Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-6003
Research Article(ISSN: 2638-6003) 
Application of Autologous Platelet Rich Plasma to Graft Donor Sites to Reduce Pain and Augment Healing: A Randomized Controlled Trial Volume 4 - Issue 3
Samarth Gupta*
- Department of Plastic Surgery, SMS Hospital, India
Received: September 22, 2020; Published: October 09, 2020
Corresponding author: Samarth Gupta, Department of Plastic Surgery, SMS Hospital, Jaipur, India
DOI: 10.32474/OSMOAJ.2020.04.000190
<
Abstract
Introduction
Platelet Rich Plasma has been vastly utilized in the medical field due to its property to heal the wounds and the multitude of growth factors it contains. Traditionally, donor sites are left to heal with a primary dressing which would otherwise be opened as the wound heals. Various methods of donor site management have been described such as collagen dressings, hydrocolloid, alginate, hydro fiber, silicone dressing, or paraffin gauze. However, it is often encountered that there is a delay in the healing process and accompanied by pain at donor site. Furthermore, in a relatively small population of patients who have a tendency to hypertrophic scar formation, this becomes a challenge for the plastic surgeon. It not only leads to unsightly scars but also additional problems of dryness and itching. Owing to the healing properties of PRP, we designed this study to utilize it for donor site dressings following split thickness skin grafts. This study primarily throws light on the usage of Autologous PRP over Split thickness Skin Graft donor sites to augment healing, and reduce pain.
Materials and Methods
The 100 patients enrolled in this study between January 2018- July 2019 were divided into two groups of 50 each on a randomized basis, one of which was subjected to use of Autologous PRP, which was topically applied at the donor site and the other control group where the wound was traditionally dressed. Pain scales were measured in the immediate postoperative period as well as at the time of first dressing. Dressing was opened on the 14th postoperative day and observed for healing.
Results
Patients with the PRP group showed statistically significant faster healing at the 14th postoperative day, as compared to the control group which required continuing dressing 3-4 weeks. We also measured pain scale in the postoperative period and at the time of first dressing, which was significantly less in the PRP group. It’s worthy to mention that a few of the patients who has hypertrophic scars previously, did not develop after the application of PRP.
Conclusion
Application of PRP is a safe, cost effective, easy method to achieve faster healing in graft donor site areas, which is more often than not bothersome to the patients undergoing split thickness grafts. It also reduces the postoperative pain at the donor site. We recommend its use more frequently in managing donor site for Split thickness skin grafts.
Keywords: PRP; Donor Site; Pain; Skin Grafts; Wound Healing
Introduction
Split thickness skin graft is a widely accepted technique to cover large defects. However, it is often encountered that there is a delay in healing process, which may further lead to problems such as pain, infection and hypertrophic scar formation. Autologous PRP has been used in various treatment modalities in the field of plastic surgery for its healing, adhesive and hemostatic properties owing to the growth factors that are released. Platelet-rich plasma (PRP) is an autologous product that concentrates a large number of platelets in a small volume of plasma [1]. PRP also provides an immediate surgical hemostatic agent that is biocompatible, safe, and effective. The platelet comprises granules which are released when PRP is applied to the surface. These granules have properties which:
• Accelerates endothelial, epithelial, and epidermal
regeneration
• Stimulates angiogenesis
• Enhances collagen synthesis
• Promotes soft tissue healing
• Decreases dermal scarring
• Enhances the hemostatic response to injury
Another concern about PRP is its method of preparation.
Although a lot has been written about methods of preparing PRP,
there is still confusion over terminology to classify and describe the
different variations of platelet concentrations. There are several
ready to use commercial devices available, which make preparation
of PRP simple and easy. However, they add to the costs of treatment.
They are usually able to achieve a concentration of 2-5 times
above baseline. Higher Platelet count above this has not shown
to cause any additional benefits contrary to the assumptions;
in fact concentration of PRP above 2.5 has been shown to be
detrimental[4]. Marx proposed that platelet count of 10 lakh/ml in
5 mL of PRP, as a working definition of PRP, based on the scientific
proof of bone and soft tissue healing enhancement [13].Rughetti et
al.[14] found that the stimulation for proliferation of endothelial
cells peak at 1.25 × 106 and angiogenesis at 1.5 × 106 platelets/
mL, respectively. This signifies the fact that a PRP platelet count 1
million/mL has become the working definition for therapeutic PRP.
We have our own institutional method of preparing PRP which has
been rectified by our labs to achieve a high platelet concentration.
In view of the properties of PRP, we have theorized its use to
be expanded in donor site dressings which has been a point of
concern for a long time for both patients and treating physicians.
In this study we have demonstrated how application of PRP aids
in donor site healing. We have also shown that it reduces pain in
the immediate postoperative period. The application of autologous
Platelet-Rich Plasma (PRP) to STSG application sites has been
recently described and theorized to help in faster healing and
treatment of hypertrophic scars.
