Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6628
Research Article(ISSN: 2637-6628) 
Knowledge of the Approach of the Tensional Cephalea, with First Contact Doctors in the Regional Military Hospital of Specialties of Guadalajara, Mexico Volume 2 - Issue 5
Miranda Nava Gabriel1* and Eladia Estefania Zaragoza Hernández2
- 1Head of the Neurology service, Mexico
- 2Internal Doctor of the Regional Military Hospital of Specialties of Guadalajara, Mexico
Received: June 11, 2019; Published: July 19, 2019
Corresponding author: Miranda Nava Gabriel, Head of the Neurology service, Regional Military Hospital of specialties of Guadalajara, Mexico
DOI: 10.32474/OJNBD.2019.02.000149
Abstract
Cephalea is one of the most common patient’s medical reasons to attend an emergency room. It is estimated that at least one-third of the population between 18 and 65 years has suffered from a headache on some occasion. Therefore, the physician must be able to differentiate between the primary and secondary Cephalea, since the latter can seriously menace the patient’s life. Likewise, to make the right diagnosis of Cephalea, is very important to identify the risk facts, the warning signs, and the diagnosis tools concerning to it. It is very significant to consider that, although the cephalea could have a multifactorial etiology, genetics and molecular biology have a relevant roll in its development. Cephalea becomes a daily challenge for the physician, since a correct approach to this condition fall on the patient´s outcome and quality of life.
Summary
Headache is one of the most common reasons for consultation by which people go to the emergency services. It is estimated that at least a third of the population between 18 and 65 has suffered from a headache on occasion. Therefore, the doctor, when facing a patient with this pathology, should have the ability to differentiate between primary or secondary headache since the latter can seriously compromise the life of your patient. Likewise, it is important to identify the risk factors, warning signs and diagnostic tools related to headache because they could help guide your diagnosis. It is important to keep in mind that, although the headache has a multifactorial etiology, the role that molecular genetics and molecular biology play in its development is also relevant. Headache becomes a daily challenge for the clinician, since the correct outcome of this condition depends on the outcome and quality of life of the patients.
Introduction
Tension Headache
Subtype of most common primary headache. The pain is typically bilateral, oppressive, and mild to moderate in intensity. There is no nausea and it is not aggravated by physical activity. Sensitivity to light, noise or pericranial hypersensitivity may be associated [1-5].
Tension headache is characterized by attacks of pain that are not associated with nausea or vomiting, and that has at least two of the following characteristics:
a) Bilateral headache.
b) Non-pulsating headache.
c) Mild to moderate intensity.
d) Headache does not get worse with activity, such as walking or climbing stairs.
Infrequent Episodic Tension Headache
Infrequent episodes of headache, of typically bilateral location, with tension or oppressive pain of mild to moderate intensity and lasting from minutes to days. This pain does not worsen with habitual physical activity nor is it associated with nausea, but photophobia or phonophobia may occur. Infrequent episodic tension headache is characterized by rare episodes of headache, which appear, on average, less than once a month and comply with the rest of tension headache characteristics (Figure 1). Frequent episodic tension headache: frequent episodes of headache, typically bilateral in location, with tensional or oppressive pain of mild to moderate intensity and lasting from minutes to days. This pain does not worsen with habitual physical activity nor is it associated with nausea, but photophobia or phonophobia may occur. Frequent episodic tension headache is characterized by at least 10 episodes of headache that occur on average, from 1-14 days per month, for more than 3 months (> or = 12 and <180 days per year) and that comply with the rest of criteria of tension headache. Chronic tension headache occurs more than 15 days a month in a period greater than three months. Chronic tension headache should be diagnosed when episodes of headache occur more than 15 days a month for more than three months and meets the rest of the criteria of tension headache. Headache is understood as the presence of pain located above the existing line. between both external ocular edges, to the center of the external auditory canal, the pain that originates below this line should be called facial pain. Headache simultaneously is a symptom and a syndrome [6-10]. When defined as pain in the cephalic limb, the symptom is referred to. On the contrary, when considered as a syndrome it would imply its multicausality and the different types involved. Its physiopathology is mediated by two routes (Figures 2 & 3).
