Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6628
Review Article(ISSN: 2637-6628) 
Neuropsychiatric Manifestations in Patients with Systemic Lupus Erythematosus Presenting at a Tertiary Care Teaching Hospital of North India Volume 5 - Issue 3
Wani Suhail A1, Sofi Fayaz A2, Mushtaq Ahmed3 and Rayees ul Hamid Wani4*
- 1Senior Resident, Department of Clinical Haematology, SKIMS, Srinagar, India
- 2Professor, Internal Medicine, Division Rheumatology, SKIMS, Srinagar, India
- 3Additional Professor, Internal Medicine, Division Rheumatology, SKIMS, Srinagar, India
- 4Senior Resident, Emergency Medicine, SKIMS, Srinagar, India
Received: March 1, 2021 Published:March 15, 2021
Corresponding author: Rayees ul Hamid Wani, Senior Resident Department of Emergency Medicine, SKIMS, India
DOI: 10.32474/OJNBD.2021.05.000213
Abstract
Background: Systemic Lupus Erythematosus (SLE) is a multisystem autoimmune disease caused by an aberrant immune response.
Aims & Objectives: To study the neuropsychiatric manifestations in patients with Systemic Lupus Erythematosus presenting at a Tertiary Care Teaching Hospital.
Material and Methods: A review of records of SLE patients admitted or evaluated in OPD from March 2010 to June 2017 was carried out.
Results: Over all 85 SLE patients out of 269 which constituted 31.6% of all SLE study group had neuropsychiatric manifestations.
Keywords: Neuropsychiatric Manifestations; Systemic Lupus Erythematosus
Introduction
Systemic Lupus Erythematosus (SLE) is an autoimmune disease that targeted cytoplasm and nucleous of body cells. It causes wide manifestations from the most outer organ to the internal organs. Organ damages may varies, from mild to severe. About 5,000,000 people around the world are affected by SLE. United Kingdom reported the prevalence of 97 cases per 100,000 people in 2012.Signs and symptoms of SLE can be varied. Genetic is predisposition factor which plays role in SLE pathogenesis. Asian’s reported more severe clinical manifestations and higher mortality rate compared to the American and European. SLE can be found in all groups age and both male and female, but it is more common found in females during their fertile period [1]. Systemic Lupus Erythematosus (SLE) is a multisystem autoimmune disease of unknown etiology characterized by the production of non-organ specific auto-antibodies directed to nuclear, cytoplasmic and cell surface antigens, which may lead to a wide range of tissue injuries [2].
The involvement of vital organs and tissues such as the brain, blood, and the kidney in most patients, the vast majority of whom are women of childbearing age. The prevalence ranges from 20 to 150 cases per 100,000 population, with the highest prevalence reported in Brazil, and appears to be increasing as the disease is recognized more readily and survival increases. In the United States, people of African, Hispanic, or Asian ancestry, as compared with those of other racial or ethnic groups, tend to have an increased prevalence of SLE and greater involvement of vital organs. The 10-year survival rate is about 70% [3].
Patients with systemic Lupus Erythematous (SLE) that suffer from one or more of several neuropsychiatric symptoms represent a subcategory termed ‘neuropsychiatric lupus’ (NPSLE). Cohorts of SLE patients suggest that nearly half will suffer from NPSLE during their disease course. The definition of NPSLE is a tough challenge owing to the broad spectrum of neuropsychiatric symptoms that it encompasses, most of which are non- specific (for example, headache, cognitive dysfunction, etc.). The most accepted effort, so far, to classify NPSLE was made by an American College of Rheumatology (ACR) expert-committee, in 1999 . This committee identified 19 neuropsychiatric conditions, termed ‘case definitions’, in NPSLE patients, including 12 central nervous system (CNS) and 7 peripheral nervous system ones. It should be noted that a few population-based studies, aimed at validating these ACR-NPSLE case definitions, did not find them to be effective in differentiating NPSLE patients from those with neuropsychiatric manifestations not associated with SLE [4]. The present study was conducted to study the neuropsychiatric manifestations of systemic lupus erythematosus presenting to a tertiary care teaching hospital.
Objectivese
To study the Neuropsychiatric manifestations in patients with Systemic Lupus Erythematosus presenting at a Tertiary Care Teaching Hospital.
Material and Methods
- Study Design: Review of records(retrospective and prospective).
- Study Duration: Seven Years, 2010-2017
- Study Setting: A hospital-based study: Rheumatology Division and Medical record section, SKIMS
- Sample size: All the patients admitted or evaluated during the study period.
- Criteria for classification of the SLE: American College of Rheumatology (ACR) classification criteria revised in 1982 updated in 1997 and the Systemic Lupus Erythematosus Collaborating Clinic (SLICC) criteria.
- Statistical Analysis: The data was entered in Ms excel sheets and was analysed by SPSS 23.0.The data was represented in the form of graphs and tables.
