Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Platelet Mass Index as A New Factor in Tinnitus Etiology Volume 6 - Issue 4
Ahmet Doblan*
- 1Department of Otorhinolaryngology, SBÜ Mehmet Akif Inan Training and Research Hospital, Turkey
Received: May 15, 2021 Published: May 28, 2021
Corresponding author: Ahmet Doblan, Member Faculty, MD, ENT-HNS Specialist, SBÜ Mehmet Akif İnan Training and Research Hospital, Şanlıurfa, Turkey
DOI: 10.32474/SJO.2021.06.000243
Abstract
Introduction: Although there are numerous studies on the etiology and treatment of tinnitus, most have not provided a definitive conclusion. Vascular and hematological abnormalities play an important role in the etiology of tinnitus. In this study, we aimed to evaluate the usability of the platelet mass index as a new inflammatory marker in patients with tinnitus.
Material and Method: The detailed medical records (examination notes, drug use, radiological evaluations, audiological evaluations, and previous vascular-cardiac-autological surgical procedures) of 1,079 tinnitus patients presenting to our clinic between January 2019 and May 2020 were examined, and a retrospective hemogram evaluation was performed in 176 patients meeting the inclusion criteria in tinnitus group. As the control group, 190 people were selected from individuals that presented to the outpatient clinic without otologic complaints. Age, gender, erythrocyte (RBC), hemoglobin (HGB), neutrophil (NEU), lymphocyte (LYM), platelet (PLT) and mean platelet volume (MPV) were examined, and the neutrophil-lymphocyte ratio (NLR), plateletlymphocyte ratio (PLR) and platelet mass index (PMI) were calculated, and the results were compared between the tinnitus and control groups.
Statistical analysis and results: There were no statistically significant difference between the control and tinnitus groups in terms of mean age, gender, and RBC, NEU, LYM, PLR and NLR levels (p>0.05 for all). The HGB and MPV levels were significantly higher (p<0.001 for both) and the PLT level was significantly lower (p = 0.033) in the tinnitus group compared to the control group.
In addition, the PMI value of the tinnitus group was statistically significantly higher than that of the control group (p<0.001).
Discussion and conclusion: This study was the first to investigate PMI in tinnitus patients, and this index was found to be higher in this patient population. This supports the idea that PMI can be used as an inflammatory marker in tinnitus. PMI can reveal platelet functions more clearly since it provides the opportunity to simultaneously evaluate the volume and number of platelets. However, since the relationship of PMI with tinnitus severity was not examined in this study, further detailed studies are needed on this subject.
Keywords:Tinnitus; platelet mass index; inflammatory marker; mean platelet volume; platelet
Introduction
Tinnitus refers to hearing sounds of different frequencies and qualities emanating from the ear without the presence of any external stimulus [1]. It is a condition that affects a large number of patients in daily otorhinolaryngology practice. Although a prevalence of 10-15% has been reported in different series, this rate may exceed 30% in the population over 60 years of age [2]. Tinnitus can affect one ear or both ears. It is classified into two main groups as objective and subjective tinnitus. In objective tinnitus, the person who performs the test hears the sound together with the patient, and this is mostly caused by temporomandibular joint disorder, arteriovenous malformations, and spasm of the tensor tympani muscle [3]. In subjective tinnitus, the sound is only heard by the patient, and the test person does not hear it. Subjective tinnitus may occur for many reasons such as hearing impairment, insomnia, drug use, depression, chronic diseases, anxiety, and difficulty in concentration, and it has a negative effect on the quality of life of patients [4]. Subjective and objective tinnitus may have various frequencies and qualities, as well as varying severity. Although there are many studies on tinnitus etiology and treatment, most have not provided a definitive conclusion However, it has been shown that despite the majority of tinnitus sounds being considered to originate from the cochlea, tinnitus continues even after the completely excision of the auditory nerve [5]. This situation may be related to tinnitus originating not only from the cochlea but also from all auditory pathways and the formation of some inappropriate neural plasticities in the central nervous system.
