Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Research Article(ISSN: 2641-1709) 
Association Between Hearing Loss with Site and Size of Tympanic Membrane Perforation: A Retrospective Study Volume 7 - Issue 1
Harshavardhan Annigeri1 and Borlingegowda Viswanatha2*
- 1Senior Resident, Department of ENT, Bangalore Medical College& Research Institute, India
- 2Professor and Head, Department of ENT, Bangalore Medical College& Research Institute, India
Received:June 18, 2021; Published:June 28, 2021
Corresponding author: Harshavardhan Annigeri, Senior Resident, Department of ENT, Bangalore Medical College& Research Institute, Bangalore, India
DOI: 10.32474/SJO.2021.07.000251
Abstract
Background: Perforation of tympanic membrane decreases surface area and allows the sound waves to pass through middle ear directly. Size of perforation and severity of the hearing loss are related.
Aim: The present study was aimed to evaluate association between hearing loss with site and size of tympanic membrane perforation.
Methods: All patients between 15-60 years of age with chronic otitis media safe type attending to outpatient clinic of ENT, Bangalore Medical College over the period of one year were included in this hospital-based retrospective study. The patients with unsafe CSOM, mixed hearing loss, and refusal to participate in the study, were excluded.
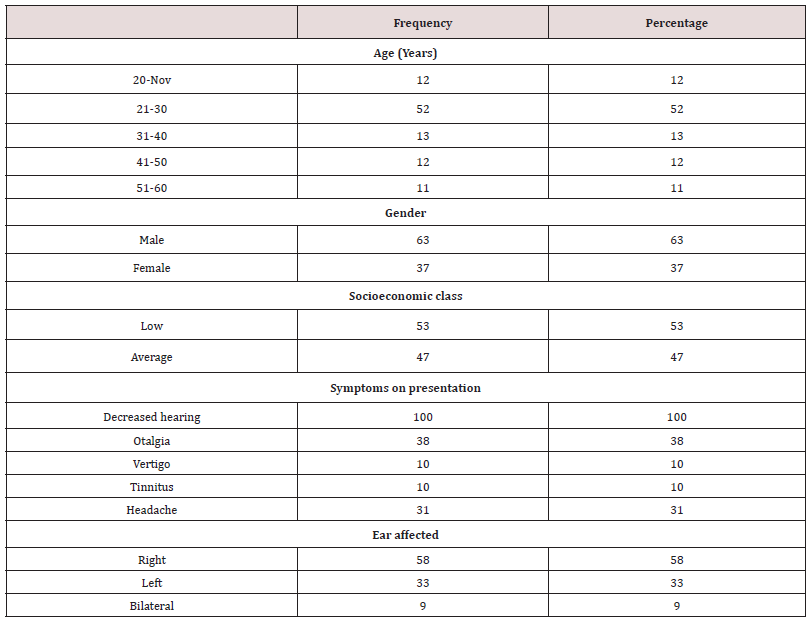
Results: 52% patients aged between 21 and 30 years. Male to female ratio was 1.7:1. 53% patients belonged to average socioeconomic class. The most common symptom on presentation was decreased hearing present in all the patients followed by otalgia (38%), and headache (31%). Unilateral ear was affected in 82 patients in our study. In 9 patients, both ears were affected. Among 50% ears, size of perforation was 10-30 mm2 followed by 0-9 mm2 in 40% ears, and >30 mm2 in 10% patients. We also observed that the patients with higher perforation have an increase in hearing loss on PTA examination (P<.0001). Among 100 ears, the most common perforation site was central (70%) followed by antero-superior (19%), antero-inferior (15%), postero-inferior (9%), and postero-superior (3%). We also observed that median PTA frequency on postero-superior site was significantly higher than antero-superior, anterosuperior, and central site (P<0.01).
Conclusion: Hearing loss is directly related to the size of TM perforation, as the size increases hearing loss also increases.