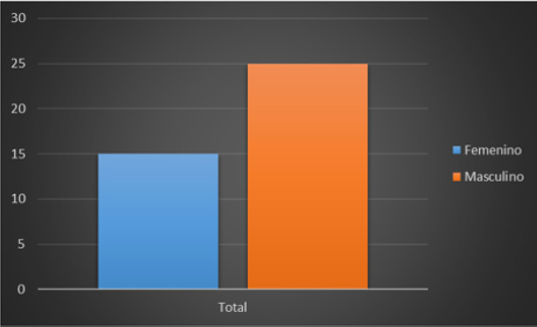
The first, which is the normal physiological response, is generated by the activation of nociceptors in response to tissue injury, visceral distension and other factors. The second, on the contrary, occurs when there is damage or malfunction in the pain pathways related to the central or peripheral nervous system. Within the structures of the cranial vault involved in the process of headache are: the venous sinuses, the anterior and middle meningeal arteries, the dura mater, the trigeminal, glossopharyngeal and vagus nerves, proximal portions of the internal carotid and its branches near of the polygon of Willis, the encephalic trunk, the periaqueductal gray matter and the sensorial nuclei of the thalamus [11]. The extracranial structures also related to headache are: the cranial periosteum, the skin, the subcutaneous cellular tissue, the arteries, the muscles of the neck, the second and third cervical nerves, (C2 and C3), the eyes, the ears, the teeth, paranasal sinuses, among others. According to the World Health Organization in its study “Global Burden of Disease 2012” (Global Burden of Disease 2012), tension headache and migraine appear as the second and third most frequent diseases in the world, (Murray CJ , 2012) and migraine is clearly the most disabling of primary headaches taking into account frequency and burden of the disease (Figure 4). (Lipton RB, 2001) Therefore, it is the most common neurological syndrome that is attended in the first level with 3% of adults who consult with their family doctor every year for this reason (Latinovic R, 2006) and is the disease that most neurologists see in their clinical practice, according to surveys applied in the United States. It has a prevalence throughout life of around 15% in the general population and affects a greater proportion of women (18%) than men (8%) [12-14].
(Steiner TJ, 2013) It has been called the seventh disabling due to its considerable impact on the quality of life of patients. (Steiner TJ, 2013). Headache, being one of the most common reasons for consultation by which people go to the emergency services, has an adult prevalence of 47%. At least a third of the population between 18 and 65 has suffered from a headache on occasion. In children the prevalence is 37 to 51% at 7 years and 57 to 82% between 7 and 15 years, being higher in men than in women between 3 and 7 years, and after 7 years is equal to. After puberty this relationship varies substantially and is estimated to be 3 women for every man. Studies conducted in Mexico show that the people who suffered most from headaches had high school level, were married and resided in the urban area, which generates a reflection on lifestyles and their possible association with the development of this syndrome. Among headaches, migraine is predominantly female: women, compared with men, have a migraine prevalence almost three times higher annually (17% vs. 6%) and the lifetime incidence is almost three times higher (43 vs. 18%) [15-17]. Some studies have suggested that between 3 and 14% of people with episodic migraine patterns progress to chronic migraine. This type of headache is part, along with the chronic tension headache of the group known as chronic daily headaches (CCD), conditions that have become important causes of disability and work absences with an average loss of 7.3 hours of paid work and 7.5 hours of unpaid work, which would represent a total loss of one active work day per month. Headache, in addition to being an important cause of disability, brings consequences on a personal level, since the individuals who suffer from it have a continuous fear of the appearance of new episodes, which frequently affects their social, family and work activities. , thus generating a deterioration in their quality of life.
