Lupine Publishers Group
Lupine Publishers
Case Report(ISSN: 2644-1209) 
A Metastatic Tumor of Ewing’s Sarcoma in the Orbit Volume 1 - Issue 5
Dilan YILDIZ1, Gamze MADEN1*, Şeyma Gülcenur ÖZTURAN1, Serap Yurttaşer Ocak1, Mehmet Tayfur1, Mehmet Egemen KARATAŞ2 and Mustafa Nuri ELÇİOĞLU1
- 1Department of Ophthalmology, Okmeydani Training and Research Hospital, Turkey
- 2Department of Ophthalmology, Okmeydani Training and Research Hospital, Turkey
Received: September 14, 2018; Published: September 21, 2018
*Corresponding author: Department of Ophthalmology, Okmeydani Training and Research Hospital, Turkey
DOI: 10.32474/TOOAJ.2018.01.000123
Abstract
Aim: We aimed to present the patient with the metastasis of Ewing’s sarcoma in orbit because of being seen very rarely.
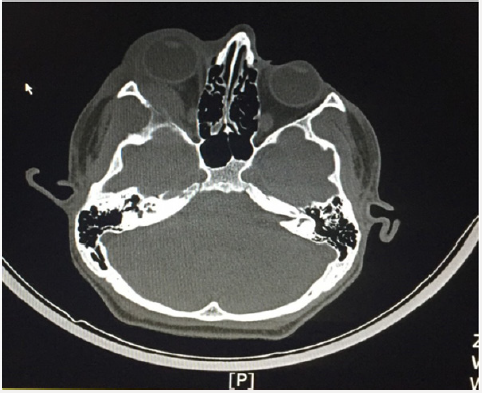
Case: A 16-year-old male patient was admitted to our clinic in June 2017 with a complaint of swelling in the right eye for 2 days. In the examination, the best corrected vision acuity (BCVA) was 0,8 for the right eye and 0,9 for the left eye by Snellen. Right periobital edema, proptosis and ptosis were present, and the eye movements were restricted in all directions (Figure 1). There was a chemosis in the right eye in the slit lamp examination and a slight deletion of the nasal borders of the bilateral optic disc in the fundus examination. When the story of the patient was questioned, we learned that he was treated with a diagnosis of Ewing’s sarcoma in the left fibula 1 year ago and was diagnosed as urgent because of a metastatic tumor causes the medulla spinalis compression which was found in the lumbar region 1 week before. The massive lesion on the posterior wall of the right orbit was detected in the orbital tomography, which made us think metastasis of the Ewing’s sarcoma primarily for the differential diagnosis and the patient was directed to the Department of Pediatric Oncology (Figure 2). Upon observation of multiple bone involvement in the Positron Emission Tomography, the patient was initiated a 5-day Iphosphamide + Carboplastin + Etoposide systemic chemotherapy protocol. On day 2, a dramatic regression was observed in the patient’s symptoms. At 1-week follow-up, the BCVA was bilateral 1.0, the eye movements were normal in all directions, the slit-lamp and fundus findings and the intraocular pressure were normal (Figure 3).
Conclusion: In conclusion, in this case it is emphasized that orbital metastases should be considered in the differential diagnosis of patients with proptosis and periorbital edema and also it is important to question the story of the patient detailed so it’s possible to prevent the development of permanent pathologies if treatment is started rapidly.
Introduction
Ewing’s sarcoma is an undifferentiated, high-grade diffuse round cell tumor that most commonly occurs in the 5 to 25-yearold, often located in the diaphysis in the long bones [1-3]. Although it can be seen in all bones, the most common sites are femur, tibia, humerus. It’s mostly located in the pelvis bone of the trunk and the involvement of the skull is rare [2]. Approximately the quarters of the cases have metastases when it was diagnosed [3]. Metastases occur most frequently in the hematogenous pathway, and the most often seen metastasis are to the lungs, bone and bone marrow [4]. The most frequent bone metastases are found in the vertebral bones [5]. Orbital metastasis is very rare. In this case report, a rare Ewing’s sarcoma patient with orbital metastasis will be discussed.
Case Report
A 16-year-old male patient was admitted to our clinic in June 2017 with a complaint of swelling in the right eye for 2 days. In the examination, the best corrected vision acuity (BCVA) was 0,8 for the right eye and 0,9 for the left eye by Snellen. Direct and indirect light reflexes were positive. Relative afferent pupil defect (RAPD) and diplopia were absent. Right periobital edema, proptosis and ptosis were present, and the eye movements were restricted in all directions (Figure 1). There was a chemosis in the right eye in the slit lamp examination and a slight deletion of the nasal borders of the bilateral optic disc in the fundus examination. When the story of the patient was questioned, we learned that he was treated with a diagnosis of Ewing’s sarcoma in the left fibula 1 year ago and was diagnosed as urgent because of a metastatic tumor causes the medulla spinalis compression which was found in the lumbar region 1 week before. The massive lesion on the posterior wall of the right orbit was detected in the orbital tomography, which made us think metastasis of the Ewing’s sarcoma primarily for the differential diagnosis and the patient was directed to the Department of Pediatric Oncology (Figure 2).
