Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2690-5752) 
Oral Health Status of Adults with Disability related to Body Structures and Activities in Rendovah District, Solomon Islands Volume 10 - Issue 1
Rayboy T Seleso Jr1, Jayantha Weerasinghe2, Ellison Vane3, Sharjeel Chaudhry4* and Zarmina Ehtesham5
- 1Department of Oral Health College of Medicine, Nursing and Health Sciences Fiji National University, Fiji
- 2Professor in Oral & Maxillofacial Surgery, Fiji
- 3Head of Population Oral Health & Research Unit Dental Department, National Referral Hospital Solomon Islands, Fiji
- 4Department of Oral Health College of Medicine, Dow University of Health Sciences, Pakistan
- 5Department of Oral Health College of Medicine, Hamdard University, Pakistan
Received: March 27, 2023; Published: April 21, 2023
Corresponding author: Sharjeel Chaudhry, Department of Oral Health College of Medicine, Dow University of Health Sciences, Pakistan
DOI: 10.32474/JAAS.2023.10.000326
Abstract
This article provides an overview of the population and healthcare system in the Solomon Islands, with a focus on the Rendovah District in the Western Province. The majority of the population lives in rural areas, with limited access to healthcare services. Malaria and non-communicable diseases are the leading causes of mortality and morbidity. The article also highlights the high proportion of disability in the country, with common types including senile debility, lameness, deafness, and blindness. The smallest provinces have the lowest proportion of disability, while Isabel, Makira-Ulaw casa, and Central provinces have the highest.
Introduction
Background Information
Stretched from the eastern end of Papua New Guinea to the northern most islands of Vanuatu [1], Solomon Islands comprised of over 900 coral atolls [2]. There are nine provinces that make up Solomon Islands, a Nation. The country’s population in the year 2009 census was estimated at 515, 870 growing at a rate of 2.3% per annum. The age group ranges from 15-59 years, with only 5% aged 60 years and older [2]. The majority (80.3%) of the country’s population lives in the rural areas than in the urban centres (19.7%) [1], there is a 20% rate of urbanization [3]. Rendovah District is an island district in the Western part of the Solomon Islands. It is one of the nine main islands that made tup the Western province of the Solomon Islands. Western Province is the third most populated province in Solomon Islands1 and is situated at the eastern end of Papua New Guinea. The nearest hospital that provides dental services to the district is thirty minutes boat ride powered by outboard motor engine. And the cost of travel will be about SBD $80 return. Subsistence farming and fishing are the main source of income for most of the people in the district. However, some people are very artistic in carving and have been their source of income. The carvings are sold to tourists and locals. The health care services delivery to the rural populace stagnated due to the influx of people into the urban center2 in recent years. Although it has declined, malaria is still the leading causes of mortality and morbidity in children, while non-communicable diseases lead in adults [2]. Limited resources are a major drawback in the country’s health care system delivery, despite the country’s transitional epidemiological phase, where the country has to deal with both controlling infectious and an increasing incidence of non-communicable diseases [2].
Disability in Solomon Islands
The year 2009 census shows that 14% of the total population has some form of disability. Approximately half of the total population aged 55-59 years has disabilities. Moreover, the proportion of disability increased rapidly at the age of 35-39 years [1]. The census report highlighted that one person can have more than one disabilities (multiple disabilities) [1]. According to the 2009 Census, common types of disabilities in adults in Solomon Island were recorded as Senile debility (3,293 cases), lameness (2,975 cases), deafness (1,398 cases) and blindness (907 cases). Isabel, Makira-Ulaw casa and Central provinces have the highest proportion of disability, while the smallest Renbell, Honiara and Malaita Provinces have the lowest proportion [1].
Health Care Delivery in Solomon Island
Almost all of the health care services in Solomon Island are provided by the government through the Ministry of Health and Medical Services (MHMS). The MHMS is a funder, regulator and provider of health care services [2] and is based on public health care approach4 and is available to all Solomon Islanders. All the nine Provinces, except the Polynesian dominant province of Renbell have Provincial hospitals. Guadalcanal province, which hosted the country’s capital city of Honiara, is serviced by the National Referral Hospital [2]. Moreover, there are other health facilities provided by the government available in the entire province and these include Nurse Aid Posts, Rural Health Clinics, Area Health Centres and the National Referral Hospitals. The presence of these health care facilities is based on the distribution of population of each provinces [2].
