Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Study of Brainstem Evoked Response Audiometry to Assess Hearing Loss in High Risk Children Below 5 Years Volume 5 - Issue 1
Suganshi Garg1 and Borlingegowda Viswanatha2*
- 1Senior Resident, ENT Department, Bangalore Medical College and Research Institute, India
- 2Professor & Head of ENT Department, Bangalore Medical College and Research Institute, India
Received: August 19, 2020; Published: August 28, 2020
Corresponding author:Viswanatha B, Professor Department of Otorhinolaryngology, Bangalore Medical College and Research Institute, India
DOI: 10.32474/SJO.2020.05.000204
Abstract
Early detection of hearing loss and intervention is very important for the development of normal speech and language. A prospective study of brainstem evoked response audiometry to access hearing loss in high risk children below 5 years of age, to find out the incidence of hearing loss in children from high risk category and to determine the threshold of hearing by brainstem evoked response audiometry in high risk children by observing wave ‘V’ at the minimum intensity of click stimulus. 100 children having one or more high-risk factors for hearing loss (up to 5 years of age) according to the inclusion criteria had been selected for the study from the outpatient department. This study showed that BERA was found to be a useful, accurate tool to detect the type of hearing loss and the site of defect in auditory transmission of sound. This aids in planning the mode of intervention for early rehabilitation for speech and language development.
Keywords: Brainstem evoked response audiometry; hearing loss; high risk children
Introduction
Early detection of hearing loss and intervention is very important for the development of normal speech and language. In India, 63 million people (6.3%) suffer from significant auditory loss. Four in every 1000 children suffer from severe to profound hearing loss. With over 100,000 babies that are born with hearing deficiency every year approximately 50% of all cases of congenital hearing loss are attributable to environmental factors such as congenital hyperbilirubinemia, ototoxic medication exposure, neonatal hypoxia, viral infections, and meningitis. The other 50% of cases are thought to be inherited, i.e., of genetic causes. Of these hereditary cases approximately 30% are classified as syndromic [1]. In a developing country like India newborn hearing screening is yet to be implemented. Joint committee on infant hearing recommends BERA (brainstem evoked response audiometry) technology as the only appropriate screening technique for use in the NICU (neonatal intensive care unit) (Figures 1-3). For infants who do not pass BERA testing in the NICU referral should be made directly to an audiologist for rescreening and when indicated comprehensive evaluation including diagnostic BERA should be done [2]. BERA is a far-field recording of the synchronized response of numerous neurons in the auditory pathway within the brainstem. BERA was first described by Sohmer and Feinmesser in 1967. It reflects neural activity generated at the level of the brainstem because of which it is not strongly affected by attention, sleep, or sedation [3].
Objectives
a) To find out the incidence of hearing loss in children from
high risk category by brainstem evoked response audiometry.
b) To determine the threshold of hearing by brainstem
evoked response audiometry in high risk children by observing
wave ‘V’ at the minimum intensity of click stimulus.
Materials and Methods
100 children having one or more high-risk factors for hearing loss (up to 5 years of age) according to the inclusion criteria had been selected for the study from the outpatient department of Bangalore Medical College and Research Institute, Bangalore for from August 2019 to July 2020. General physical examination was conducted to know the health status and to rule out any deformities in the subjects. Any local pathology present in ear, nose and throat was treated and BERA was carried out in all children.
Inclusion criteria
Following high risk children are included in the study
a) History of intrauterine infections (congenital infections)
b) Birth weight < 1.5 kgs.
c) Hyperbilirubinemia > 20mg/dl.
d) Moderate to severe birth asphyxia.
e) Maternal or neonatal history of ototoxic drug intake.
f) Documentary evidence of intracranial infections in the
past.
g) Family history of childhood hearing impairment.
h) Consanguineous marriage.
Exclusion criteria
a) Known case of seizure disorders where BERA cannot be
interpreted
b) Atresia or stenosis of external ear canal of both ears.
c) Patients not giving consent for BERA.
Parameter studied
BERA threshold for each ear with absolute latencies of wave I, II, III, IV and V waves interpeak latencies (IPL) of I-III, I-V and III-V and amplitude ratio V/I were considered from the recordings of high risk children.
Procedure
It was performed in dust free, soundproof, air-conditioned room free from electromagnetic disturbances. Syrup Pedichlor (25 mg/kg body wt.) was given to sedate the baby half an hour before procedure. After cleaning forehead, vertex and both mastoid regions with Nuprep (skin prep gel), surface electrodes were placed at the vertex, both mastoids and forehead (ground) and subject was tested in sleeping state with neck slightly flexed to minimize any myogenic activity. Headphone (TDH-39) was held against the ear of baby taking care that external auditory canal does not collapse. 2000/4000 clicks at a rate of 11.1/sec was given and the graphs was recorded on BERA machine Labat Epic- Plus.
