Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6628
Research Article(ISSN: 2637-6628) 
Mirror Mirror on the Brain; Tell Me What Do They Feel? Mirror Neurons; The Neural Wi-fi System for Affect Sharing Volume 2 - Issue 5
MMC Gabriel Miranda Nava1* and Nester Javier Escott Leyva2
- 1Head of the Neurology service, Mexico
- 2Undergraduate Internal Medicine, Mexico
Received: June 17, 2019; Published: June 24, 2019
Corresponding author: MMC Gabriel Miranda Nava, Head of the Neurology service, Regional Military Hospital of specialties of Guadalajara, Mexico
DOI: 10.32474/OJNBD.2019.02.000148
Abstract
The present work allows us to observe the quality of sleep and the respect of circadian cycles as very important factors in the development of multiple diseases and in various specialties, which affects therapeutic methods, both in outpatients and in hospitalized patients and the variety of symptoms that can be observed, through a method of surveys in a practical way, with the main objective of contributing in the awareness to treating physicians about the importance of sleep hygiene measures and their improvement in the quality of life of the patients [1,2].
Introduction
When trying to define the dream it is inevitable to differentiate the physiological characteristics in the good quality of sleep depending on the species, where it is a little simpler to enumerate the behavioral characteristics that are associated with the aspect of the dream and try to define it properly, where it can be associated with immobility and muscle relaxation, it is a reversible event (which differentiates it from other pathological states such as stupor and coma), decreased consciousness and reactivity to external stimuli and finally during sleep individuals acquire a stereotyped posture. The absence of sleep induces different behavioral and physiological alterations in addition to generating a cumulative sleep debt that eventually must be recovered. A tool that has been of vital importance for the study of sleep physiology is the electroencephalogram (EEG), which is the graphic and digital representation of the oscillations that show the electrical activity of the brain, to be recorded by electrodes placed in different regions of the head. During alert states while keeping the eyes closed on the EEG, oscillations of electrical activity are observed that are usually between 8-13 cycles per second, mainly in occipital regions (alpha rhythm). Within the dream, characteristic changes of brain activity occur. which are the basis for dividing the dream into several phases, where it is usually divided into two phases: without rapid eye movements, and with rapid eye movements [3].
Sleep NOT MOR
Phase N1 corresponds to drowsiness or the onset of light sleep, light arjerks are usually observed (acute vertex waves), phase N2 appear specific patterns of brain activity, called sleep spindle and complex k, heart rate and respiratory begins to decrease gradually, phase N3 or slow wave sleep is the deepest phase observed in the EEG very slow frequency activity (<2 Hz).
MOR Sleep
Now it is called the R phase and is characterized by the presence of rapid eye movements, physically all muscle tone decreases. A young adult spends approximately 70-100 min in non-MOR sleep, which can last between 5-30 min and this cycle is repeated every hour and a half throughout the night, therefore throughout the night they can be presented normally between 4 and 6 MOR sleep cycles [4].
Sleep hygiene Sleep hygiene measures are a series of recommendations about desirable behaviors and habits, as well as modifications of environmental conditions and other related factors, aimed at improving the sleep quality of people who already suffer from a sleep disorder such as insomnia, or that can be used as measures to prevent a sleep disturbance. Although there is no global consensus about what these sleep hygiene measures should be and some of these sleep hygiene measures are transplanted with some forms of non-pharmacological behavioral treatment we can generally consider (avoid prolonged naps> 1 hour, lie down to sleep at the same time every day, wake up at the same time all day, sleep in a comfortable bed, sleep in a room with low lighting and little ambient noise). Epidemiology It is estimated that, in our country, around 45% of the adult population has poor sleep quality [5,6]. The above is reflected in the difficulty that people must get up, as well as in constant drowsiness and fatigue during the first hours of the morning.
Methods
The present study uses the referential method as a basis, mentioning descriptive surveys, and testing the Pittsburgh quality of sleep scale in which 20 hospitalized patients are evaluated in the Regional Military Hospital of Specialties of Guadalajara, Jalisco, assessing the level of quality of sleep and what concomitant symptoms are added by poor sleep hygiene, February-May trial period. Justification The present investigation will focus on studying the hygiene habits based on the quality of sleep in hospitalized patients, since due to work stress or in hospital instances it has been seen that patients have directly modified their sleep habits, worsening the quality of life and By delaying the recovery in the hospital by increasing concomitant symptoms, we propose then to investigate the evolution of the pathological patterns and their aggregate symptoms; the reasons that led us to investigate the quality of sleep in hospitalized patients are due to the increase in discomfort or somnolence data reported by patients after staying more than 2 days in hospital. We think that by means of the detailed analysis we will be able to make the health personnel aware to improve the hygiene of the sleep, thus helping the quick recovery without appearance of concomitant symptoms in the patients who are hospitalized.