The Nurse Aid Posts (187) provide very basic primary health care, public health and prevention services; they are commonly situated in the remote parts of the country. Rural health Clinics offer the next level of health care, supervise the Nurse Aid posts within the same area and arrange outreach activities. There are 38 Area Health Centres that provide inpatient, outpatient, outreach care and public health services. It also offers specific birth facilities, administrative space and staff housing. Basic dental treatment is provided in the Area Health Centres, these include tooth extractions, fillings and provision of dentures. The provincial hospitals (7) are always the highest health care provider to those residing in the remote areas. The only National Referral Hospital offers a full range of secondary clinical care, operating theatre and emergency department. Clinical cases that cannot be dealt within the facilities in the Referral hospital are referred mainly to St Vincent’s Hospital in Sydney, Australia. The treatments are free of charge and the airfares are paid by the Solomon Island government based on the 1993 arrangement between the hospital and the Solomon Island government. Few paediatrics cases are sent to Randwick Children’s Hospital and to Greenlane Hospital in New Zealand [2]. Apart from the seven (7) public hospitals provided by the government, there are three privately owned by non- government organizations and Church groups.
Oral Health issues in Solomon Island
Dental care treatment provided ranges from simple tooth extractions and fillings in the Area Health Centres to minor oral surgical procedures and complicated restorative procedures such as root canal treatment, crown and bridge etc. in the National Referral Hospital Dental department. Factors influencing oral health of the general population include access to health care facilities, cost of care, lack of oral health promoters (staff) [2] and betel nut chewing habits. There are very limited Oral health professional and specialists in Solomon Island [3-8]. In 2005 a total of 52 dentists were recorded and the ratio per 1,000 population was 0.102. Dental caries and periodontal diseases are the two most common dental health problems of adults in Solomon Island. Most patients present to any dental clinic in the country due to pain. In general adults suffering from periodontal diseases do not visit a dental facility due to lack of knowledge of the disease. Tooth loss, dental caries, periodontal diseases, xerostomia and precancer/cancer are some of the common oral health problems in adults [8]. According to a study [6] in 2000, there is a mark increased prevalence of Oral cancer in adults in Solomon Island.
Statement of the Problem
Adults with disabilities may have poor oral health status due to lack of physical accessibility, transportation, and cost of treatment, fear/anxiety and lack of knowledge in oral hygiene in Pacific Island Nation. The same may prevail in the Solomon Islands due to its geographical location in the Pacific region, weak economic status and lack of Oral health knowledge among the general populace. The findings of this study will be helpful in planning health care delivery in Solomon Islands in future especially to the special need patients.
Literature Review
The International Classification of Functioning, Disability and Health (ICF) defined disability as impairment, activity limitations and participation restrictions7. ICF estimates that 15% of the world’s population has some form of disability and between 110 million to 190 million adults worldwide have significant difficulties in functioning7. This is due exclusively to ageing and increased chronic health conditions7. In support of this, a study9 in 2006 shows that an increase population of male and female with intellectual and other developmental disabilities is reaching older age. Reports have suggested that there is high prevalence of disability in female than in male, however the pattern of disability varies between countries. This may be influenced by trends in health conditions and trends in environmental and other factors such as road traffic crashes, natural disasters, conflict, diet and substance abuse [7]. Robust evidence suggests that people with disabilities have poor health, less education and low socioeconomic status. Despite the recent recommendation by World Health Organization (WHO) for mainstream programmes to meet the disabled individu al’s ordinary needs [7], they continue to suffer oral health diseases or conditions.
Mental disability
Numerous studies have established that adults with some sort of mental or cognitive disabilities have poor oral health [10-13]. A longitudinal study [14] supports that person with mild intellectual disability experience more caries than that other objects in the study. Moreover, Chalmers et al. [15] states that patients with dementia had higher experiences of oral diseases and conditions and that the higher experience is associated with the severity of dementia. There is also evidence that they have numerous unmet dental needs [16]. Paul [17] further highlighted that certain oral conditions appear more often in person with specific disabilities partly because of the disability itself, but also because of behaviour patterns associated with the disability.
Hearing Impairments
Hearing impairment also has oral health impact on adults. Shannon and Santhosh et al.agrees that adults with hearing impairment have poor oral health [18,19]. A study in children also suggests that hearing impaired patients tend to have poor oral health and high DMFT [20]. Lack of communication is the main issue that lead to poor oral health among hearing impaired patients [19]. Shannon [18] suggests that good sufficient communication should be established between oral health care provider and the patient, this includes patient wearing hearing aid, dentist speak directly without wearing musk, reduced background noise, provide written instructions and speak when the patient is looking. Moreover, Sandeep et al. [21] discovered that visual instruction is an effective medium to oral health education in hearing impaired patient.