Clinical Picture
Tensional type headache (CTT) is characterized by the presence of bilateral pain (most of the time), oppressive, non-pulsating, that distinguishes it from migraine, in addition to being less frequent the presence of accompanying symptoms Characteristics of migraine, does not increase with physical activity and mild to moderate intensity (Figures 5 & 6). Therefore, it could be said that the diagnostic criteria of CTT indicate that the patient does not suffer from migraine. It can occur episodically (<15 days a month or <180 days a year) or chronically (> 15 days a month for > 3 months or > 180 days a year), as well as associated or not to muscle pain pericranial The diagnosis is usually made with the criteria of the International Classification of Headache. Even so, not all doctors are familiar with the diagnostic criteria. Underdiagnosis continues to be a major problem in daily practice, resulting in incorrect treatment. Several instruments have been designed to improve the diagnosis of migraine, to identify the psychological alterations it causes, to measure the burden of the disease and disability and to know the reduction in the quality of life that occurs due to pain attacks. These instruments include the ID Migraine, a 3-item test, which has been validated in primary care as a way to improve the rapid diagnosis of migraine; the MIDAS questionnaire used to evaluate the disability caused by migraine attacks and the HIT 6, which is a tool that allows us to measure the impact that headaches have on the quality of life of patients and the severity of pain [18-22].
Despite having all these instruments, the proper selection and interpretation of them is crucial to make faster, more accurate diagnoses that allow us to initiate treatment to patients who are affected by this disease, so that we can grant them an adequate management and they can reincorporate themselves to their daily life without suffering affectations in it. It is of vital importance to establish guidelines regarding the treatment of tension headache and migraine because there is a great variability in clinical practice regarding the management of these two entities; it causes the individuals who suffer them to have a constant fear for the appearance of new episodes and, failing to achieve the restoration of health, they are limited to return to their daily activities, with the respective repercussions on their social, work and family environment , generating a deterioration in their quality of life.
Problem Statement
What is the clinical approach, or cabinet studies for the diagnosis of tension headache in the Regional Military Hospital of Specialties of Guadalajara, Jalisco?
Justification
The most common of consultation in the Neurology service are tension headache and migraine, which can cause substantial levels of disability, not only to patients and their families but to society as a whole, due to its high prevalence in the general population. Approximately half of patients with acute headache have tension headache and 10% have migraine. A migraine attack is a spectacularly complex brain event that can produce a wide variety of neurological and systemic symptoms. Although pain is its most prominent feature, migraine can include a multiplicity of symptoms that occur before, during and after pain [22-25]. This makes headaches a daily challenge for doctors; This is why it is of vital importance to know their clinical presentation, warning signs and diagnostic methods, in order to achieve a clinical approach with a view to timely diagnosis and management, so as not to suffer from episodes of headache or disability. The purpose of this research is to establish a national reference to guide the making of clinical decisions based on recommendations based on the best available evidence. This guide makes available to the staff of the first and second level of care recommendations based on the best available evidence with the intention of standardizing national actions regarding:
Unify diagnostic criteria of Tensional and Migraine Headache in the first and second level of care.
a) Use diagnostic tools for tension headache and migraine in the first and second level of care.
b) Offer prophylactic treatment to adult patients with tension headache and migraine in the first and second level of care.
c) Implement an adequate treatment, using available resources, to patients with tension headache and migraine in the first and second level of care. This will favor the improvement in the effectiveness, safety and quality of medical care, contributing, in this way, to the wellbeing of people and communities, which is the central objective and raison d’être of health services.
Overall Objective
Define the diagnostic method of tension headache by the doctors of the Regional Military Hospital of Guadalajara, Jalisco.
Conclusion
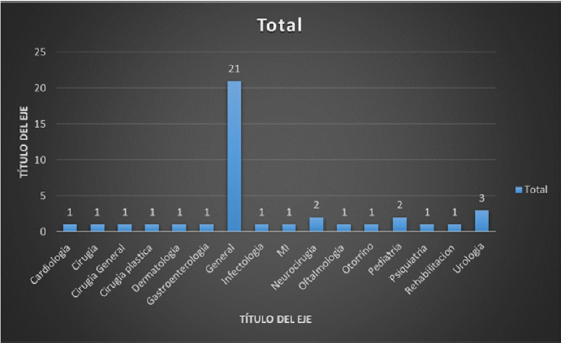
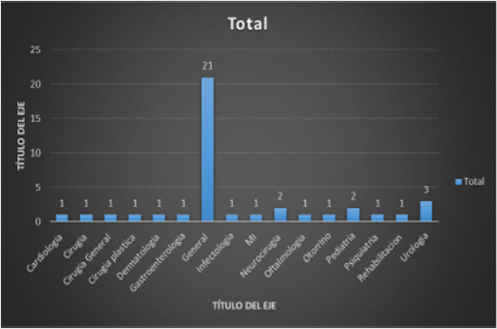
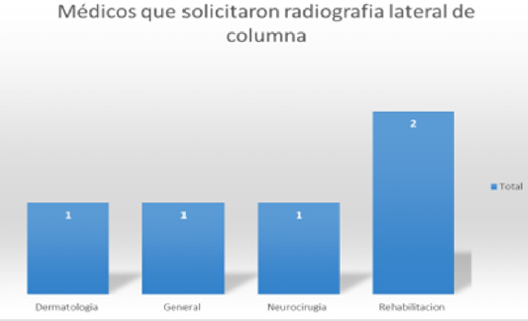
The approach of the tension headache is eminently clinical, but the cabinet studies will always be very important, focused mainly on the tomography of the skull, and even more on the lateral x-ray of the cervical spine, so forgotten, but so useful and demonstrative of the lesions that cause a headache, which should be addressed at the end of the day as a spinal problem.
