Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6628
Case Report(ISSN: 2637-6628) 
Whole Spine Metastasis from Supratentorial Glioblastoma Multiforme Volume 4 - Issue 2
Lakhdar F*, Benzagmout M, Chakour K and Chaoui ME
- Department of neurosurgery, Hassan II Hospital, University Sidi Mohammed Ben Abdellah, Fez, Morocco
Received: June 17, 2019; Published: June 30, 2020
Corresponding author: Fayçal Lakhdar, Department of neurosurgery, Hassan II hospital, University Sidi Mohammed Ben Abdellah, Fez, Morocco
DOI: 10.32474/OJNBD.2020.04.000183
Abstract
Glioblastoma multiforme (GBM) is a highly aggressive and one of the most common primary brain tumors in adults. Metastasis of intracranial glioblastoma via the cerebrospinal fluid to the spine is a rare occurrence with a poor prognosis. We hereby present a rare case of GM in a 28-year-old man, who developed intramedullary, extramedullary, as well as spinal leptomeningeal metastasis 6 months after surgery of supratentoriel glioblastoma multiforme.
Keywords: Glioblastoma; Intramedullary; Leptomeningeal; Spinal Metastasis
Abbreviations and Acronyms: GBM: Glioblastoma Multiforme; WHO: World Health Organization
Introduction
GBM is categorized as grade 4 in the WHO scale and often occurs in the supratentorial white matter, mostly in the frontal, temporal, and parietal lobes [1]. However, leptomeningeal metastasis from primary intracranial GBM is a rare phenomenon and there is usually a long interval between the cerebral lesion and the spinal seeding. Although the best treatment involves maximal surgical resection followed by adjuvant radiotherapy and chemotherapy, the median survival time is less than two years [2]. We report a case of symptomatic leptomeningeal metastasis from primary intracerebral glioblastoma.
Case Report
A 28-year-old man presented with history of headache, nausea, vomiting and generalized seizures. Neurological examination revealed no deficit, also general and other systemic examinations were unremarkable. Brain CT scan showed a left parietal irregular, heterogeneously enhancing lesion (Figure 1a). He underwent left parietal craniotomy and gross total removal. Histopathology was suggestive of GBM, World Health Organization (WHO) grade IV. The patient then underwent external beam radiotherapy for 6 weeks associated to chemotherapy (Temozolamide capsule 100 mg daily) with an uneventful course. Postoperative control CT scan during follow up was not suggestive of residual/recurrent disease (Figure 1b).
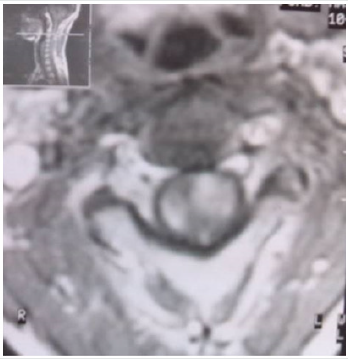
After approximatively 6 months, the patient presented with gradually progressive weakness of lower limb, with numbness in both the lower limbs and bowel and bladder involvement. On neurological examination, spastic paraparesis with the sensory level at T9. MRI of the spine showed a multiple, enhancing, intramedullary lesion with cord expansion with diffuse leptomeningeal involvement all along the cervical and dorsal spine (Figure 2a & 2b). He underwent biopsy of the dorsal lesion and histopathology was suggestive of metastatic glioblastoma (WHO grade IV). Then the patient refuses radiotherapy and succumbed to his disease after a period of 4 months.
Figure 2a: Spinal MRI gadolinium enhanced T1-weighted images showing invasion of tumor through the pia mater into the medulla of the cervical spinal cord.
Discussion
Glioblastoma multiforme is an aggressive, high-grade
malignancy of glial cell origin, accounts for 16% of all primary
brain tumors with a well-known tendency for intracranial spread
but rarely for extracranial spread [1, 3]. Spinal intramedullary
metastasis and entire spinal cord involvement from primary GBM
is a rare event. CSF dissemination occurs in 15 to 25% of cases of
supratentorial GBM. In the other hand, the rate of spinal metastasis
from cerebral GBM has been reported to be 0.4-2% [4,5].