Keywords:Chronic otitis media; tympanic membrane; hearing loss
Introduction
Chronic suppurative otitis media (CSOM) is the persistent inflammation of the middle ear or mastoid cavity. CSOM usually manifests as intermittent or persistent ear discharge through a perforated tympanic membrane [1,2]. Initially, CSOM presents with mucopurulent discharge through perforated tympanic membrane with otalgia; then hearing impairment follows [3]. CSOM is one of main cause of middle ear disease and a major cause for hearing loss in the developing countries [3]. In India, overcrowding and poor hygiene as well nutrition is observed; thereby, adding to the prevalent CSOM. Tympanic membrane (TM) plays a major role in middle ear transformer mechanism. Perforation of TM decreases the total ratio of the surface area and allows the sound waves to pass through middle ear directly. With larger TM perforation size, hearing loss severity increases. In the recent years, several clinical studies have been conducted in patients of CSOM to correlate the hearing loss with the characters of the perforation such as size and site [4]. The present study was aimed to evaluate association between hearing loss with site and size of tympanic membrane perforation.
Patients and Methods
All patients between 15-60 years of age with chronic otitis media safe type attending to outpatient clinic of ENT, Bangalore Medical College over the period of one year were included in this hospital-based retrospective study. The patients with unsafe CSOM, mixed hearing loss, and refusal to participate in the study, were excluded. Each of the participants was interviewed with a pretested questionnaire and examined clinically to assess the features of tympanic membrane perforation. Examination included detailed history of the patient, local and systemic examination, detailed examination of the patient including ear, nose examination. Ear examination was done using otoscope, microscope, tuning fork tests using 512 Hz. Tympanic membrane was divided into five segments antero-superior, postero-superior, antero-inferior, postero-inferior and central for the localization of the perforation site, which was assessed using otoscope. Depending upon area, perforation was divided into 3 groups. Group I: Small perforation 0-9 mm2. Group II: Medium perforation 9-30 mm2, and Group III: Large perforation >30 mm2.
Data analysis
Data were recorded into Microsoft® Excel workbook 2019 and exported into SPSS v21.0 (IBM, USA). Categorical data were expressed as frequency and percentages. Normative quantitative variables between multiple groups were expressed as mean and standard deviation and compared using one-way ANOVA followed by Bonferroni’s post-hoc correction. Non-normative quantitative variables between multiple groups were expressed as median and compared using Kruskal-Wallis test followed by pairwise comparison. P value <0.05 was considered significant.
Results
General characteristics
Table 1 shows general characteristics of the study participants. Mean age of the study participants was 33.91±13.23 years ranging from 15 years to 60 years. In our study, 52% patients aged between 21 and 30 years. Male to female ratio was 1.7:1. 53% patients belonged to average socioeconomic class. The most common symptom on presentation was decreased hearing present in all the patients followed by otalgia (38%), and headache (31%). Unilateral ear was affected in 82 patients in our study. In 9 patients, both ears were affected. A total of 100 ears were affected.
Duration of disease
Out of 100 affected ears, only 34% (n=18) had duration of disease more than 5 years, 58% had duration between 1-5 years, and remaining <1 year.
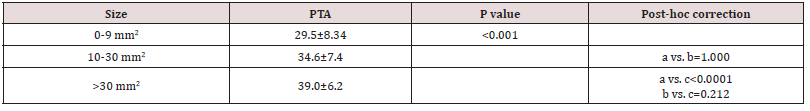
Association between size of perforation
Among 50% ears, size of the perforation was 10-30 mm2 followed by 0-9 mm2 in 40% ears, and >30 mm2 in 10% patients. We also observed that the patients with higher perforation have an increase in hearing loss on PTA examination (P<.0001) (Table 2).
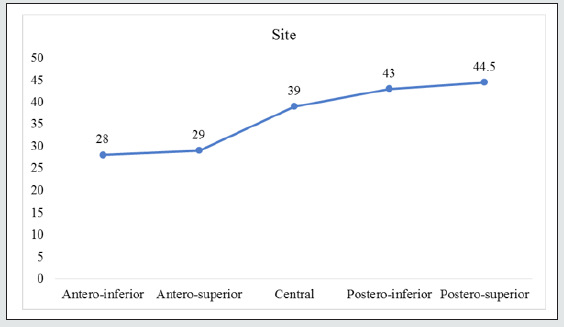
Association between site of perforation
Among 100 ears, the most common site of perforation was central (70%) followed by antero-superior (19%), antero-inferior (15%), postero-inferior (9%), and postero-superior (3%). We also observed that median PTA frequency on postero-superior site was significantly higher than antero-superior, antero-inferior, and central site (P<0.01) (Figure 1).