Visual Impairment
Kandelman and et al. [22] found that visual impairment affects adult patient’s ability to maintain oral hygiene and recognize signs of oral diseases such as caries and periodontal disease. A pilot study further states that they are not in a position to detect and recognize early signs of oral diseases [23]. Thus they need supervision to achieve optimum oral health. Watson [24] further stress that developing oral health promotions that ensures patients with a visual impairment have appropriate information regarding oral hygiene and its provision is of paramount importance.
Physical Disability
On the other hand, adults with physical disabilities cannot care for their oral health due to paralysis [25], the main drawback in maintaining good oral health. This was confirmed by Neuman [26]. Also a survey [27] in Southern Australia demonstrates that 76.3% of the adult population with physical and intellectual disabilities had caries experience (DMFT>0). In addition, 70% of Greek dentists interviewed states that treating a patient with physical and intellectual impairment demanded a lot of time and was hard to accomplish [28]. For these same reasons, Irish dentists suggested that additional fee were deemed necessary for the treatment of special need patients [29]. Thus, these special need patient might have higher experiences of poor oral hygiene. Other identified factors that contribute to poor oral health of adults with disabilities include fear and anxiety, financial constrain, physical barriers, lack of time and domiciliary equipment and transportations [30-34].
WHO-ICF International Classification of Functioning, Disability and Health
The ICF is a classification of health and health-related conditions for children and adults which was developed by the World Health Organization (WHO) and published in 2001 [35]. The WHO considers the ICF classification system as a partner to the ICD (International Classification of Diseases and Related Health Problems) system. Whereas the ICD classifies disease, the ICF looks at functioning. Therefore, the use of the two together would be beneficial. The ICF is not based on aetiology or “consequence of disease,” but as a component of health [36]. The ICF describes health and health related domains using standard language and recommends use of the same for the purposes including: collection of statistical data, clinical research, clinical use and social policy use.
Components of ICF
The ICF framework consists of two parts: Functioning and Disability and Contextual Factors. These parts are further broken down in the following manner.
Functioning and Disability includes
a) Body Functions and Structures - describes actual anatomy and physiology/psychology of the human body.
b) Activity and Participation - describes the person’s functional status, including communication, mobility, interpersonal interactions, self-care, learning, applying knowledge, etc.
Contextual Factors include.
a. Environmental Factors: Environmental factors are those that are not within the person’s control, such as family, work, government agencies, laws, and cultural beliefs.
b. Personal Factors: Personal factors include race, gender, age, educational level, coping styles, etc. Personal factors are not specifically coded in the ICF because of the wide variability among cultures.
Rendovah District, Solomon Islands
Rendovah island district has a total land area of 411.3sq.km with an average elevation of 30 meters. The 2009 Census estimates that the South Rendovah with 334 houses has a population of 2,477 while the North Rendovah with 451 houses has a population of 1,724. The map of Rendovah district (Figure 1) shows the villages scattered along the shoreline. There is no tar sealed road on this island district, neither public vehicle nor the main transport mode is used of boats. The PI was born and brought up in the village called Ughele in North Rendovah. Being brought up in a village in Rendovah district, The Principle Investigator has seen people having difficulty in accessing dental services. Due to lack of transportation and low socio- economic status, Moreover, most people don’t see the value of their teeth or their oral health in general. Thus, it is decided to carry out this research to gather, analyse and interpret data to show responsible authorities and stakeholders the urgent need to provide dental service. As advised by the DOHRC and CHREC and due to other constraints, the study will be conducted among the villages of the Northern region of the Rendovah island district. PI will be staying in his family house and reach the nearby villages on foot or by boat along the seashore. In addition, it would be easier for the Principle Investigator to approach the key stakeholders for this research project because of the familiarity of the geography of the district and people.
Aims & Objectives
The Aim of the study is to determine the Oral health status of non-institutionalized adults with disability related to body structures and activities in Rendovah District in Solomon Islands. The objectives of this study are:
a) To identify the common disabilities of adults related to body structures and activities in Rendovah District, Solomon Islands.
b) To determine the Oral health status of adults with disability related to body structures and activities in Rendovah District, Solomon Islands
Methodology
Study Type, Variables, Data Collection Technique
Study Type
This is a cross-sectional study carried out among non-institutionalized adults with disability. Considering factors such as constraints in conducting general clinical examination in a household environment, non-availability medical records and other logistics, this study concentrated only on adults with physical disability as explained in the ICF classification that may have direct or indirect relationship to maintenance of oral health.