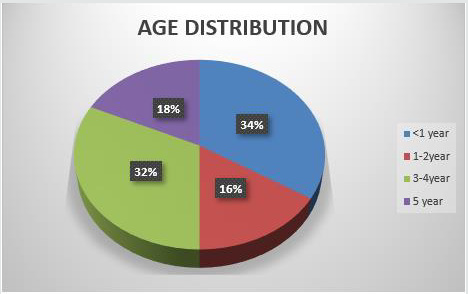
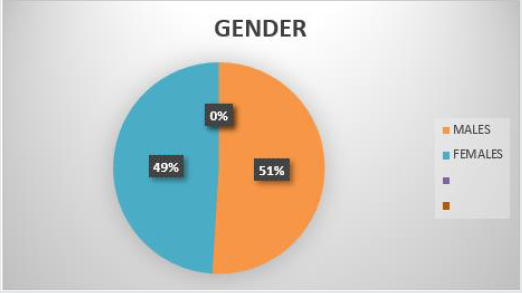
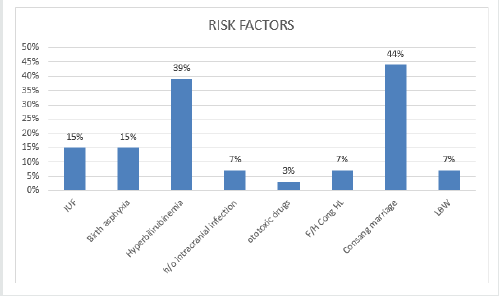
Results
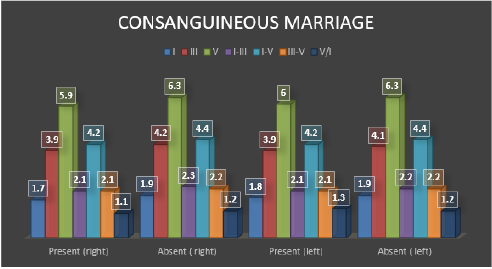
In this study 34% were in the age group <1 year. 51% were males and 49% were females. Almost equal number of males and females. In the study 15% had intrauterine infections, out of 15 subjects, 7 of them had CMV and 8 of them had Rubella. 39% had Hyperbilirubinemia, 44% had consanguineous marriage, of them 18 had 2nd degree marriage and 26 had 3rd degree marriage. There was significant difference in mean BERA parameters (V(dB) Threshold, III, V, I-III, I-V, III-V between those with and without hyperbilirubinemia. The above said parameters were significantly high among those with hyperbilirubinemia in right and left ear. There was Significant difference in mean V(dB) Threshold, III, V and I-V between those with and without H/o Consanguineous Marriage in Right ear. There was significant difference in mean V (dB) Threshold, V b/w those with and without H/o Consanguineous Marriage in Left ear. Those with Consanguineous Marriage, majority had mild (35.7%) hearing loss (Figures 4 & 5). In this study there was statistically significant difference between wave V threshold and high-risk factors consanguineous marriage and hyperbilirubinemia. There was no significant difference in mean BERA parameters between those with and without intrauterine infections, low birth weight, intrauterine infections, h/o intracranial infections, h/o ototoxic drug intake, family h/o congenital hearing loss and birth asphyxia in both right and left ear. 26 out 44 children with history of consanguineous marriage had hearing loss out of which 4 were unilateral with mild hearing loss. 34 out of 39 children with hyperbilirubinemia as a risk factor had hearing loss with one child having unilateral hearing loss.
Figure 4: Bar diagram showing Comparison of BERA parameters with respect to presence and absence of hyperbilirubinemia in Right and Left ear.
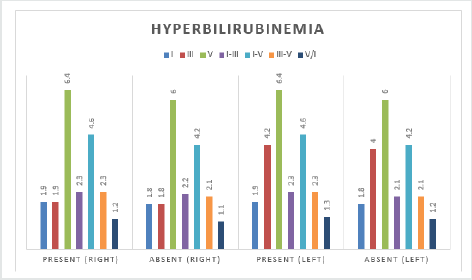
Figure 5: Bar diagram showing Comparison of BERA parameters with respect to presence and absence of consanguineous Marriage in Right and Left ear.
Discussion
Early detection of hearing loss and intervention is very
important for the development of normal speech and language.
Majority of children with hearing loss belong to age group 1-5 years
between which most of the speech and language development
occurs.4 Interventions usually vary from sign language to cochlear
implantation. Brainstem evoked response audiometry although
more time-consuming, is an accurate and reliable test for early
detection of neural conduction abnormalities in the auditory
pathway from the cochlea till the brainstem. The reported
sensitivity of the BERA for hearing assessment was 100% and
specificity around 86% [5]. Earlier perinatal causes like birth
asphyxia, hyperbilirubinemia, and intrauterine infections were
on the rise but recently inherited causes are on the rise especially
in developing countries like India. This is probably due to better
treatment facilities and referral centers available. In our study the
most common risk factor is shown to be consanguineous marriage
showing inherited causes were on the rise. Abnormality at the level
of cochlear nucleus and brainstem due to inheritance of abnormal
genes. This data is consistent with studies by Ramanathan [4] and
Mallikarjun [6] where inherited causes were on the rise. Health
education is of prime importance to increase awareness of the
detrimental health effects of consanguineous marriage.