References
>- (2007-2012) National Health Program, Secretary of Health.
- Levil L, Anderson l (1975) Psychosocial Stress: Population, Environment and Quality of Life New York: sp books division of spectrum publications, Mexico.
- Pain K, Dunn M Anderson G, Darrah J Kratochvil M (2004) Quality of Life: What Does It Mean in Rehabilitation Journal Rehabilitation, p.11.
- (1498) World Health Organization, Constitution of the World Health Organization.
- Guyatt GH, Feeny DH, Patrick DL (1993) Measuring Health-Related Quality of Life Ann intern med 118(8): 622-629.
- Rodríguez O, Rojas R (1998) La Psicología De La Salud En América Latina México: Miguel Ángel Porrúapps, p. 13-32.
- Jacobson AM, de Groot M, Samson JA (1994) The evaluation of two measures of Quality of Life in patients with type I and type II. Diabetes Care 17(4): 267-278.
- Boyer JG, Earp JAL (1997) The development of an instrument for assessing the quality of life of people with diabetes MedCare 35(5): 440-453.
- (1988) Diabetes Control and complications Trial research group Reliability and validity of Diabetes quality of life measure for the diabetes control and complication trial (DCCT). Diabetes Care 11(9): 725-732.
- American Diabetes Association (ADA) (2003) Expert Committee on the diagnosis and classification of DM. Diabetes Care 26(Suppl 1): 5-20.
- (2008) Programme, World Health Organization.
- (2001) Iniciativa de diabetes para Las Américas (DIA): Plan de acción para América Latina y el Caribe 2001-2006, División de prevención y control de enfermedades no transmisibles, Organización Panamericana de la Salud, Organización Mundial de la Salud, julio.
- (2008) Pan American Health Organization. "ALAD Guidelines for diagnosis, control and treatment of DM2" Washington, USA.
- Martínez FR Mávil L, Mendiola I (2001) Home amputation of toes in diabetic patients Rev Surgery and Surgeons. Volume 69.
- (2010) DOTA: Declaration of the Americas on Diabetes, Brochure Promoting Better Health for People with Diabetes.
- IDF, Atlas of DM, (5th edn).
- (2003) American Diabetes Association (ADA), Expert Committee on the diagnosis and classification of DM.
- Ministry of the Interior.
- Presentation of the impact of the DM from the Institutional perspective of Ernesto Álcantara Luna.
- (2008) National Center for the Prevention of Chronic Diseases and Health Promotion.
- Boyer JG, JAL Earp (1997) The development of an instrument for assessing the quality of life of people with diabetes. Med Care 35(5): 440-453.
- Patrick DL (1990) Bergner M Measurement of health status in the 1990. AnnRev Public Health 11: 165-183.
- Garrat AM, Schmidt L, Fitzpatrick R (2002) Patient-assessed health outcome measures for diabetes: A structured review. Diabet Med 19(1): 1-11.
- Watkins K, Connel CM (2004) Measurement of health related QOL in DM. Pharmacoeconomics 22(17): 1109-1126.
- Robles R, Cortàzar, J, Sànchez, S, Pàez, A, Nicolini S (2003) Evaluation of the quality of life in diabetes mellitus type II Psychometric properties of the Spanish version of DQOL. Psicothena 15(2): 247-250.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...