Materials and Methods
The study was performed in the Department of Plastic, Reconstructive and Burns Surgery, SMS Hospital, Jaipur between 2018-2020. We obtained a sample size of 100 using our institutional software to make the study statistically significant in view of the previous studies involving use of PRP for various treatments. The 100 patients taken into the study with written and informed consent were randomly divided into two groups of 50 each in cases and controls. Sealed envelopes containing a number indicative of the group assignment (even number = Cases, uneven = Controls) were used to randomly allocate patients into two groups in the operation theatre. 100 envelopes were prepared in this manner and the patients were blinded to the treatment. All the patients gave consent to be a part of this trial as well.The patients in the cases group were subjected to use of PRP at the donor site followed by the standard paraffin gauze dressing. In the patients of the control group, the donor site was managed simply by paraffin gauze dressing without the use of PRP.Intraoperatively, fentanyl in a dose of 1ug/kg was given as a pain medication and postoperatively no pain medication was administered until the patient complained of pain. If he did complain of pain a rescue drug Inj. Diclofenac in a dose 1mg/kg was given. All patients with wounds that required split thickness skin grafting were included in the study. To be a part of the study the patient had to fulfill the following inclusion criteria
Inclusion Criteria
• All patients which required harvesting of split thickness
skin graft
• S. Albumin above 2.5 g/dl
The following patients were excluded from the study
Exclusion Criteria
• Active Infection
• Age >70 years
• Pus, discharge
• Immunocompromised patients
• Exposed ligaments/ bone/cartilage
• Underlying Comorbidities uncontrolled hypertension,
uncontrolled diabetes and renal disorders
• Uncooperative Patients
• Drug Abuse
Our Method of Preparing Prp
• Patients venous sample was taken
• Blood Collected in 10 ml ACD vials
• The vials were spun for 5 mins at 1500 rpm (Soft Spin)
after which the supernatant was spun at 3500 rpm (Hard Spin) for
15 mins.
• PRP is spread as a thin film over the area using a syringe
with a 24 gauge needle
• 5 ml for 100 square cm was used.
Post-Operative Care
Dressing was opened on the 14th Postoperative day to assess
for healing and pain by an independent observer thereby masking
the treatment allocation. The wound was said to heal well if on
inspection there was complete epithelization of the donor site
characterised by healthy pink tissue, there was no residual raw area
or any signs of infection.
Next follow up was done on the 21st day.
Primary Outcome
• Donor site healing on 14th post-operative day
• Pain scale in the postoperative period at 6,10 and 16
hours and on the 14th day at the time of dressing.
• A paired T test was used as a tool to assess the test of
significance.
• All patients adhered to follow up protocols as designed in
our study.
Results
Healing on 14th Day
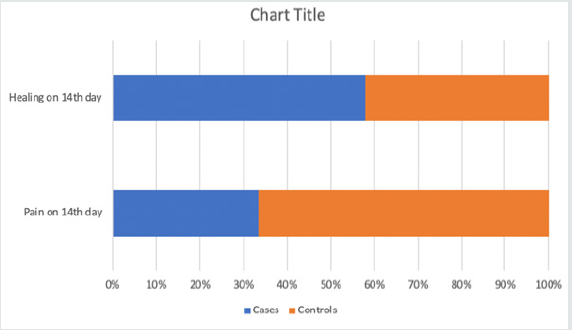
The wound healing was assessed by an independent observer at the time of the first dressing. The wound was said to heal well if on inspection there was complete epithelization of the donor site characterised by healthy pink tissue, there was no residual raw area or any signs of infection. 48 out of 50 patients had good wound healing on the 14th post operative day. In other two patients we required more dressings. The first of these was a 60 year old male with no other comorbidities who underwent grafting for post traumatic ulcer on foot. The other patient was a 55 year old male with traumatic ulcer over knee. In both these patients we required 3 additional dressings before the wound completely healed. (Table 1) shows the wound healing in both cases and controls on the day 14th post operatively. A paired T Test was applied to assess this where in a p value of <0.005 was obtained. It was observed that the patients in the PRP group had significantly higher fasted wound healing rates as compared to the controlled group.
Assessment of Pain Control
Pain at the donor site was measured at 6, 10, 16 hours post operatively by the use of VAS Scales. Further, pain was also measured at the time of first dressing. (Table 2) depicts the Mean VAS Scores at the defined intervals. Paired T test was used to define the test of significance and It was observed that the Mean VAS Score was significantly lower with a p value <0.05 at 6 hours in the Cases group. At 10hours and 16 hours the VAS Scores were similar. The Pain scores were also significantly less at the time of first dressing with a p value <0.045. (Table 2) and (Figure 2)depict Mean VAS Scores in two groups. (Figure 1) depicts pain and healing on the day of first dressing.