The next most common risk factor was found to be
hyperbilirubinemia having Wave V absolute latency was increased
in both the ears and also interpeak latency I-V [7]. This indicates
that raised bilirubin levels is a important risk factor for detecting
hearing loss.8 In most infants with raised bilirubin levels the
values reverted back to normal after treatment indicating that
it is a reversible cause and prompt treatment is required. This is
similar to a study by Pramod Sharma [7] and by other authors
[8-10] in which there was statistically significant correlation in prolongation of latency and the interpeak latencies with serum
bilirubin levels more than 25 mg%. Follow up of infants with raised
bilirubin levels having hearing loss is required. Children with birth
asphyxia could have hearing loss due to the depressed end cochlear
potential induced by hypoxia and acidosis causing the involvement
of cochlea or cochlear nerve showing dysfunction in the peripheral
auditory process [11,12]. A definitive conclusion cannot be made
out regarding the outcome of the study, but it does suggest that
all high-risk children will benefit from early detection of hearing
loss and rehabilitation through BERA. High risk children should be
screened in hospital NICUs, prior to discharge from the hospital
and immunization clinics particularly around 6 months of age or
below one year using BERA for timely intervention to avoid delay in
speech and language development. A national program dedicated
to detecting early hearing loss would help reducing the burden of
handicap by avoiding delay in intellectual development of the child.
Brainstem evoked response audiometry though expensive is a
safe and accurate procedure to ascertain whether the hearing loss
can benefit through common rehabilitative measures like hearing
aids or not. Infants with abnormal BERA recordings should be
rescreened within 3 months and several times within the first year.
If abnormal responses persist immediate intervention to develop
speech and language should be undertaken.
Conclusion
From our study we can thus conclude that among the high-risk factors, consanguineous marriage seems to be the most common factor causing hearing loss in children. This factor being is a preventable cause, as compared to others, by premarital genetic counseling and health education in lower socioeconomic groups. The next most common factor is shown to be hyperbilirubinemia. This is proven to be a reversible cause of hearing loss according to some studies. Therefore, early detection treatment and follow up is very important in such children. Almost all of the children with a family history of hearing loss had mild to moderate hearing loss suggesting inheritance of abnormal proteins through genes but the sample size for the same was less to derive any significant correlation. BERA was found to be a useful, accurate tool to detect the type of hearing loss and the site of defect in auditory transmission of sound. This aids in planning the mode of intervention for early rehabilitation for speech and language development.
References
- Biswas A (2002) Brainstem evoked response audiometry. In: clinical Audio vestibulometry. 3rd Ed, Mumbai, India p. 68 - 88.
- Ballenger JJ, Snow JB (1996) Diagnostic Audiology and Hearing aids. In: Otorhinolaryngology Head and Neck surgery. 15th William and Wilkins p. 953-973.
- Flint PW, Haughey BH, Lund VJ, Niparko JK, Richardson MA, et al. (2015) Electrophysiologic assessment of hearing. In: Cummings Otolaryngology Head and Neck surgery. 6th Ed, Philadelphia, USA Elsevier p. 2071-2082.
- Thirunavukarasu R, Balasubramaniam G, Kalyanasundaram R, Narendran G, Sridhar S (2015) A study of brainstem evoked response audiometry in high-risk infants and children under 10 years of age. Indian Journal of Otology 21(2): 134.
- Sharma B, Shrivastava R, Shrivastava A (2016) Brainstem evoked response audiometry in high risk infants. J Evolution Med Dent Sci 5(39): 2463- 2466.
- Patil M, Handi P, Prasenkumar K, Gouripur K (2018) Objective screening of hearing impairment using brainstem evoked response audiometry in children below 5 years of age and assessing the highrisk factors. International Journal of Otorhinolaryngology and Head and Neck Surgery 4(4): 923.
- Sharma P, Chhangani N, Meena K, Jora R, Sharma N, et al. (2006) Brainstem evoked response audiometry (BAER) in neonates with hyperbilirubinemia. The Indian Journal of Pediatrics 73(5): 413-416.
- Silva DPC, Martim RHG (2009) Analysis of transient otoacoustic emissions and brinstem evoked auditory potentials in neonates with hyperbilirubinemia. Braz J otorhinolaryngol 75(3): 381-386.
- Sharma R, Grover N, Shankhyan N, Sharma ML (2006) Auditory brainstem responses in neonatal hyperbilirubinemia and effect of therapy. Indian J otolaryngol Head Neck surgery 58(4): 340-342.
- Bluestone CD, Stool SE, Alper CM, Arjmand EM, Casselbrant ML, et al. (2003) Ear and Related structures. In: Paediatric otolaryngology, 4th Ed, Saunders, Elsevier 779-807.
- Mishra PK, Katiyar CP, Kapoor RK, Shukla R, Malik GK, et al. (1997) Brainstem auditory evoked response in neonates with birth asphyxia. Indian Pediatrics 34: 199-205.
- Streletz LJ, Graziani LJ, Branca PA, Desai HJ, Travis SF, et al. (1986) Brainstem auditory evoked potentials in full term and preterm newborns with hyperbilirubinemia and hypoxemia. Neuro pediatrics 17(2): 66-71.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...