Figure 1: Line diagram showing trend in hearing loss with site of perforation. Values are expressed as median.
Discussion
The present study assessed the effect of size and site of tympanic membrane perforation on degree of hearing loss in patients of CSOM safe. In our study, mean age of the study participants was 33.91±13.23 years ranging from 15 years to 60 years. In our study, 52% patients aged between 21 and 30 years. The possible reason of the group is being more active socially as well as more health conscious. The presence of shorter and straight Eustachian tube predisposes easy passage of infection in this age group could also be a reason. Our findings are in concordance with Dessai et al and Prasansuk et al who reported similar findings [4,5]. In our study, 61.4% of the patients in our study were males. These findings have been supported by various investigators. Aneesa et al reported that the number of males in the study group was higher than the number of females (M:F=1.38:1) [6]. In our study, majority of the patients belonged to low socioeconomic class. Anil and Bayahati reported that safe type (Tubotympanic) of CSOM, is most commonly seen in low socioeconomic class among adolescents and mid-aged group people [7]. In our study, the most common symptom on presentation was decreased hearing in all the patients followed by otalgia, and headache. In a study from Nigeria, the most common presenting symptom was otorrhea (81.5%), followed by otalgia (72.8%) and tinnitus (55.7%) [8]. In our study, among 100 ears, the most common TM perforation site of central. Nahata et al. reported observed that hearing loss was higher in posterior perforation, followed by central perforation, and anterior perforation [9]. Our study observed an increasing trend of hearing loss from anterior to posterior site (P<0.001). In a study by Aneesa et al, there was significant increase in mean hearing loss from anterior perforation to posterior perforation [6]. This can be associated with the direct exposure to the sound waves, which results in cancellation of phase difference among the oval and round windows. When comparing the severity of hearing loss with various sizes of perforation, increased hearing loss with increased size of perforation was observed. Our results were comparable with Nahata et al, and Pannu et al. [9,10].
Conclusion
Hearing loss is directly related to the size of TM perforation, as the size increases hearing loss also increases. Posterior quadrant TM perforations have more hearing loss as compared to anterior quadrant perforations of TM.
References
- Orji F (2013) A survey of the burden of management of chronic suppurative otitis media in a developing country,” Ann Med Health Sci Res 3: 598-612.
- Kamal N, Joarder AH, Chowdhury AA, Khan AW (2004) Prevalence of chronic suppurative otitis media among the children living in two selected slums of Dhaka city. Bangladesh Med Res Counc Bull 30: 95-104.
- Basak B, Gayen GC, Sarkar MD, Dhar G, Ray R, et al. (2014) Demographic profile of CSOM in a rural tertiary care hospital. IOSR J Pharm 4: 43-46.
- Dessai TD, Philip R (2017) Influence of Tympanic Membrane Perforation on Hearing Loss. Glob J Oto 5: 55-73.
- Prasansuk S, Hinchcliffe R (1982) Tympanic membrane perforation discriptors and hearing levels in otitis media. Audiology 1: 43-51.
- Aneesa M, Siraj S, Ali A (2019) Correlation of tympanic membrane perforations with hearing loss. Int J Otorhinolaryngol Head Neck Surg 5: 1213-1216.
- Anil H, Byahatti N (2019) Relation of site and size of Tympanic membrane perforation on Hearing loss with help of PTA. IP J Surg Allied Sci 1: 82-85.
- Adegbiji WA, Olajide GT, Olajuyin OA, Olatoke F, Nwawolo CC (2018) Pattern of tympanic membrane perforation in a tertiary hospital in Nigeria. Niger J Clin Pract 21: 1044-1049.
- Nahata V, Patil CY, Patil RK, Gattani G, Disawal A, et al. (2014) Tympanic membrane perforation: its correlation with hearing loss and frequency affected-an analytical study. Indian J otol 20: 10-15.
- Pannu KK, Chadha S, Kumar D, Preeti (2011) Evaluation of hearing loss in tympanic membrane perforation. Indian J Otolaryngol Head Neck Surg 63: 208-213.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...