Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1709
Case Report(ISSN: 2641-1709) 
Adenoid Cystic Carcinoma of the Sinonasal Tract: Two Cases Report Volume 5 - Issue 2
Mouna Bellakhdher, Maha Mejbri*, Wassim Kermani and Mohamed Abdelkefi
- ENT Department, Farhat Hached Academic Hospital, Tunisia
Received: August 24, 2020; Published: September 10, 2020
Corresponding author: Maha Mejbri, ENT Department, Farhat Hached Academic Hospital, Sousse, Tunisia
DOI: 10.32474/SJO.2020.05.000206
Abstract
Adenoid cystic carcinomas (ACC) of the sinonasal tract is a malignant neoplasm, characterized by slow and insidious growth. Thus, patients usually present in advanced stages. Clinical presentation is unspecific. Treatment is based on surgery followed by radiotherapy. Since the tumor spreads through perineural and hematological routes, delayed metastasis and local recurrence may occur several years after remission. In the present manuscript, we report the case of two patients who present with an ACC of the maxillary sinus diagnosed in an advanced stage. Orbital and cerebral involvement was objectified in one patient. Treatment consists in surgery. Post-operative radiotherapy was performed in one patient. He had a complete remission. Loco-regional recurrence occurred in the second patient. ACC is a particular entity among sinonasal cancers. Further studies are needed to define multimodal treatment including surgery, radiotherapy, and chemotherapy
Keywords: Adenoid cystic carcinoma; sinonasal tract; surgery, radiotherapy
Introduction
Adenoid cystic carcinoma (ACC) of the sinonasal tract is a rare cancer that originates from salivary glands [1]. It is the most frequent malignancy in the maxillary sinus among non-squamous cell carcinomas [2]. Clinically, it presents as a slow growing and locally aggressive tumor with a tendency to local recurrence and late metastasis [3]. Through two cases report, we illustrate clinical, histological, and therapeutic characteristics of sinonasal ACC.
Case Presentation
Case 1:
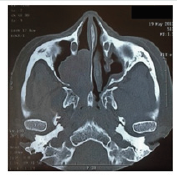
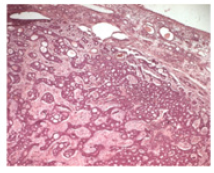
A 50-year-old female patient, with no medical history, presented with right nasal obstruction, epistaxis and nasal discharge that appeared one year ago. Physical examination found a mass of the right nasal cavity. The neck was free from lymph nodes. The neurological and ophthalmological examination were normal. CT scan showed a 5 cm mass, occupying the right maxillary sinus (Figure 1). Tumor extended to the ethmoid and the right nasal cavity. A biopsy of the lesion was performed. Histological examination (Figure 2) concluded to ACC with a cribriform type. No metastasis was found. Tumor was classified T3N0M0. Patient was operated on by Rouge-Denker technique. Post-operative radiotherapy was performed. Patient had regular clinical and radiological follow-up. No recurrence was noted during the 10 year-follow-up.
Case 2:
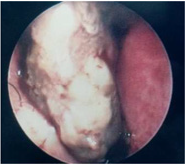
A 39-year-old male patient, presented with unilateral rhino logical symptoms (epistaxis, rhinorrhea, and nasal obstruction) evolving for 5 months. At the physical examination, we found a nasal deformity and a bleeding mass of the left nasal cavity (Figure 3) that extended to the nasopharynx. A left exophthalmia was noted. No cervical lymph nodes were found. The ocular motility and the fundus examination were normal. MRI was performed and showed a mass of the left maxillary sinus which was isointense on both T1 and T2-weighted sequences. Extension to the nasal cavity, nasopharynx and left orbit was objectified. Tumor was removed by paralateronasal approach. Post-operative radiotherapy was planned. Unfortunately, orbital, and cutaneous recurrence occurred. Thus, palliative radiotherapy was achieved.
Discussion and Conclusion
Sinonasal tract malignancies are rare tumors that account for
3% to 5% of all the upper aerodigestive tract cancers [4]. Among
these malignancies, ACC is the most frequent salivary gland cancer.
It represents 10% of all malignancies at this site [5,6] and about 10%
to 25% of all ACCs of the head and neck [7]. It is a slow-growing and
locally aggressive tumor with clinical, biological, and therapeutic
characteristics. Mean age at diagnosis is 55 to 57-year-old [8]. ACC
is thought to be hormonally dependent. A female predominance
was noted in literature [9]. Tumor growth is insidious thus,
patients are asymptomatic for a long period and may present with
advanced-stage disease [3] . ACC is also characterized by a tendency
for perineural spread along major and minor nerves which makes
the treatment challenging [10]. Most frequent signs are nasal
obstruction, epistaxis, nasal discharge, facial pain and dysosmia [6]
likewise our patients. This unspecific presentation leads generally
to a delayed diagnosis. When the tumor reaches large dimensions
and invades surrounding bone and structures, severe signs appear
such as headaches, seizures, ophthalmoplegia, diplopia and
trigeminal neuralgia [6,8]. The occurrence of neurological and
ophthalmological signs is correlated with poor prognosis [3]. The
maxillary sinus is the most common site followed by the nasal cavity
and the ethmoid sinus [8,11]. The frontal and sphenoid sinuses are
correlated with a worse survival rates due to their proximity to the
skull base [7]. Skull base involvement and intracranial extension
are remarkably high. Cervical lymph node metastases are rarely
reported. They accounted for 6% in the series of Rhee [11], 3.6%
in the series of Unsal [7] and none of our patients. Lymph node
involvement is correlated with poor prognosis as they represent a
risk factor for distant metastasis and low survival rate [12].