Inclusion criteria
Adults with physical disability in relation to body structures and activities. This will include visible structural body abnormalities, vision, hearing, speech and activities of mobility and routine functions.
Exclusion criteria
Adults with other disabilities such as mental functions, other systems of the body, and environmental factors explained in the ICF classification. Severe disabilities that prevent proper oral examination and use of medications that have effects on oral health will also be exclusion criteria.
Data Collection Instruments
Tools used in the study are:
a) WHO Oral Health Assessment Form, 2013 to identify oral health parameters.
b) Instructor assisted questionnaire for Disabilities with questions extracted on disability in relation to body structures and activities from the WHO-ICF International Classification of Functioning, Disability and Health.
c) Basic Oral examination set: This includes dental mirror, WHO probe and explorer.
ICF Coding
ICF codes utilize an alphanumeric system to describe health and health-related domains, with the following letter codes:
a) b - Body functions
b) s - Body structures
c) d - Activities
Variables
This study has following variables:
Dependent Variables
a) Oral health parameters of the disabled adults
b) Disability features in relation to body structures and activities
Independent Variables
a. Age
b. Sex
c. Ethnicity
Data Collection Technique
Study Population
Adults with Disability related to Body Structures and Activities in Rendovah District, Solomon Islands. The study area of North Rendovah has an estimated total population of 1,724.
Data Collection
A study by Kuruvilla and Joseph37 in 1999 discussed the use of Rapid Rural Appraisal and House-to-House Survey as methods that could be used to comprehensively identify people with disability in a community. The first phase of the study will be conducted as a Rapid Rural Appraisal where the information about possible households of each village with disabilities will be obtained through various sources in the community such as village chiefs, headsmen, community health workers and community social workers. The information obtained will be mapped with the targeted houses marked and will be used for a subsequent phase: house-to-house survey. During the house visit, the Participant information sheet was issued to potential participants or care-giver, or family members and thorough explanations was provided in the local dialect by the principal researcher. Upon acceptance, the participants were given the consent form for written approval by themselves or by a third party.
Instructor assisted questionnaire for Disabilities.
The Instructor Assisted questionnaire for disabilities was completed by interview with participant in the presence of care-giver or a family member. As described earlier, this questionnaire was prepared to crudely assess the body structure (S), body functions (B) and activities (D). Original questions were extracted from the validated questionnaire recommended for surveys and the original codes will be used. As a final year BDS student the PI is capable of identifying gross abnormalities of the body as mentioned in the questionnaire while details of functions and activities could be obtained by questioning, hence this will be an instructor assisted questionnaire. The presence of Co-Supervisor will ensure the accuracy of the process.
Conduct of Oral Examination- WHO oral health assessment form
The WHO oral health assessment form was used to collect data. With the guidance of the co- investigator in Solomon Islands, who is an official of the MOH, access to sterilised instruments would be obtained from the nearby health facility. Participants were examined in their living premises in a suitable sitting position under natural light. Disposable gloves and pre-sterilised sets of basic dental instruments will be used for the Oral Examination. Used instruments were washed and cleaned soon after examination and returned to the health facility for re-sterilization.
Sampling
Convenience sampling technique will be employed in this study. A total sample of 50 adults with disabilities will be recruited to participate in this study.
Plan for Data Collection
The village nurse was consulted about any disabled adults in the village. The Principal investigator was accompanied by the co-supervisor during the data collection. Upon locating the disabled adults in the community, the participant information sheet was, either to the participant or the care-giver, depending on the level of education of the participant and care-giver. Thorough explanations were provided by the researcher in the local dialect. If the participant has agreed to take part in the study, an Oral examination was carried out using the modified WHO form.
Data Processing and Analysis
Microsoft excel 2013 was used to analyse the data.
Ethical Considerations
Approval was sought from the Department of Oral Health Research Committee and College Health Research and Ethics Committee and the National Health Research and Ethics committees of Solomon Islands. The final approval was obtained from the Rendovah Council of Chief to carry out the survey in Rendovah district, Solomon Islands. All data collection forms were coded and kept in a safe place for a period of seven years and then destroyed unless required by law. Participants in need of dental treatment were referred to an appropriate health facility. Informed written consent was obtained from participants and a third party consent (either a family member or a caregiver) was invited in the consent process as either a witness or a surrogate decision-maker. A witness observes the consent process and attests that the oral presentation of information made by the investigator is consistent with the disclosures made in the informed-consent document. A witness may also help the potential subject to understand the presented information so that he or she can make an informed decision regarding participation. A surrogate decision-maker acts for the potential subject and actually decides if the potential subject will participate in the study.
