Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
Congenital Laryngeal Web in Adult Female: Impromptu & Incidental Volume 7 - Issue 2
Sphoorthi Basavannaiah*
- Associate Professor, Department of ENT, Subbaiah Institute of Medical Sciences, India
Received:July 14, 2021; Published:July 23, 2021
Corresponding author: Sphoorthi Basavannaiah, Associate Professor, Department of ENT, Subbaiah Institute of Medical Sciences, India
DOI: 10.32474/SJO.2021.07.000257
Abstract
Congenital laryngeal web constitutes 5% of all congenital laryngeal anomalies. Most of them are either present at birth or in the first few months of life but very rarely at an older age group. It needs both meticulous evaluation and imperative management to the earliest as its presentation can range anywhere between perpetual dysphonia to permanent dyspnoea leading to devastating morbidity and mortality.
Keywords: Glottic web; congenital; dysphonia; dyspnoea; anterior laryngeal web
Introduction
Congenital laryngeal webs are rare abnormalities of the larynx that accounts to 5% of congenital laryngeal anomalies. They arise due to failure of recanalization of the primitive larynx which should usually occur between 8 to 10 weeks of embryogenesis. Clinical manifestations vary according to the extent of glottic involvement and obstruction [1-3]. Shorter webs accounts to dysphonia while larger webs needless to say causes airway compromise, which is an emergency. Surgical intervention ranges from planned and scheduled stenting to early and immediate tracheostomy based on patient symptomatology at the time of presentation and clinical evaluation [2]. Here, is one such patient who presented with laryngeal web, which was impromptu as well as incidental.
Case Report
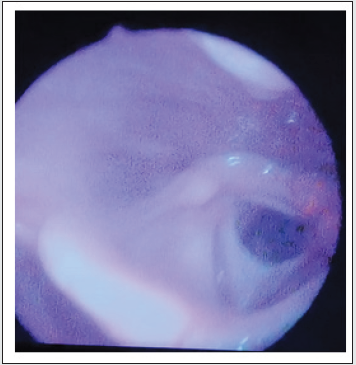
38-year-old female patient comes to ENT outpatient department with dysphonia plus on and off dyspnoea since childhood; both of which went deliberately unnoticed as they were subtle in nature according to the patient history. But these features were a point of curiosity to me during my clinical assessment of this patient. She had no other throat and nose complaints to offer. She gave no previous history of intubation or infection, any history of trauma or any other medical/ surgical history in the past. She was not accustomed to any habits such as tobacco chewing etc. Both general physical as well as systemic examination of the patient was within normal limits. Indirect Rigid 700 endoscopic examination of the larynx showed anterior laryngeal web covering nearly 50% of the glottis lumen, partially compromising the glottic chink i.e. (Cohen’s classification of Type II glottic web) as depicted in the picture below Figure 1. The vocal cords were not actively mobile, as they could not be well visualised. The glottic chink seemed adequate for not causing active airway compromise. There was no abnormality detected in the rest of the laryngeal structures.
Discussion
Congenital laryngeal webs are one of the rare abnormalities of larynx that constitutes 5% of congenital anomalies despite Cohen’s description which states prevalence to be 1 in 1200 children at a Children’s Hospital in Los Angeles. Congenital glottis webs arise due to failure of recanalization of the primitive larynx that usually occurs between 8-10 weeks of embryogenesis. Congenital anterior laryngeal web is a part of the spectrum of this developmental defect mostly, laryngeal atresia [1,4]. There are possibilities of other congenital malformations to occur simultaneously along with this condition such as subglottic stenosis, tracheo-oesophageal fistula and few cardiovascular anomalies although in some cases the web is found isolated [5]. It has found to have a relatively frequent association with 22q11 microdeletion (also seen in children with Velo-cardio-facial syndrome and DiGeorge’s syndrome) as the cause of this malformation according to literature review. Hence, genetic investigation and counselling is imperious [6]. In 1820, Fleischmann described the first case of a laryngeal web after performing autopsy on a 27-day old infant. While in 1869, Zurhelle diagnosed this condition in 11-year-old boy who presented with voice anomaly on an indirect laryngoscopy. Acquired lesions are more common that occur due to an infective aetiology [7]. In the present day, the main causes for such lesions are iatrogenic, following intralaryngeal surgeries or a post-traumatic intubation [5]. These webs usually involve the anterior glottis while the larger ones extend into the subglottis. Sometimes, thin and larger ones are limited only to the glottis. The symptoms can range anywhere from dysphonia, hoarseness of voice, stridor to airway obstruction [8]. Sometimes, the dysphonia goes unnoticed when subtle and the patient presents only with breathlessness, as in this case report. Other differential diagnosis includes tracheal webs, tracheomalacia, tracheal stenosis, leiomyoma of trachea and functional disorder of larynx. This condition is often thought of when there is no response to bronchodilators and anti-inflammatory therapy and have features of upper respiratory tract obstruction as it may masquerade as bronchial asthma [7]. In this case report, it was an impromptu and incidental find, and the patient was not keen for any kind of intervention at present as she was satisfied with the present scenario. The initial evaluation in an anticipated case of a laryngeal web consists of:
a) Describing whether web is present and, if so, whether it is congenital or acquired,
b) Observing for presence of any associated anomalies,
c) Defining the best surgical and anaesthetic options for reconstruction and providing proper airway adequacy [2,5].