Histologically, ACC is composed of three subtypes: tubular,
cribriform, and solid [7]. The cribriform subtype is the most
common one whereas the solid subtype has the worst prognosis
[11]. Treatment of sinonasal ACC is based on surgery, followed
by radiotherapy [13]. According to Lupinetti et al., overall, and
disease-specific survival are improved when patients are treated
with surgery and postoperative radiation compared with other
treatment modalities [6]. The aim of surgery is to ensure complete
tumor removal with negative margins. However, surgery of
advanced stages tumor is challenging and can result in serious
morbidity, especially when critical anatomic structures are involved
such as the brain, the orbit, the cranial nerves, and the nasopharynx
[10]. In our series, tumor extended to the nasopharynx and orbit
in one patient. ACC is a radiosensitive tumor but not radio curable
[13]. Postoperative radiotherapy aims to clear positive margins
left after surgery [14]. Long-term survival does not seem to be
improved when radiotherapy is associated, but 5-year diseasefree
period is slightly prolonged [7]. In the study of Rhee, the
5-year local recurrence rate was 42% in T3 and T4 stages despite
postoperative radiotherapy was performed in most of the patients
[11]. Radiation therapy alone is indicated in T4 unresectable tumors
[15]. Chemotherapy has not proven effectiveness in ACC treatment.
Further clinical trials using combined therapeutic approaches are
required [11]. ACC is characterized by local recurrence and distant
metastasis that can occur several years after initial treatment and
remission [11]. In the series of Miller, local failure rate was 50%.
This high rate was explained by the high proportion of patients
diagnosed in advanced stages [10]. In other studies, treatment
failure rates range from 60% to 70% [15]. ACC of sinonasal tract has
a poor prognosis. The most relevant prognosis factors are tumor
site, skull base invasion, stage, histopathologic type, and treatment
modalities. Treatment is based on surgery. Even though ACC is not radio curable, post-operative radiotherapy improves locoregional
control. Early diagnosis, applying the appropriate therapeutic
approach and long-term follow-up are the mean guarantees to
improve prognosis.
Funding and Conflict of Interest
Authors declare that they have not receive any financial support. No conflict of interest.
References
- Duberge T, Benezery K, Resbeut M, Azria D, Minsat M, et al. (2012) Adenoid cystic carcinoma of the head and neck: a retrospective series of 169 cases. Cancer Radiother 16(4): 247-256.
- da Cruz Perez DE, Pires FR, Lopes MA, de Almeida OP, Kowalski LP (2006) Adenoid cystic carcinoma and mucoepidermoid carcinoma of the maxillary sinus: report of a 44-year experience of 25 cases from a single institution. J Oral Maxillofac Surg 64(11): 1592-1597.
- Andrade MF, de Faria PR, Cardoso SV, Santos MR, Dias FL, et al. (2014) Adenoid cystic carcinoma of the maxillary sinus: a clinical-pathological report of 10 years of experience from a single institution. Int J Oral Maxillofac Surg 43(11): 1313-1318.
- Banuchi V, Mallen J, Kraus D (2015) Cancers of the nose, sinus, and skull base. Surg Oncol Clin N Am 24(3): 563-577.
- Kokemueller H, Eckardt A, Brachvogel P, Hausamen JE (2004) Adenoid cystic carcinoma of the head and neck--a 20 years’ experience. Int J Oral Maxillofac Surg 33(1): 25-31.
- Lupinetti AD, Roberts DB, Williams MD, Kupferman ME, Rosenthal DI, et al. (2007) Sinonasal adenoid cystic carcinoma: The MD Anderson Cancer Center experience. Cancer 110(12): 2726-2731.
- Unsal AA, Chung SY, Zhou AH, Baredes S, Eloy JA (2017) Sinonasal adenoid cystic carcinoma: a population-based analysis of 694 cases. Int Forum Allergy Rhinol 7(3): 312-320.
- Husain Q, Kanumuri VV, Svider PF, Radvansky BM, Boghani Z, et al. (2013) Sinonasal adenoid cystic carcinoma: systematic review of survival and treatment strategies. Otolaryngol Head Neck Surg 148(1): 29-39.
- Turner JH, Reh DD (2012) Incidence and survival in patients with sinonasal cancer: a historical analysis of population-based data. Head Neck 34(6): 877-885.
- Miller ED, Blakaj DM, Swanson BJ, Xiao W, Gillison ML, et al. (2017) Sinonasal adenoid cystic carcinoma: Treatment outcomes and association with human papillomavirus. Head Neck 39(7): 1405-1411.
- Rhee CS, Won TB, Lee CH, Min YG, Sung MW, et al. (2006) Adenoid cystic carcinoma of the sinonasal tract: treatment results. Laryngoscope 116(6): 982-986.
- Spiro RH (1997) Distant metastasis in adenoid cystic carcinoma of salivary origin. Am J Surg 174(5): 495-498.
- Wiseman SM, Popat SR, Rigual NR, Hicks WL Jr, Orner JB, et al. (2002) Adenoid cystic carcinoma of the paranasal sinuses or nasal cavity: a 40-year review of 35 cases. Ear Nose Throat J 81(8): 510-514, 516-517.
- Garden AS, Weber RS, Morrison WH, Ang KK, Peters LJ (1995) The influence of positive margins and nerve invasion in adenoid cystic carcinoma of the head and neck treated with surgery and radiation. Int J Radiat Oncol Biol Phys 32(3): 619-626.
- Bhattacharyya N (2003) Factors affecting survival in maxillary sinus cancer. J Oral Maxillofac Surg 61(9): 1016-1021.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...