Methods
The present study uses the referential method as a basis, mentioning descriptive surveys, and testing the Pittsburgh quality of sleep scale in which 20 hospitalized patients are evaluated in the Regional Military Hospital of Specialties of Guadalajara, Jalisco, assessing the level of quality of sleep and what concomitant symptoms are added by poor sleep hygiene, February-May trial period. Justification The present investigation will focus on studying the hygiene habits based on the quality of sleep in hospitalized patients, since due to work stress or in hospital instances it has been seen that patients have directly modified their sleep habits, worsening the quality of life and By delaying the recovery in the hospital by increasing concomitant symptoms, we propose then to investigate the evolution of the pathological patterns and their aggregate symptoms; the reasons that led us to investigate the quality of sleep in hospitalized patients are due to the increase in discomfort or somnolence data reported by patients after staying more than 2 days in hospital. We think that by means of the detailed analysis we will be able to make the health personnel aware to improve the hygiene of the sleep, thus helping the quick recovery without appearance of concomitant symptoms in the patients who are hospitalized.
Goals
a) Clinically observe the behavior of hospitalized patients and their quality in sleep hygiene.
b) Intervening and preventing concomitant pathologies that are associated with poor hygienic sleep habits.
c) Improve the quality of life of hospitalized patients.
d) Awareness of the application of hygiene or good sleep habits to improve the quality of life.
e) Decrease the percentage of symptoms added by decrease in sleep schedules. 6. Locate key events or outstanding problems in the quality of sleep.
Statistical Population
Sampling was carried out where people of both sexes were chosen, who underwent a descriptive evaluation by means of direct surveys, where a sample of 20 people with characteristics with a simple random election type was collected, making a list of participants hospitalized to form the sample to be studied by means of questionnaires.
Results
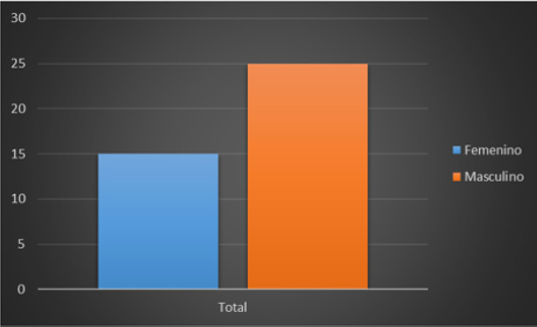
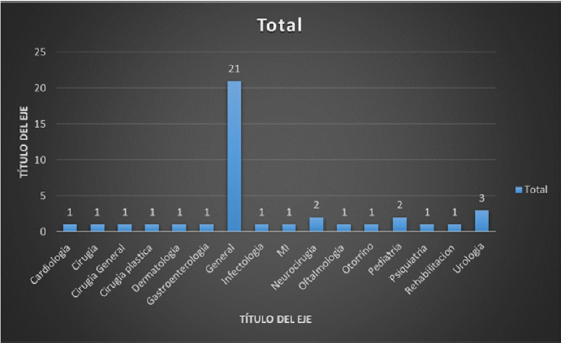
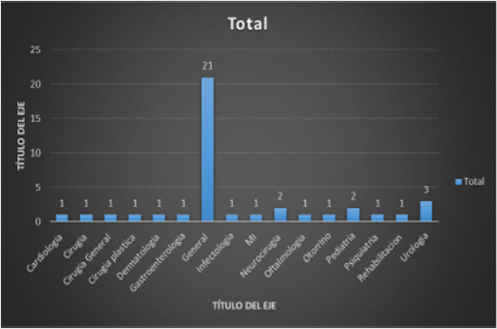
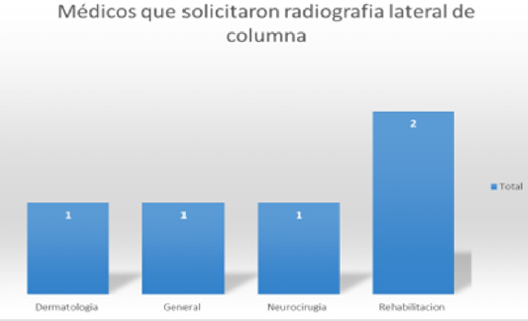
A random sample is taken to carry out descriptive direct surveys at the Regional Military Hospital of Guadalajara, Jalisco, where 14 people of the female sex and 6 of the male sex are taken, having a percentage of 70% female and 30% male. Regarding age, there is an ambiguous percentage where it is observed that 30% corresponds to people between 21 and 30 years of age following proportionally 15% of patients aged 31 to 73 years (Figure 1). In the marital status 74% of the respondents are married, 11% are single, and 15% are proportionally divorced, widowed and in free union (Figures 1 & 2). The descriptive surveys did not take into account the situations of right-of-way in the institution where the majority of those interviewed or those who were interviewed were the rightful claimants in the asset, having the majority percentage with 60% followed by military personnel in the asset where it was noted that most of the concomitant symptoms corresponded to anxiety and headache (Figure 3).