When a laryngeal web is assumed, an initial assessment by fiberoptic laryngoscopy is vital. During the fiberoptic examination, things to be observed are the thickness of the web, vocal cord mobility, size of the subglottic lumen, process of swallowing and presence of posterior cleft in the interarytenoid region. The nasal surface of the soft palate for submucosal cleft and abnormal pulsations of medialized internal carotids also should be ruled out. These findings may also be observed in children with chromosome 22q11 deletion as mentioned earlier [4,7]. Imaging technique such as CT scan mainly helps in assessing the degree of subglottic stenosis especially in children with complete atresia. It also provides information about the length and degree of stenosis along with assessment of the rest of the lower airway. However, imaging should not replace direct visual analysis, as it cannot evaluate the airway mucosa and the degree of inflammation [8]. Cohens and Benjamin’s staging [1] of webs is currently used classification for glottis webs. Cohen’s classification defines type I to IV, based on the degree of glottic narrowing as follows: Type I - anterior webs involving 35% or less of the glottis and are free of subglottic extension, Type II - webs involve 35 -50% of the glottis, Type III - webs involve 50-75% of the glottis and are usually thick anteriorly and thin posteriorly and Type IV - webs occupy 75-90% of the airway and are uniformly thick with subglottic extension and vocal cords may not be identifiable. Types II and III may have subglottic extension. But this patient had an isolated thin type II web. Benjamin’s classification has four degrees: glottic webs, subglottic webs, congenital interarytenoid fixation, and supraglottic webs. The two classifications can be concurrently used to define a lesion [1,3]. Depending on the severity of the web, there are three options for management:
a) Observation: It is a good option for an incidental, small anterior web without any respiratory or voice problems, which can be considered in this case as the patient is not much interested in any kind of intervention
b) Endoscopic management: It is ideal for thin webs without any subglottic extension.
c) Open approach: thick webs with subglottic extension, associated with subglottic stenosis or laryngeal cleft require an open approach.
Though cold instruments could be used for lysis of the web like sickle knife, but a CO2 laser is actually and always a better option, if available [3,5]. The CO2 laser cuts precisely, it ablates tissue with minimal surrounding damage and bleeding. Traditionally, keel placement to prevent recurrence of the web has been performed through an external approach which these days have become obsolete due to advent of technology and instrumentation. But now, endoscopic approach can be preferred as a mode in selected cases [7]. Open approaches have some disadvantages such as necessitating tracheostomy and at least two separate external procedures. Endoscopic methods have several advantages such as absence of an external wound, minimal damage to normal voice and deglutition following surgery. Hence case selection for a particular approach is of extreme importance. Unfortunately, although excellent anatomical results, outcomes of voice improvement are erratic and often poor despite of fine surgical procedures and restoration [3,6].
Conclusion
Congenital laryngeal web should be suspected and systematically assessed in the presence of neonatal dysphonia and early onset of laryngitis. Treatment of anterior glottic web remains a therapeutic task and there is no single suitable approach. Treatment protocols range from outdated but still in vogue keel fixation to latest and cutting the edge shooting laser beams and stenting. Few things which are directive, essential and defined towards the management process has to be easy to apply, effective in terms of success, beneficial with regards to patient response, minimally invasive in terms of feasibility, cosmesis, pain threshold and most importantly less chance for recurrence, revision, persistent scarring and lastly providing well adequate, aerated, patent airway and preserve satisfactory voice quality.
References
- Avelino MAG, Pazinatto DB, Rodrigues SO (2020) Congenital laryngeal webs: from diagnosis to surgical outcomes. Brazilian Journal of Otorhinolaryngology 1808-8694(20)30118-X: 1-8.
- Parelkar KA, Thorawade VP, Shah KA (2017) A misdiagnosed laryngeal web: treated with an innovative self-made keel. Journal of Clinical and Diagnostic Research 11(5): 4-6.
- Trey LA, Lambercy K, Monnier P (2016) Management of severe congenital laryngeal webs- a 12-year review. Int J Pediatr Otorhinolaryngol 86: 82-86.
- Amir M, Youssef T (2010) Congenital glottic web: management and anatomical observation. The Clinical Respiratory Journal 4(4): 202-207.
- Goudy S, Bauman N, Manaligod J, Smith RJ (2010) Congenital laryngeal webs: surgical course and outcomes. Ann Otol Rhinol Laryngol 119: 704-706.
- Nicollas R, Triglia JM (2008) The anterior laryngeal webs. Otolaryngologic Clinics of North America 41(5): 877-888.
- Milczuk HA, Smith JD, Everts EC (2008) Congenital laryngeal webs: surgical management and clinical embryology. International Journal of Pediatric Otorhinolaryngology 52(1): 1-9.
- Cohen SR (1985) Congenital glottic webs in children: a retrospective review of 51 patients. Annals of Otology, Rhinology & Laryngology 94(6_suppl): 2-16.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...