Although these changes in the central nervous system are both structural and functional, they may occur not only in auditory pathways but also in different parts of the brain [6,7]. When tinnitus patients are evaluated, vascular and hematological abnormalities can be defined as important etiological reasons. These hematological and vascular causes may be effective in the development of structural and functional problems in the central nervous system and cochlea. Despite the availability of many studies on the vascular and hematological dimensions of tinnitus, as in the case of sudden hearing loss and facial paralysis, to date, no clear result has been obtained. It has been shown that among possible hematological reasons, the neutrophil-lymphocyte ratio and platelet lymphocyte ratio are related to the inflammatory process and some thrombotic events [8]. However, considering that the main factor that constitutes a thrombotic risk is platelets, they should be examined in more detail. At this point, the importance of the platelet mass index (PMI) comes to the fore due to its high activity in such thrombotic events at the microvascular level. This is an important issue, especially in organs with endarteria, such as the ear cochlea. Any microvascular thrombotic event caused by platelets in these endarteria leads to serious dysfunction in the organ. However, this cannot always be revealed by angiographic methods, and there is the possibility of temporary ischemic attacks and tissue injury that should not be overlooked. It has been emphasized in the literature that the increase in mean platelet volume (MPV) is effective in inflammatory processes and increased MPV rates are directly related to the activation of platelets [9]. Although MPV is a parameter that has been investigated before, its evaluation alone may not be reliable enough since the number of platelets is at least as important as its volume. Therefore, in the current study, we aimed to evaluate the usability of PMI as a new inflammatory marker in tinnitus patients. To the best of our knowledge, this is the first study to investigate the importance of PMI in patients with tinnitus.
Material and Method
After obtaining the approval of the ethics committee of Harran University (dated 29.06.2020 and numbered HRU/20.12.09), the detailed medical records of 1,079 tinnitus patients that presented to our clinic between January 2019 and May 2020 were evaluated. Examination notes, drug use, radiological evaluations, audiogram evaluations, hemogram parameters, vascular surgery records for cardiac region and otologic surgery records for the head and neck region, chronic disease records, and otologic disease records were evaluated for all patients. The inclusion criteria for the tinnitus group were as follows: age between 18 and 60 years, unilateral or bilateral chronic subjective tinnitus (continuing for at least three months despite medical treatment), normal ranges of hemogram and audiological test values in both ears, and symmetry of the two ears. A total of 176 patients that did not meet the specified exclusion criteria were included in the tinnitus group. As the control group, 190 people were selected from individuals that presented to the outpatient clinic without otologic complaints, underwent audiogram examinations and hemogram tests, and had no history of temporary (lasting for less than two weeks) or permanent tinnitus. Patients with cancer, chronic diseases, history of vascular surgery in the cardiac or head and neck region (by-pass, carotid artery surgery, etc.) or medical records of platelet dysfunction were excluded in order to reveal the independent role of PMI in identifying tinnitus. Further excluded from the study were patients with acute inflammation or infection, diabetes mellitus, systemic hypertension, hyperlipidemia, coronary artery disease, chronic liver disease, acute or chronic renal failure, chronic obstructive pulmonary disease, psychiatric disease history, connective tissue disease, inflammatory bowel disease, acoustic trauma history, noise-related hearing loss or family history of hearing loss; active smokers; patients with a hearing loss of 20 dB (this value was considered to be the normal hearing value) or above and an asymmetrical hearing threshold of >5dB between the two ears due to any otologic disease such as chronic otitis media, otosclerosis and Meniere’s disease; and those with a history of otologic surgery. The same inclusion and exclusion criteria were applied to both groups. For the patients included in the sample based on these criteria, demographic data such as age and gender were obtained, and a hemogram examination was undertaken to evaluate the levels of erythrocyte, hemoglobin, neutrophil, lymphocyte, platelet, and MPV. Furthermore, the neutrophil-lymphocyte ratio (NLR), platelet-lymphocyte ratio (PLR) and PMI (number of platelets x MPV / 1,000) were calculated in all patients, and the results were compared between the tinnitus and control groups.