GBM predominates subcortically in the temporal and parietal
lobes and can be multifocal with spinal leptomeningeal metastasis.
Even tough, the common symptoms of spinal metastasis are radicular
pain, sensory loss, followed by paraparesis or quadriparesis, bowel
or bladder dysfunction, and sexual dysfunction [6,7]. The surgical
management of leptomeningeal metastasis is still uncertain due to
the rarity of these cases, although the mainstay of treatment is safe
surgical decompression, followed by adjuvant radiotherapy in total
dosage of 25-40 Gy, and intravenous or intrathecal chemotherapy
[8-10]. Nevertheless, spinal metastasis of GBM have poor prognosis,
with fatal outcome [11].
Conclusion
It is important to consider the possibility leptomeningeal metastasis in a patient with intracranial GBM, to investigate and treat the patient accordingly. Even if safe surgical resection combined with chemo-radiotherapy the prognosis remains very poor, leading to a fatal outcome.
References
- Maslehaty H, Cordovi S, Hefti M (2011) Symptomatic Spinal Metastases of Intracranial Glioblastoma: Clinical Characteristics and Pathomechanism Relating to GFAP Expression. J Neurooncol 101(2):329-333.
- Alatakis S, Malham GM, Thien C (2001) Spinal Leptomeningeal Metastasis from Cerebral Glioblastoma Multiforme Presenting with Radicular Pain: Case Report and Literature Review. Surg Neurol56(1):33-37.
- Witoonpanich P, Bamrungrak K, Jinawath A, Wongwaisayawan S, Phudhichareonrat S, et al. (2011) Glioblastoma Multiforme at the Corpus Callosum with Spinal Leptomeningeal Metastasis. Clin Neurol Neurosurg 113(5):407-410.
- Birbilis TA, Matis GK, Eleftheriadis SG, Theodoropoulou EN, Sivridis E (2010) Spinal Metastasis of Glioblastoma Multiforme: An Uncommon Suspect? Spine (Phila Pa 1976) 35(7):E264-269.
- Tai P, Dubey A, Salim M, Vu K, Koul R (2015) Diagnosis and Management of Spinal Metastasis of Glioblastoma. Can J Neurol Sci42(6):410-413.
- Lun M, Lok E, Gautam S, Wu E, Wong ET (2011) The Natural History of Extracranial Metastasis from Glioblastoma Multiforme. J Neurooncol 105(2):261-273.
- Konar SK, Bir SC, Maiti TK, Nanda A (2017) A systematic Review of Overall Survival in Pediatric Primary Glioblastoma Multiforme of the Spinal Cord. J Neurosurg Pediatr19(2):239-248.
- Lin L, Innerfield CE, Cuccurullo SJ (2014) Symptomatic Spinal Leptomeningeal Metastasis from Intracranial Glioblastoma Multiforme. Am J Phys Med Rehabil93(9):838-839.
- Tinchon A, Oberndorfer S, Marosi C, Rudà R, Sax C, et al. (2012) Malignant Spinal Cord Compression in Cerebral Glioblastoma Multiforme: A Multicenter Case Series and Review of the Literature. J Neurooncol110(2):221-226.
- Shahideh M, Fallah A, Munoz DG, Loch Macdonald R (2012) Systematic review of primary intracranial glioblastoma multiforme with symptomatic spinal metastases, with two illustrative patients. Journal of Clinical Neuroscience 19(8):1080-1086.
- Purkayastha A, Sharma N, Sridhar MS, Abhishek D (2018) Intramedullary Glioblastoma Multiforme of Spine with Intracranial Supratentorial Metastasis: Progressive Disease with a Multifocal Picture. Asian J Neurosurg13(4):1209-1212.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...