In the orbital contrast enhanced magnetic resonance imaging of the patient who was admitted to the Department of Pediatric Oncology at the same day; there were a mass lesion compatible with metastasis in the posterior-external wall of the right orbit, proptosis in the right globe, and inflammation in the right periorbital soft tissue. Upon observation of multiple bone involvement in the Positron Emission Tomography, the patient was initiated a 5-day Iphosphamide + Carboplastin + Etoposide systemic chemotherapy protocol. On day 2, a dramatic regression was observed in the patient’s symptoms. At 1 week follow-up, the BCVA was bilateral 1.0, the eye movements were normal in all directions, the slit-lamp and fundus findings and the intraocular pressure were normal (Figure 3).
Discussion
The metastatic lesions are the seven percent of the orbit cancers [6]. The most common metastatic cancers in the orbit are from the breast, prostate and lung cancer for adults, while the most commons for the pediatric group are neuroblastoma, Ewing’s sarcoma and Wilm’s tumor [6,7]. In Ewing’s sarcoma, metastatic lesions usually involve the external wall of the orbit and the most common findings were proptosis, ptosis, periorbital edema and visual loss (6). In our case, the lesion was in the posterior external wall of the right orbit and the patient had proptosis, periorbital edema, and chemosis findings.
Ewing’s sarcoma is a poorly differentiated, high grade round cell tumor that most commonly occurs in men between 5 and 25 years of age and frequently located in the diaphysis in long bones [1-3]. Although it can be seen in all bones, the most common places are femur, tibia, humerus. Our case was a 16 years old man and also primary tumor site was tibia so it fits with this profile.
Metastases occur at an early stage in four of the Ewing sarcoma cases [3]. Metastases occur most commonly in the hematogenous tract, and metastasis to the lungs, bone and bone marrow are the most often seen ones [4]. The most frequent bone metastases are found in the vertebral bones [5]. Orbital metastasis is very rare. When our patient was diagnosed, the inguinal lymph nodes were metastasized, but there was no lung involvement. Metastasis occurred in the spinal canal and orbit when he arrived 2 months after the treatment. Bone marrow biopsy was negative.
Ewing’s sarcoma is sensitive to chemotherapy and radiotherapy. Chemotherapy is given before and after the local treatment. Chemotherapy protocols commonly used are VACA (vincristine, actinomycin-D, cyclophosphamide and adriamycin), VAIA (vincristine, actinomycin-D, ifosfamide, adriamycin) or EVAIA (VAIA + etoposide). In cases with good response during preoperative chemotherapy (often a good response is obtained); it is seen that tumor cells are commonly necrosis, tumor is reduced and retracted into bone. Advanced techniques such as myeloablative regimens and bone marrow transplantation may be applied in the presence of multiple bone involvement or metastasis, where necessary [3]. VACA was administered as a primary treatment for our patient, and after the orbital metastasis was occured, the protocol of iphosphamide + carboplastin + etoposide systemic chemotherapy was initiated for five days. On the second day of treatment, the findings were dramatically regressed.
Conclusion
In conclusion, in this case it is emphasized that orbital metastases should be considered in the differential diagnosis of patients with proptosis and periorbital edema and also it is important to question the story of the patient detailed so it’s possible to prevent the development of permanent pathologies if treatment is started rapidly.
References
- Mario Campanacci (1999) Ewing’s sarcoma and primitive Neuroectodermal tumor. Bone and Soft Tissue Tumors pp. 653-683.
- Campanacci M, Bertoni F, Bacchini P, Enneking WF, Notini S (1990) Ewing’s Sarcoma. Bone and Soft Tissue Tumors. Vienna: Springer Verlag pp. 509-538.
- De Ioris MA, Prete A, Cozza R, Podda M, Manzitti C, et al. (2013) Ewing sarcoma of the bone in children under 6 years of age. PLoS One 8(1): 53223.
- Cangir A, Vietti TJ, Gehan EA, Burgert EO Jr, Thomas P, et al. (1990) Ewing’s sarcoma metastatis at diagnosis. Results and comparisons of two intergroup Ewing’s sarcoma studies. Cancer 66(5): 887-893.
- Wilkins RM, Pritchart DJ, Burgert EO, Unni KK (1986) Ewing’s sarcoma of bone. Experience with 140 patients. Cancer 58(11): 2551-2555.
- Macedo JE, Machado M, Araujo A, Angelico V, Lopes JM (2007) Orbital metastasis as a rare form of clinical presentation of nonsmall cell lung cancer. J Thor Oncol 2(2): 166-167.
- Shields JA Metastatic cancer to the orbit in: Diagnosis and management of orbital tumors. Philadelphia: WB Saunders comp pp. 291-315.