Statistical analysis
Data analysis was performed using IBM SPSS Statistics version 17.0 software (IBM Corporation, Armonk, NY, USA). Whether the continuous variables were normally distributed was determined using the Kolmogorov-Smirnov test. The assumption of the homogeneity of variances was examined with the Levene test. Descriptive statistics for continuous variables were expressed as mean ± standard deviation or median values (25th–75th percentiles) where appropriate. Number of cases and percentages were used for categorical data. While the mean differences between the groups were compared using Student’s t-test, the Mann Whitney U test was applied for the comparisons of continuous variables that did not meet parametrical test assumptions. Categorical data were analyzed using Pearson’s χ2 test. The optimal cut-off values of laboratory measurements to discriminate cases and controls were evaluated with the receiver operating characteristic (ROC) analysis that provided the maximum sum of sensitivity and specificity for the significant results. The sensitivity, specificity, positive and negative predictive values, and accuracy of PMI were also calculated. The independent statistically significant role of PMI in discriminating tinnitus patients from controls was evaluated with the multiple logistic regression analysis after the adjustment of age, gender, and hemoglobin levels. A p value of less than 0.05 was considered as statistically significant.
Results
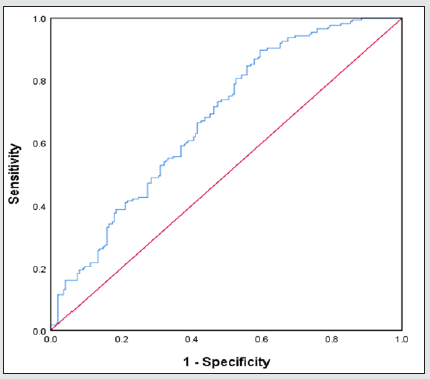
Table 1 presents the results of the comparisons between the tinnitus and control groups in terms of demographic characteristics and laboratory measurements. The PMI level of the tinnitus group was statistically significantly higher than that of the control group (p < 0.0011). Table 2 shows the results of the ROC analysis performed to evaluate whether PMI, PLR and NLR were statistically significant markers in distinguishing the tinnitus patients from the controls. The area under the ROC curve (AUC) for the PMI measurements was found to be statistically significant in differentiating between the tinnitus and control groups [AUC = 0.678, 95% confidence interval (CI): 0.623-0.732, p < 0.001] (Figure 1). The best cut-off value for PMI was 1.6452, at which PMI had a sensitivity of 89.8%, specificity of 68.1%, positive predictive value of 58.3%, negative predictive value of 81.1%, and diagnostic accuracy of 64.2%. According to the multiple logistic regression analysis, PMI was also an independent factor that discriminated between the tinnitus cases and controls after the data were adjusted for age, gender, and hemoglobin level (OR = 6.608, 95% CI: 3.661-11.928, p < 0.001).
Table 1: Demographical characteristics and laboratory measurements of the study groups.
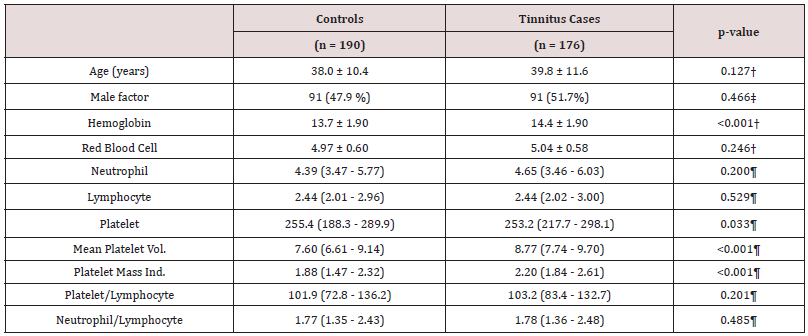
† Student’s t-test, ‡ Pearson’s χ2 test, ¶ Mann-Whitney U test
Table 2: The results of the ROC analysis for laboratory measurements to discriminate between the control and tinnitus cases.