Pre-test
On the advice of the co-investigator, prior to the actual research, this study will be pretested among five individuals with similar characteristics to the study population in the same locality. The Principal Investigator was calibrated on the Oral examination and the use of the instructor assisted questionnaire for disabilities by the DOH research coordinator and the Principal Supervisor.
Results
Description of Sample
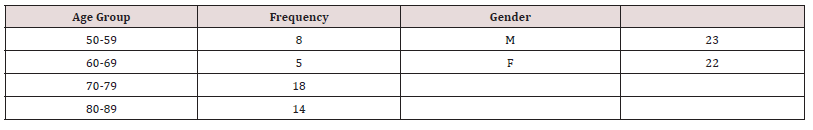
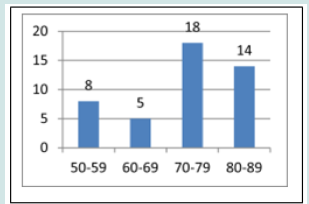
The targeted sample size was 50, however due to advice and restrictions from CHREC to limit the study to the northern region of the district, only 46 participants were recruited. Of the 46 participants, 23 were male and 22 female with a male-to-female ratio 0f 1.1:1. The participants’ ages ranged from 50-89 with an average age of 74 years. Table 1 and Figure 2 shows that there were more participants in the age range 70-79 years but less in 60-69 years. Figure 1 shows that more male participants were recruited than female.
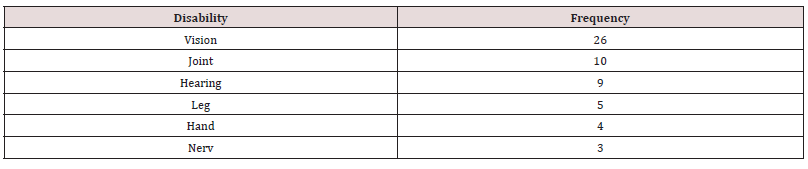
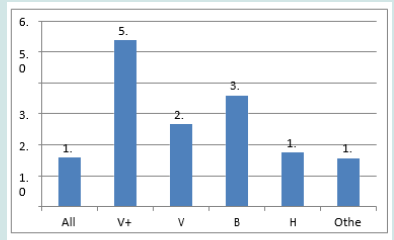
Description of Disabilities
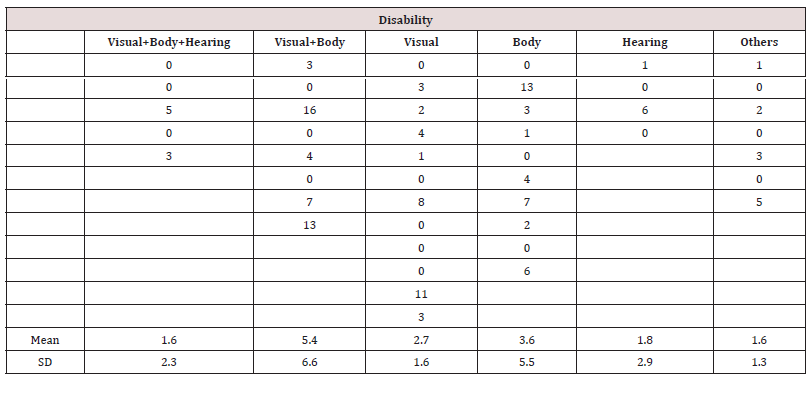
Disabilities were grouped into six (6) groups based on their disability type to ascertain the most frequent type of disability. Figure 3 show that vision has the highest frequency, meaning to say that more participants have visual impairments and impairment related to Nerve was the least frequent types. Now that we have established the most common type of disability in Rendovah district, the types of disabilities were again grouped into four (4) basic groups, namely Visual, Body, Hearing impairments and others. Visual impairments include those with partially blind, blind due to aging and those that blind from birth, Body impairments include hand, joint, leg and nerve impairments, Hearing group are those that are deaf, either at birth or aging, Others group are those elderly that has disabilities other than mentioned above (Table 2). These include, cleft palate, voice function and fluency of speech and limited body activities. While analysing the data, it was found that one person can have more than one type of disabilities, thus the basic groups were regrouped into six (6) subgroups for analysis purposes. Table 3 and Figure 4 indicates that more of the participants have visual and body combined while visual, body and hearing combined and others have the lowest frequency.
