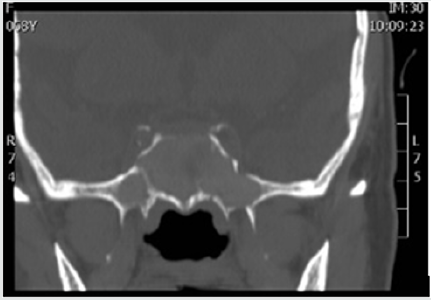
Figure 4: (A) Intraoperative endoscopic view of the allergic mucin and fungal mud filling the sphenoid sinus. (B) Endoscopic view of the Post-operative wide sphenoidotomy procedure.
Conclusion
Even though isolated sphenoid fungal ball is rare, it’s clinically important because untreated SNIFS can cause significant complications. The clinical features of SNIFS are ambiguous and nonspecific which make its diagnosis more difficult. Post-nasal discharge and headache refractory to the medical management is the most common symptom of SNIFS. CT scan is still the cornerstone of radiological diagnosis of SNIFS. Endoscopic sinus surgery is the standard care of management. Post-operatively, the majority of patient had good results with no complication and recurrence.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Sources of funding
There is no financial support and sponsorship.
Consent
Written informed consent was obtained from the parents for publication of this case report on behalf of the patient.
References
- Grosjean P, Weber R (2007) Fungus balls of the paranasal sinuses: A review. Eur Arch Otorhinolaryngol 264(5):461-470.
- Chakrabarti A, Denning DW, Ferguson BJ, Ponikau J, Buzina Wet al. (2009) Fungal rhinosinusitis: a categorization and definitional schema addressing current controversies. Laryngoscope 119(9): 1809-1818.
- Hnatuk LA, Macdonald RE, Papsin BC (1994) Isolated sphenoid sinusitis; the Toronto Hospital for sick children experience and review of the literature. J Otolaryngol23(1):36-41.
- Lew D, Southwick FS, Montgomery WW, Weber AL, Baker AS (1983) Sphenoid sinusitis. A review of 30 cases. N Engl J Med 309(19):1149-1154.
- Sethi DS (1999) Isolated sphenoid lesions: diagnosis and management. Otolaryngol Head Neck Surg 120(5):730-736.
- Cakmak O, Shohet MR, Kern EB (2000) Isolated sphenoid sinus lesions. Am J Rhinol 14(1):13-19.
- Wyllie JW, Kern EB, Djalilian M (1973) Isolated sphenoid sinus lesions. Laryngoscope 83:1252-1265.
- Lawson W, Reino A (1997) Isolated sphenoid sinus disease: an analysis of 132 cases. Laryngoscope 107(12pt 1):1590-1595.
- Martin TJ, Smith TL, Smith MM, Loehrl TA (2002) Evaluation and surgical management of isolated sphenoid sinus disease. Arch Otolaryngol 128(12):1413-1419.
- Wang ZM, Kanoh N, Dai CF (2002) Isolated sphenoid sinus disease: an analysis of 122 cases. Ann OtolRhinolLaryngol 111(4):323-327.
- Lee LA, Huang CC, Lee TJ (2004) Prolonged visual disturbance secondary to isolated sphenoid sinus disease. Laryngoscope 114(6):986-990.
- Bardana EJ Jr (1981) The clinical spectrum of aspergillosis–part 2: Classification and description of saprophyticallergic and invasive variants of human disease. Crit Rev Clin Lab Sci 13(2):85-159.
- Metson R, Gliklich RE (1996) Endoscopic treatment of sphenoid sinusitis. Otolaryngol Head Neck Surg 114(6):736-744.
- Veress B, Malik OA, El Tayeb AA, El Daoud S, Mahgoub ES, et al. (1973) Further observations on the primary paranasal aspergillus granulomas in Sudan: a morphological study of 46 cases. Am J Trop Med Hyg 22:765-772.
- Bent JP 3rd, Kuhn FA (1994) Diagnosis of allergic fungal sinusitis. Otolaryngol Head Neck Surg 111(5):580-588.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...