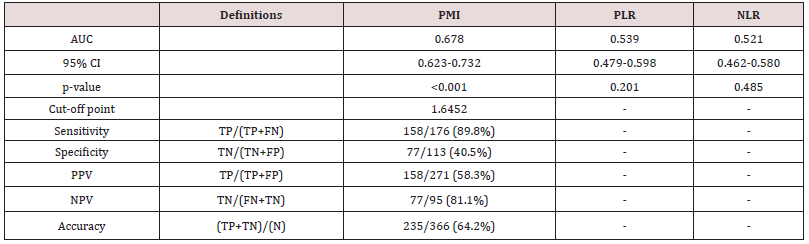
AUC: Area under the curve, CI: Confidence interval, TP: True positive, FN: False negative, TN: True negative, FP: False positive, PPV: Positive predictive value, NPV: Negative predictive value, PMI: Platelet Mass Index, PLR: Platelet/Lymphocyte Ratio, NLR: Neutrophil/Lymphocyte Ratio
Discussion
Tinnitus is a condition characterized by damage to auditory pathways through various mechanisms, but its etiology and treatment have not yet been clearly demonstrated. Vascular and hematological abnormalities and inflammatory processes are among the known causes of tinnitus. It is known that especially MPV is directly related to inflammatory processes and functions of platelets [9]. Therefore, the various effects of mediators secreted by platelets on the tissue, especially neovascularization should not be overlooked. Evaluating platelets based only on their number without the assessment of their function will result in limitations in the interpretation of results. MPV is an inexpensive and very practical parameter that can be measured in routine complete blood count analysis. Factors such as age, obesity, hyperlipidemia, diabetes, smoking, and hypertension may affect this platelet parameter [9]. However, it is important to know that the significant difference in MPV may also be due to pre-measurement factors including blood tube selection, processing, and equipment used [10]. Increased MPV means an increase in granulocytes in the platelet, which is directly related to the platelet activity. In other words, large platelets are more active than small platelets [11]. At this point, although the volumetric size of platelets is important, their number is also important. Ischemia that occurs in tissues causes an inflammatory process to begin. In ischemic tissues, many pro-inflammatory cytokines, mainly TNF-alpha, are released in the affected tissue [12]. It is considered that an ischemic state in auditory pathways caused by vascular pathologies may trigger a mechanism that leads to an increase in MPV. Increased MPV or platelet count naturally results in an increase in PMI. In a study by Kemal et al., it was observed that MPV was increased in tinnitus patients and tinnitus might occur as a result of increased MPV causing the formation of microvascular thrombosis in the vessels of the auditory tract and thereby leading to hypoperfusion-ischemia [13]. However, we consider that it would not be appropriate to implicate MPV alone in all these mechanisms. There are studies in the literature that support this idea. Yüksel et al. reported that MPV was lower but the platelet count was higher in tinnitus patients compared to the control group [14].
Overall platelet function can be more accurately reflected by platelet mass compared to platelet count alone. This was first demonstrated by Gerday et al., who reported that the use of platelet mass resulted in a reduced number of platelet transfusions [15]. To the best of our knowledge, our study is the first to explore the relationship between PMI and tinnitus in the literature. As explained above, as an index evaluating the number and volume of platelets together, PMI can be more useful in explaining the mechanism of tinnitus rather than the evaluation of MPV alone. PMI is associated with platelet functionality because larger platelets are enzymatically more active than small platelets. Increasing the number of active platelets means an increase in PMI, which supports our hypothesis. Recently, some studies aiming to reduce unnecessary transfusions have suggested using platelet mass instead of platelet count as an indicator of the need for platelet transfusion [15,16]. Okur et al. reported that premature babies with bronchopulmonary dysplasia, intraventricular bleeding, necrotizing enterocolitis, retinopathy of prematurity, and sepsis had lower PMI in the early period compared to those without these neonatal morbidities [17] Although the differences in MPV were not significant, the authors also showed that PMI was significantly lower in these neonatal complications [17]. This situation may also be valid for tinnitus patients. Based on these data, we consider that PMI may be a better marker than MPV in some cases. In our study, we found that PMI was statistically significantly higher in patients with tinnitus, but larger series are needed to prove the superiority of PMI over MPV as an inflammatory marker in this condition. Based on the results obtained from our study, we consider that PMI may be a more sensitive parameter as a clinical marker compared to MPV in tinnitus patients. The significant difference in PMI revealed by the current study may guide further research aimed at revealing the relationship between tinnitus severity and PMI.
Limitations
A major limitation of the study concerned its retrospective nature, which led to the necessity of limiting the number of patients and applying a wide a range of exclusion criteria. As a natural consequence of this situation, our case group was limited. In addition, no scoring was undertaken to evaluate tinnitus severity; thus, there is a need for further studies to be conducted in light of our findings to provide additional data in this respect. The severity of tinnitus was not included in the scope of our study, and therefore we did not administer any related questionnaire (e.g., Tinnitus Handicap Inventory). Our concern here is that we have no evidence as to whether vascular factors that may affect tinnitus cause lowor high-intensity tinnitus. In conclusion, the hemoglobin and MPV values were found to be higher in the tinnitus group compared to the control group. Furthermore, PMI, which was investigated for the first time in tinnitus patients, was also significantly higher, contributing to the main purpose of this study. Therefore, we consider that PMI can be used as a new clinical marker in tinnitus patients, and it can also be an appropriate parameter that could provide significant results in many otorhinolaryngologic diseases and conditions, especially Bell’s palsy, vestibular neuritis, nasal polyps and allergic rhinitis, and sudden sensorineural hearing loss.