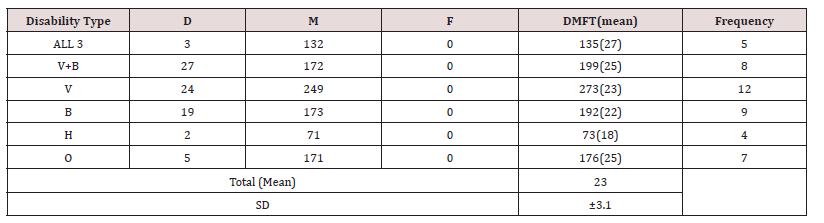
Dentition Status
The dentition status as measured by the mean DMFT was 23±3.1 (mean±SD) (Table 4). Although there were no similar studies to compare the data at the country level, similar studies in Pakistan (DMFT = 16.3) and the USA (DMFT = 18.3) clearly shows that disabled adults in Rendovah have poor dentition status [38,39].
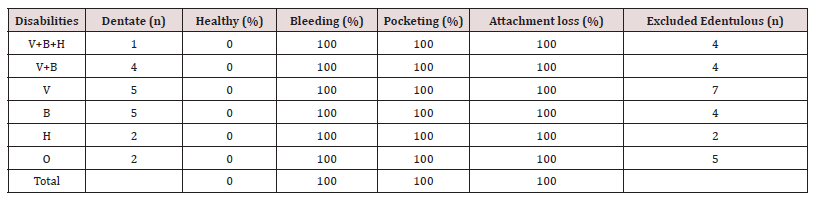
Periodontal Status
The periodontal status of the participants as measured by the modified Community Periodontal Index was summarized in Table 5 below. Table 5 and Figure 5 shows that none of the 64% dentate (n=28) patients have healthy periodontal condition, ALL the dentate (28) participants have bleeding gums and periodontal pocketing, indicative of periodontal diseases.
Denture Status
Sixty four (64%) per cent of the participants were dentate with an average teeth of 15, ranges from 1- 15 teeth. The remaining 36% were edentulous. Of the 36% edentulous participants 65% wear complete upper and lower denture, the remaining 35% didn’t. Out the 64% who are dentate, none wear any partial denture despite having missing teeth (Figures 6 & 7).
Oral Mucosal Lesion Status
There is no Oral mucosal lesion detected in any of the participants.
Discussion
The study reflects the poor oral health status of the elderly with disabilities in Rendovah District. Higher mean DMFT, higher prevalence of periodontal diseases and edentulousness are the major oral health problems facing the participants. Similar studies in Pakistan and the USA also reported that elderly and disabled population have poor oral health status [38,39]. Participants with visual, body and hearing impairments combined and visual and body combined have the highest mean DMFT, while participants with hearing impairments alone have a lower DMFT score. Robust evidence [18- 27] have shown that individual disabilities are a risk factor to poor oral health, this study shows that participants with more than one type of disability have higher DMFT. This is an indicative of the larger magnitude of the impact of disability on oral health status of the patients. Although there is no oral mucosal lesion detected in any of the participants, there is a higher prevalence of periodontal diseases exist as measured by CPI. This is an indicative poor oral hygiene practice among the disabled adults despite type and severity of the disabilities they have. Lack of knowledge of good oral health is evident. This study reveals that 100% of the 64% of the participants who are dentate suffered from periodontal disease. This result is more severe compared to the Pakistan and USA study which has 70% and 80.3% respectively.
Moreover, this study contradicts the year 2000 study6 which indicated that there is a mark increased prevalence of Oral cancer in adults in Solomon Island. This is due to the religious belief of the participants. Even though their religious background was not obtained, most of the participants were members of the Seventh Day Adventist Church, which has a strong teaching of healthy diet and abstinence from alcohol, tobacco and areca nut chewing. Numerous evidence has shown the reason for poor oral health status of the disabled adults. Waldron S et al. [18] pointed out that adults with visual impairments are unable to recognize signs of oral diseases and have limited ability to maintain oral health. Difficulty accessing oral health services without assistance is one other reason why visually impaired adult continue to suffer poor oral health. Peterson et al. [22], pointed out that adults with body impairments have difficulty caring for themselves regarding oral hygiene practice, unable to access services is also highlighted as one factor contributing to poor oral health status in adults with body disabilities. Lack of communication is the major obstacle facing hearing impaired adults. Communication is a two way process, where a speaker and a listener are involved. In this case, there is no listener. This barrier in delivering oral health hygiene by dental professionals and restricting the victim to hear and understand the oral health education continue to contribute to the poor oral health status of hearing impaired adults. This was highlighted by Waldron and Santhosh [18,19]. Other factor limiting the full participation and practice of good oral hygiene by the disabled adults were fear and anxiety, financial constraint, physical barriers, lack of time and domiciliary equipment and transportation [30-34].