Results
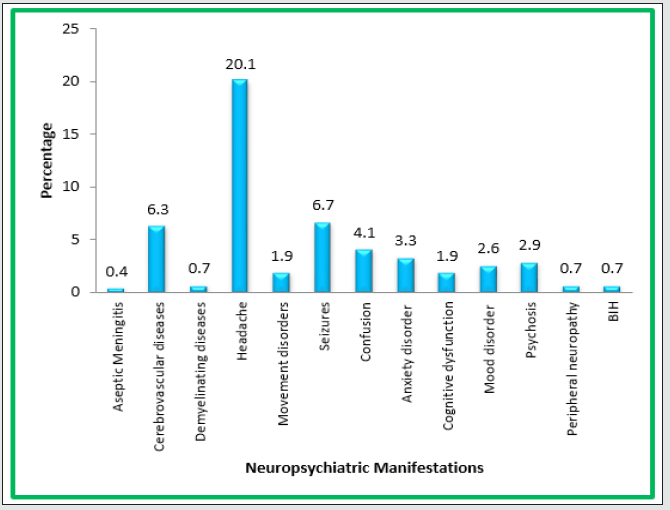
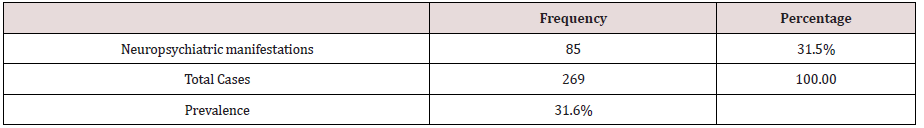
A total of 269 patients were studied. Data of patients with systemic lupus erythematosus patients over a period of seven years from March 2010 to July 2017 was collected. Over all 85 SLE patients out of 269 which constituted 31.6% of all SLE study group had neuropsychiatric manifestations (Table 1). In our study, 54(20.1%) had headache, 18(6.7%) had seizures, 17(16.3%) had cerebrovascular disease, 11 (4.1%) had confusion, 9(3.3%) had anxiety disorder, 7(2.6%) and 8(2.9%) had mood disorder and psychosis respectively. Peripheral neuropathy and BIH each was present in 2(0.7%) patients. 5(1.9%) patients had movement disorder (Figure 1).
Discussione
The onset of Systemic Lupus Erythematosus (SLE) is often marked by seemingly innocent musculoskeletal symptoms, and these may dominate its early course. Unless they are recognized, patients may go on for a long time with some rheumatic diagnosis until an acute febrile episode or visceral or cutaneous symptoms afford clues to the correct diagnosis. Systemic lupus erythematosus is protean in its manifestations and follows a relapsing and remitting course. Cumulative Neuropsychiatric manifestation in our study patients (e.g aseptic meningitis, cerebrovascular diseases, demyelinating diseases, headache, movement disorder, seizures, confusion, anxiety disorder, cognitive dysfunction, mood disorder, psychosis, peripheral neuropathy and benign intracranial hypertension) were present in 31.6% of SLE patients (85/269) which was in agreement with those of American study by Dubois et al, [5-9], Arabia by Al-attia et al, [10-13], and multicentric study in Tunisia by Monia Smiti Khanfir et al [7]. Although the incidence of neuropsychiatric systems were lower as was observed by Malaviya et al, [5], which can be because of ethnic, environmental and socioeconomial variations and because of variation in disease activity in genetically different populations. Estimates of the prevalence of neuropsychiatric lupus (NPSLE) have ranged from 14% to over 80% in adults. A retrospective study of NPSLE in 185 Chinese children over a 20-year period found that 11% had NPSLE manifestations at the time of diagnosis and an additional 16% developed them within one year [14]. Studies in adults using the ACR case definitions collectively have detected the presence of 14-17 of the 19 NPSLE syndromes and reported a fairly consistent prevalence of the following syndromes: total spectrum of headache (39%–61%), seizures (8%– 18%), cerebrovascular disease (2%– 8%), psychosis (3%–5%), cranial neuropathy (1.5%–2.1%) [15]. Our results of NPSLE (Table 1) were consistent with the world literature (Table 2).