Conflict of Interest
The authors have no conflicts of interest to declare.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and international guides on clinical research. Ethics committee approval was obtained from Harran University Faculty of Medicine 29.06.2020 date and numbered HRU/20.12.09.
Author contributions
All authors contributed to the manuscript.
References
- Wegger M, Ovesen T, Larsen DG (2017) Acoustic coordinated reset neuromodulation: a systematic review of a novel therapy for tinnitus. Frontiers in Neurology 8: 36.
- Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, et al. (2014) Clinical practice guideline: tinnitus. Otolaryngology–Head and Neck Surgery 151(2_suppl): S1-S40.
- Bauer CA (2018) Tinnitus. New England Journal of Medicine 378(13): 1224-1231.
- Zeman F, Koller M, Langguth B, Landgrebe M (2014) Which tinnitus-related aspects are relevant for quality of life and depression: results from a large international multicentre sample? Health and Quality of Life Outcomes 12(1): 7.
- Kohno M, Shinogami M, Yoneyama H, Nagata O, Sora S, et al. (2014) Prognosis of tinnitus after acoustic neuroma surgery—surgical management of postoperative tinnitus. World Neurosurgery 81(2): 357-367.
- Husain FT, Schmidt SA (2014) Using resting state functional connectivity to unravel networks of tinnitus. Hearing research 307: 153-162.
- Adjamian P, Sereda M, Hall DA (2009) The mechanisms of tinnitus: perspectives from human functional neuroimaging. Hearing research 253(1-2): 15-31.
- Ferroni P, Riondino S, Formica V, Cereda V, Tosetto L, et al. (2015) Venous thromboembolism risk prediction in ambulatory cancer patients: clinical significance of neutrophil/lymphocyte ratio and platelet/lymphocyte ratio. International Journal of Cancer 136(5): 1234-1240.
- Karli R, Alacam H, Unal R, Kucuk H, Aksoy A, et al. (2013) Mean platelet volume: is it a predictive parameter in the diagnosis of sudden sensorineural hearing loss? Indian Journal of Otolaryngology and Head & Neck Surgery 65(4): 350-353.
- Noris P, Melazzini F, Balduini CL (2016) New roles for mean platelet volume measurement in the clinical practice? Platelets 27(7): 607-612.
- Vizioli L, Muscari S, Muscari A (2009) The relationship of mean platelet volume with the risk and prognosis of cardiovascular diseases. International journal of clinical practice 63(10): 1509-1515.
- Haider HF, Ribeiro SF, Martins C, Ribeiro D, Trigueiros N, et al (2020) Tinnitus, hearing loss and inflammatory processes in an older Portuguese population 59(5): 323-332.
- Kemal O, Müderris T, Basar F, Kutlar G, Gül F (2016) Prognostic value of mean platelet volume on tinnitus. The Journal of laryngology and otology 130(2): 162.
- Yüksel F, Karatas D JJo CS (2016) Can platelet indices be new biomarkers for subjective tinnitus? J Cranifac Surg 27(5): 420-424.
- Gerday E, Baer VL, Lambert DK, Paul DA, Sola‐Visner MC, et al. (2009) Testing platelet mass versus platelet count to guide platelet transfusions in the neonatal intensive care unit. Transfusion 49(10): 2034-2039.
- Zisk JL, Mackley A, Clearly G, Chang E, Christensen RD, et al. (2014) Transfusing neonates based on platelet count vs. platelet mass: a randomized feasibility-pilot study. Platelets 25(7): 513-516.
- Okur N, Buyuktiryaki M, Uras N, Oncel MY, Ertekin O, et al. (2016) Platelet mass index in very preterm infants: can it be used as a parameter for neonatal morbidities? The Journal of Maternal-Fetal & Neonatal Medicine 29(19): 3218-3222.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...