Among the key questions that are characterized in the scale of Pittsburgh manifested bedtime where literally 50% of the patients interviewed reiterated to sleep at around 10:00 pm and 11:00 pm, while the rest were distributed with 25% who go to bed regularly from 08:00 pm to 09:00 pm and the other 25% after 12:00 pm (Figure 4). Continuing with the variability of sleep habits, the question about the total time it takes to sleep is indispensable, where a detailed variability between each point and constant was obtained, obtaining as a result that 45% of the studied population reconciled the sleep within the first 10 minutes, while 25% is distributed in patients who sleep within the first 30 minutes and an important fact is that 15% of patient samples last more than 60 minutes to fall asleep (Figure 5).
It should be noted the relevance of the time that people take to sleep and the time they have to get up, since it should be noted that within the quality of sleep it is known that a young adult should sleep an average of 7-8 hours, although This amount may vary because it depends on internal factors of the organization and external society, so a preschool child can sleep between 11 or 12 hours and an older adult between 5 and 6 hours not taking into account the periods that doze during the day , so the results are very important in which the percentages of patients who wake up early and sleep late are focused as they begin to have functional and organic damages that are involved in their daily life. Within the Pittsburgh scale it is essential to highlight and highlight the following two patterns:
a) The time when patients regularly wake up from their dreams
b) The total hours of sleep of a patient. Where the results taking as supremacy that 40% of the studied population wakes up at 7:00 am while the other 40% wakes up on an average between 5:00 and 6:00 am to perform their activities, finally 15% It has a short sleep average waking up between 3:00 and 4:00 am (Figure 6).
Performing and observing an average within the sleep habits and the quality of sleep of the patients a question is asked to evaluate the amount of hours that people sleep approximately, taking into account their basic pathologies (post-operative, chronic pathologies) degenerative, concomitant pathologies), with the result that 45% of patients only sleep 5 to 6 hours in a row compared to the time a person really has to sleep to refer adequate quality and hygiene of sleep is really low of established parameters, while around 15% of the patients who were taken as a sample sleep an average between 10 and 15 hours a day, it should be noted that these patients mentioned having psychological and psychiatric problems as depression, if we recapitulate the concepts offered by the national sleep foundation 85% of the patients interviewed do not meet the criteria to define that they maintain a to adequate sleep health, while only 5% of patients could enter the criteria already established and mentioned (in the following graph represents the number of patients and the total sleep hours they maintain for a day) the scale of Pittsburgh are observed questions which are worth mentioning that are subjective processes that take relevance in the last 4 weeks, about falling asleep where 45% of hospitalized patients answered that approximately three times a week they are prevented from falling asleep. a proper way [7].
And evaluating the number of people and how many times they get up during the night, results were obtained that 14 people of the interviewed women get up between 2 and 3 times a week, which is about 70% of the patients surveyed with those bad sleep habits. Regarding the reasons why patients wake up, the following result was obtained. Where 65% of respondents in the last month would not have suffered from feelings of shortness of breath, while the number of 6 people reported that three times in the week are awakened by feeling a sense of shortness of breath corresponding to a 30% of the sample investigated. When asking indirect questions about whether his family member snored 40% answered that they did not catch such events in the last 4 weeks while 45% answered that on average 1-2 times per week they snored at night what they did the patient will wake up during the night, 50% of patients have not woken up during the night due to cold in the last 4 weeks, and with a total of 5 patients it gives a result of 25% who woke up at least once a week due to cold sensation. Otherwise, 70% of patients used to wake up during the night due to the sensation of heat. 35% of the patients surveyed had as a result that they have not had problems like nightmares at bedtime, while the other 35% have nightmares 1 or 2 times a week, 30% 3 times a week; The following graph is representative of the results obtained when applying that question to the sample that was investigated [8].