Conclusion and Recommendations
The current study clearly indicates that oral health status of the disabled adults in Rendovah District is very poor. There is a need for commitment at the national level to care for this vulnerable population, this includes: building public policy that consider free oral health services for the disabled, reorienting the oral health services so equal distribution of services reached the vulnerable population. Physical barriers should be removed from the health centre for easy accessibility for the disabled. The policy should be clear and should be backed by sufficient resources. It is time the Solomon Island government accelerates senior citizen and especially the vulnerable and disabled health care programs and provide them with benefits they deserve so as to improve the overall quality of life and wellbeing among the disabled adults. Oral health service providers should be given special training to tackle issues facing the vulnerable populations. Community nurses or health workers should be trained with basic skills to detect oral diseases. Caregivers and relatives should be educated on oral health care and dietary impact on oral health. If a similar study was to be carried out, a larger sample size would be recommended and that TMJ assessment could be included in examinations and assessment. Otherwise, a large nationwide survey should be conducted to give a reliable picture of the oral health status of these vulnerable adults.
Acknowledgement
God has been a source of knowledge and wisdom in my education, and I wouldn’t make it this far without Him. I would like to convey my sincere thank you to the following for helping me in one way or the other in making this report a success.
a) Professor Jayantha Weerasinghe – for the supervision of this research.
b) Dr Ellison Vane – for co-supervision and the assistance provided during data collection.
c) Dr Temalesi King for guidance and advice on the course.
d) Solomon Island Government for sponsorship of this research.
e) School of Dentistry and Oral Health.
f) Family members for moral and financial support during and after data collection.
g) Registered Nurses, Maghi and Likonia for information and whereabouts of the study populations.
h) Classmates for support and encouragement.
References
- (2009) Solomon Island Government. Population and Housing Census: National Report. Solomon Island National Statistical Office.
- (2012) Solomon Island Government. Health Service Delivery Profile. Ministry of Health and Medical Services.
- (2011) Solomon Islands Statistics Office. Summary of the DHS. Honiara, Solomon Islands Statistics Office and Macro International.
- Maike P (2010) Framework for priorities in health: Solomon Islands country case study. Noumea, Secretariat of the Pacific Community.
- Roybot T (2020) Oral Health Status of Adults with Disability Related to Body Structures and Activities in Rendovah District, Solomon Islands. Journal of Oral Health and Dental Science 6(1).
- Lumukana R, King T (2003) Smoking and Chewing Habits of Oral Cancer Patients in the Solomon Islands. Pacific Health Dialog 10(1): 41-44.
- (2014) World Health Organization. Fact Sheets: Disability and health.
- Peterson PE, Yamamoto T (2005) Improving the Oral Health of Older People: The Approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 33: 81-92.
- Waldman HB, Mary R T, Perlman SP (2006) Slipping Through the Cracks: Dental Care for Older Persons with Intellectual Disabilities. New York State Dental Journal 72(2): 47-51.
- Chen X, Clark JJ, Naorungroj (2013) Oral Health in Older Adults with Dementia living in Different Environments: A Propensity Analysis. Spec Care Dentist 33(5): 239-247.
- Warren JJ, Chalmers JM, Levy SM, Blanco VL, Ettinger RL (1997) Oral Health of Persons with and without Dementia attending a Geriatric Clinic. SCD Speclal Care In Dentistry 17(2).
- Dolan TA (2013) Professional Education to meet the Oral Health needs of Older Adults and Persons with Disabilities. Spec Care Dentist 33(4): 190-197.
- Anders PL, Davis EL (2010) Oral Health of Patients with Intellectual Disabilities: A Systematic Review. Spec Care Dentist 30(3): 110-117.
- Pia G, Thore M, Lars G (2001) Longitudinal Study of Dental Caries, Tooth Mortality and Interproximal Bone Loss in Adults with Intellectual Disability. European Journal of Oral Sciences 109(1): 20.
- Chalmers JM, Carter KD, Spencer AJ (2003) Oral Diseases and Conditions in Community- Living Older Adults with and without Dementia. Spec Core Dentist 23(1): 7-1 7.