Table 2 Neuropsychiatric Manifestations in Study Patients (CNS and PNS). N=85 (31.6%)
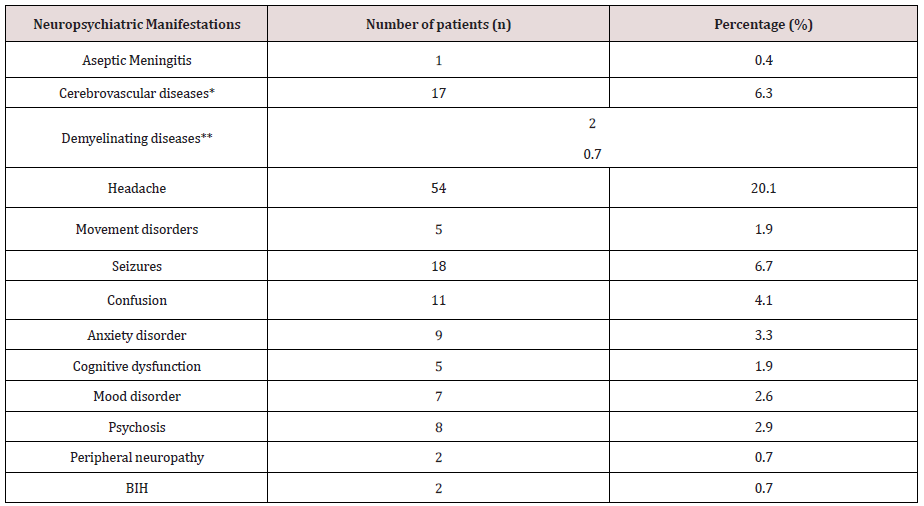
*Cerebrovascular diseases included are Stroke, PRES and CNS Vasculitis. **Demyelinating diseases include are Optic Neuritis and Transverse myelitis.
Summary
Systemic Lupus Erythematosus (SLE) is a multisystem autoimmune disease of unknown etiology characterized by the production of non-organ- specific auto-antibodies directed to nuclear, cytoplasmic and cell surface antigens, which may lead to a wide range of tissue injuries. Over all 85 SLE patients out of 269 which constituted 31.6% of all SLE study group had neuropsychiatric manifestations. In our study out of total patients, 54 (20.1%) had headache, 18(6.7%) had seizures, 17(16.3%) had cerebrovascular disease, 11(4.1%) had confusion, 9 (3.3%) had anxiety disorder, 7(2.6%) and 8(2.9%) had mood disorder and psychosis respectively. Peripheral neuropathy and BIH each was present in 2(0.7%) patients. 5(1.9%) patients had movement disorder.
References
- Duarte C, Couto M, Ines L, Liang MH (2011) Epidemiology of systemic lupus erythematosus. (5thed), London: Elsevier, 673-696.
- Moez Jallouli, Makram Frigui, Mohamed Ben Hmida, Sameh Marzouk, Neila Kaddour, et (2008) Clinical and immunological manifestations of systemic lupus erythematosus: A study of 146 south Tunisian patients. Saudi J Dis Transplant 19(6): 1001-1008.
- Pons Estel GJ, Alarćon GS, Scofield L, Reinlib L, Cooper GS (2010) Understanding the epidemiology and progression of systemic lupus Semin Arthritis Rheum 39(4): 257-268
- Ainiala H, Hietaharju A, Loukkola J, Peltola J, Korpela M, et al. (2001) Validity of the new American College of Rheumatology criteria for neuropsychiatric lupus syndromes: A population-based Arthritis Rheum 45(5): 419-423.
- Malaviya AN, Singh R, Kumar A, Shamar PN (1988) SLE In Northern India. A Review Of 329 Cases. J Assoc Phys India 36(8): 476-840.
- Paudyal BP, Gyawalee M (2012) Clinical Profile of Patients with Systemic Lupus J Nepal Med Assoc 52(187): 111-117.
- Monia Smiti KHANFIR, Mohamed Habib Houman, Eya CHERIF, Amira HAMZAOUI, Sonia SOUISSI, et (2013) TULUP (TUnisian LUPus): A multicentric study of systemic lupus erythematosus in Tunisia. International Journal of Rheumatic Diseases 16(5): 539-546.
- Estes D, Christian CL (1971) The natural history of systemic lupus erythematosus by prospective Medicine (Baltimore) 50(2): 85-95.
- Edmund L Dubois, Denny L Tuffanelli (1964) Clinical manifestations of systemic lupus erythematosus: Computed Analysis of 520 Cases. JAMA 190: 104-111.
- Robert Grigor, John Edmonds, Raymond Lewkonia, Barry Bresnihan, Graham RV Hughes (1978) Systemic Lupus Erythematosus A Prospective Annals of the Rheumatic Diseases 37(2): 121-128.
- Renu Saigal, Amit Kansal, Manoop Mittal, Yadvinder Singh, Hari Ram Maharia, et al. (2011) Clinical Profile of Systemic Lupus Erythematosus Patients at a Tertiary Care Centre in Western India. JIACM 1(13): 27-
- Binoy J, Paul, Muhammed Fassaludeen, Nandakumar, MV Razia (2003) Clinical Profile of Systemic Lupus Erythematosus in Northern Kerala. J Indian Rheumatol Assoc 11: 94-97.
- Haider M Al-Attia (1996) Clinic laboratory profile of 33 Arabs with systemic lupus erythematosus. Postgrad Med J 72(853): 677-679.
- Yu HH, Lee JH, Wang LC, Yang YH, Chiang BL (2006) Neuropsychiatric manifestations in pediatric systemic lupus erythematosus: A 20-year Lupus 15(10): 651-657.
- Eyal Muscal, Robin L Brey (2010) Neurological Manifestations of Systemic Lupus Erythematosus in Children and Neurol Clin 28(1): 61-73.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...