Among the data that we want to highlight in this study is the presence of pain and of what type in the last 4 weeks, referring to pain as some event that keeps them awake or that awakens them during the night, having as conclusion that the 30 % of the patients interviewed answered affirmatively that approximately once a week felt pain, and 35% mentioned that approximately twice a week felt some type of pain. Putatively evaluating the data provided by the patients, it was obtained that 70% of the hospitalized patients have presented tension headache caused by bad habits or sleep hygiene, adding lumbago and even anxiety in a total of 5 more patients that correspond another 25% more of the sample studied. 50% of the patients rated their sleep quality as bad, while 35% rated it as a good sleep, He was asked if they took any medication or taken in the last 4 weeks to be able to fall asleep, where 75% denied having taken medication to fall asleep. While the other 25% agreed to have ingested medication to be able to sleep either 1 to 3 times per week [9].
The unanimous medication that 25% of patients used is clonazepam which is a benzodiazepine that acts directly on the central nervous system, which can create drowsiness and fatigue. Within the study of sleep hygiene there is variability where it focuses directly on factors such as drowsiness that is directly caused by poor sleep hygiene habits, based on the Pittsburgh scale there is a direct section where questions about the drowsiness that the patient could suffer and finally if that drowsiness or fatigue could prevent the accomplishment of some daily activity, or executive in the day to day. Having as a result that 65% of patients have been in a drowsy status or have felt tired in an approximate period of between two times to three times a week, while only 25% of patients have drowsiness due to at least once a week, preventing their early recovery or decreasing their resistance in everyday life [10]. Taking into account the number of patients who answered affirmatively to the question about sleepiness, a graph was obtained showing the results in which the disability or problem that caused the maintenance of that drowsiness status was shown, obtaining that 35% of the patients do not have no problem when carrying out their daily activities, while another 35% of the people surveyed expressed their concern and described as a slight problem in their daily lives the maintenance of somnolence data which can cause difficulties in their daily life; Finally, 25% classified their level of sleepiness as a moderate problem, defining that in daily activities it is a conflict to be able to perform them with the greatest aptitude and energy.
Conclusion
The great problem of health to solve in our country necessarily has to do with habits and because, by not respecting the hours of sleep, biorhythms are altered that result in clinical problems such as: headache, nervous colitis, depression, anxiety, metabolic and systemic problems. It is important to understand the reeducation to our patients in each consultation and sanitary step, since the installation of an adequate diet and weight control, as well as a healthy and aerobic sport together with the sleep hygiene measures will be the main weapons to attack diverse diseases in our times.
References
- Lluesma Vidal M, Murgui Pérez S, Carmona Simarro JV (2019) Nutritional status regarding the quality of life and sleep pattern in community-dwelling older adults with cognitive dysfunction. Nutr Hosp 36(2): 303-308.
- Garrigós Pedrón M, Segura Ortí E, Gracia Naya M, La Touche R (2019) Predictive factors of sleep quality in patients with chronic migraine. Neurologia 4853(19): 30014.
- Serrano Guzmán M, Valenza Peña CM, Serrano Guzmán C, Aguilar Ferrándiz E, Valenza Demet G, et al. (2016) Effects of a dance therapy programme on quality of life, sleep and blood pressure in middle-aged women: A randomised controlled trial. Med Clin (Barc) 147(8): 334-339.
- Abad Massanet F, Rivero Pérez J, Vera Osorio JA (2015) Differences in health-related quality of Life between men and women with sleep-disordered breathing. Semergen 41(8): 407-142.
- Cruz T, García L, Álvarez MA, Manzanero AL (2019) Sleep quality and memory function in healthy ageing. Neurologia 4853(19): 30003-30009.
- Escobar Fernández L, Coccolo Góngora A, Vázquez López M, Polo Arrondo AP, Miranda Herrero MC, et al. (2019) Continuous spike-waves during slow-wave sleep: Experience during 20 years. An Pediatr (Barc) 4033(19): 30021-30029.
- Abbott SM, Weng J, Reid KJ, Daviglus ML, Gallo LC, et al. (2019) Sleep Timing, Stability, and BP in the Sueño Ancillary Study of the Hispanic Community Health Study/Study of Latinos. Chest 155(1): 60-68.
- Félix Amaro (2019) Trastornos del sueño en la infancia y la adolescencia.
- Paul Carrillo Mora, Jimena Ramírez-Peris, Katia Magaña Vázquez (2013) Neurobiology of the dream and its importance: anthology for the university student. Journal of the Faculty of Medicine (Mexico) 26(4).
- Sierra J, Delgado Domínguez C, Carretero Dios H (2009) Influence of Sleep Quality On Psychopathological Variables: A Comparative Analysis Among Workers Submitted To Turnos and Employees with Normal Schedules. Latin American Journal of Psychology 41(1): 121-130.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...