- Maupome G, Wyatt CCL, Williams M, Aickin M, Gullion CM (2002) Oral Disorders in Institution-dwelling Elderly Adults: A Graphic Representation. Special Care Dentist 22(5): 194-200.
- Paul F, Joseph C (2002) Oral Health for Adults with Disabilities: Dental Teatment for Adults. The Exceptional Parent 32(9): 1.
- Waldron S (2011) Auditory sensory impairments and the impact on oral healthcare: A review of the literature. Canadian Journal Of Dental Hygiene.
- Santhosh K, Rushabh JD, Anmol M, Manish J, Prabu D et al. (2008) Oral Hygiene Status in Relation to Sociodemographic factors of Children and Adults who are Hearing Impaired, Attending a Special School. Spec Care Dentist 28(6): 258-264.
- Djeri A, Kuzmanović Radman I, Grabež M, Bajić Z, Prtina A, et al. (2014) Oral Health in Children with Hearing and Speech Impairment in Banjaluka. Serbian Dental Journal / Stomatološki Glasnik Srbije 60(3): 139-146.
- V Sandeep, C Vinay, V Madhuri, V Veerabhadra, KS Uloopi, et al. (2014) Impact of visual instruction on oral hygiene status of children with hearing impairment. Journal of the Indian Society of Pedodontics & Preventive Dentistry 32(1): 39-43.
- Kandelman D, Peterson PE, Ueda H (2008) Oral health, General Health, and Quality of life in Older People. Spec Care Dentist 28(6): 224-236.
- Chembri A, Fiske J (2001) The Implications of Visual Impairment in an Elderly Population in recognizing Oral Disease and Maintaining Oral Health. Spec Care Dentist 21(6):222-226.
- Watson EK, Moles DR, Kumar N, Porter SR (2010) The Oral Health Status of Adults with a Visual Impairment, their Dental Care and Oral Health Information needs. Br Dent J 208(8): E15.
- V Atam, H Ram (2004) Oral Problems in Persons with Physical Handicaps who have had Cerebral Vascular Accidents (Strokes). Spec Care Dentist 24(3).
- Neumann J (2012) People with developmental disabilities face greater risk of oral health issues. Chicago Tribune 12: 2.
- Pradhan A , Slade GD, Spencer AJ (2009) Access to Dental Care among Adults with Physical and Intellectual Disabilities: Residence factors. Aust Dent J 54(3): 204-211.
- Gizani S, Kanilorou H, Kavvadia K, Tzoutzas J (2012) Oral Health Care provided by Greek Dentists to Persons with Physical and/or Intellectual Impairment. Spec Care Dentist 32(3): 83-89.
- Smith G, Rooney Y, Nunn J (2009) Provision of Dental Care for Special Care Patients: The view of Irish Dentists in the Republic of Ireland. Journal of the Irish Dental Association 56(2): 80-84.
- Gambhir RS, Brar P, Singh G, Sofat A, Kakar H (2013) Utilization of dental care: An Indian outlook. J Nat Sc Biol Med 4: 292-297.
- Tanya R, Amanda H, Michael B Flora H, Mark H, et al. (2011) Receipt of Dental Care and Barriers Encountered by Persons with Disabilities. Spec Care Dentist 31(2): 63-67.
- Edwards DM, Merry AJ (2002) Disability Part 2: Access to Dental Services for Disabled People. A Questionnaire Survey of Dental Practices in Merseyside. British Dental Journal 193.5: 253-255.
- Stephen RR (2001) The Dental and Oral Care Needs of Adults with a Learning Disability living in a Rural Community: Consideration of the Issues. Journal of Learning Disabilities (14690047) 5(2): 133-156.
- Michael S Strayer (1995) Perceived barriers to oral health care among the homebound. Special Care In Dentistry 15(3): 113-118.
- (2014) International Classification of Functioning, Disability.
- (2014) International Classification of Functioning, Disability, and Health (ICF) Resources.
- Kuruvilla S, Joseph A (1999) Identifying Disability: Comparing House-to-House Survey and Rapid Rural Appraisal. Health Policy and Planning 14(2): 182-190.
- Syed A, Bilal Abdul QM, Izhar F, Ayyaz AK (2012) Oral Health Status of the Elderly in Lahore District of Pakistan. Pakistan Oral & Dental Journal 32(2).
- John PM, Paula MM, Paul CS, Matthew DF, Konstantina EY, et al. (2012) The oral health status of 4,732 adults with intellectual and developmental disabilities. JADA 143(8): 838-846.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...