Cost of PRP
The overall running cost of PRP is only $2-3 depending upon the number of 8 ml ACD vials being used. In contrast to other dressings such as negative pressure wound therapy, collagen or hydrofiber for which the patient may have to bear a cost running into hundreds of dollars.
Observation in Patients with a history of Hypertrophic Scar
5 of our patients in the PRP group had hypertrophic Scars in previously grafted donor sites. All of them had undergone skin grafting at least a year back. These patients were followed for 1 year and we observed that these patients did not develop hypertrophic scars in the follow-up. 3 patients in the control group who were found to have hypertrophic scar at previously grafted donor sites developed hypertrophy in the donor sire at 1 year follow up. (Figure 4,5)showreduced hypertrophy in one of the patients.
Discussion
PRP is defined as a biological product derived from patients own blood with the concentration of platelets above the baseline [2]. PRP has been known to have many benefits which help early vascularisation by delivering these growth factors and increasing collagen synthesis. There are other benefits like reduced hematoma, infection, and cost. Donor site care with dressing material should provide optimum healing, be cost effective and should prevent complications such as pain, infection, discomfort and scarring. It is often encountered that patients feel more pain at the donor site as compared to the recipient wound bed[3,4,5]. There have been a variety of dressings and devices that are available in the clinical practice. However, there is no single dressing that is devoid of complications or can address to all the necessary problems with donor sites. This has led to variations in choice of dressing or topical agents used by health care professionals. [6,7,8]. Gibran et al conducted a study on forty post burn patients in which they used PRP as a wound adhesive for fixing of grafts over wound beds comparing it to traditional methods like sutures and staples. [9] Schade and Roukis found PRP enhances wound healing time by releasing the growth factors it contains. [10] Kakudo et al. published a study which proved that PRP helps in revealed that PRP epithelialization and angiogenesis of graft donor sites [11]. There are many other studies that have been conducted which demonstrates that PRP aids healing and reduces pain providing growth factors to the local site. In that view this study was conducted to overcome these problems at graft donor sites.
Various methods have been described to prepare PRP. Use of
different compounds in vials has also been described. In a recent
study, Wanden-Berghe et al. found accelerated wound healing in
chronic wound beds by PRP activated by calcium chloride [12].
In our center, after taking the venous sample in ACD tubes there
are two cycles of centrifugation. The first spin step is performed at
constant acceleration to separate RBCs from the remaining whole
blood volume. After the first spin step, the whole blood separates
into three layers: an upper layer that contains mostly platelets and
WBC, an intermediate thin layer that is known as the buffy coat
and that is rich in WBCs, and a bottom layer that consists mostly
of RBCs. For the production of PRP the upper layer and superficial
buffy coat are transferred to an empty sterile tube. The second
spin step is then performed. The upper portion of the volume that
is composed mostly of PPP (platelet-poor plasma) is removed.
Pellets are homogenized in the lower 1/3rd (5 ml of plasma) to
create the PRP (Platelet-Rich Plasma).The platelet concentrations
have been classified into Low with a count of 0.5 x million/μl,
Intermediate having 0.5-3 x million/μl and High with 3-5 x million/
μl. We have been able to achieve high concentration of platelets
by our technique of preparation. We observed that the problem
of prolonged dressings and donor site pain for which there was
no definite solution. Keeping that in mind and with the proven
properties of PRP, this study was conducted. It has been observed that there was significantly faster healing rates and that the donor
site in most of the cases had healed when the dressing was opened
on day 14. We observed that our study showed lower pain scales at
6 hours. At 10 and 16 hours the similarity in pain scales was due to
the rescue medication which was given to patients that complained
of pain. Pain scales were also significantly lower on the day of first
dressing in coherence with Previous studies that correlate regular
application of PRP with pain reduction during gauze changes
[15,16,17,18,19,20]
We also followed up 8 patients (5 in PRP group and 3 in Control
group) who had history of hypertrophic scar formation in donor
sites. It was observed that patients in PRP group did not develop
Hypertrophy in donor sites as compared to the control group where
hypertrophy occurred at the end of 1st year. Although no statistical
analysis was done on these patients we found it worthy enough for
its mention and that a study could be done to prove this hypothesis.
Conclusion
Application of PRP is a safe, cost effective, easy method to promote faster healing in donor site areas from where split thickness skin grafts have harvested. It also reduces the postoperative pain at the donor site. We recommend its use more frequently in managing donor site for split thickness skin grafts.
Ethical Statement
• Funding: None
• Conflict of Interest: Pradeep Goil and Samarth Gupta
declare that they have no conflict of interest
• Ethical approval: Institutional Ethics Committee has given
the due clearance for the study
• Consent to participate: All patients have given a written
and informed consent
• Declaration of Helsinki: The authors state that our study
complies with Declaration of Helsinki, and that the locally
appointed ethics committee has approved the research protocol
and informed consent has been obtained from the subjects.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...