Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6628
Research Article(ISSN: 2637-6628) 
Image Guided Brain Surgery (Neuronavigation) In Annapurna Neurological Institute and Allied Sciences, Nepal: Retrospective Study on Role and Effectiveness of Neuronavigation Volume 6 - Issue 4
Basant Pant2, Sambardhan Dabadi B E1*, Raju Raj Dhungel B E1, Pritam Gurung2, Resha Shrestha2, Samir Acharya2, Pravesh Rajbhandhari2, Pranaya Shrestha2 and Sudan Dhakal2
- 1Department of Biomedical Engineering, Annapurna Neurological Institute and allied Sciences, Nepal
- 2Department of Neurosurgery, Annapurna Neurological Institute and allied Sciences, Nepal
Received: October 17, 2022; Published: November 28, 2022
Corresponding author: Sambardhan Dabadi Department of Biomedical Engineering, Annapurna Neurological Institute and allied Sciences, Nepal
DOI: 10.32474/OJNBD.2022.06.000242
Abstract
Introduction
In recent years, neurosurgery has seen great advancement owing to the development of the image-guided interactive system. The introduction of neuro-navigation system has been a great leap to improve the quality of neurosurgery. With an aim to investigate the role of navigation system on cranial surgeries, cases performed with the assistance of Easy Nav navigation system, a newly introduced system through gaming hardware and software for the first time has been reviewed. Materials and Methods: 500 cranial surgeries performed with guidance of navigation within the period of 2017 to 2021 were analysed and the surgical outcome, effectiveness were studied. Out of all cases 71% were brain tumour, 4% vascular anomalies, 15% pituitary tumour and remaining were intra-cranial bleed, and cysts. Results: The studies concluded EasyNav navigation to be effective in localizing the lesions, reducing exposure areas, less harm to normal brain tissue and overall decreased surgical time. Navigation proved to be effective in various surgeries irrespective of site, size, consistency and vascularity. However slight off target indication were seen on few surgeries performed on prone position especially in posterior fossa. Conclusion: Easy Nav neuronavigation system proved to be an affordable, easy, straight forward optical tracking-based navigation system, whereas other navigation system are too expensive for the developing countries like Nepal. The navigation system has helped surgeons to locate lesions on difficult sites and in deep brain structures. Mini-craniotomy, complete resection, better localization of the lesion with the guidance of navigation has helped in uplifting the overall outcome of cranial surgeries.
Keywords: Aneurysm; CT; Lesions; MRI; Navigation; Optical Tracking
Introduction
Accuracy and the areas exposed during any surgical procedure determines the post-operative condition of the patient [1]. In order to increase the accuracy and pinpoint the lesions, different techniques have been introduced. Endoscopes, laparoscopes have been extensively used in gastro-intestinal surgeries whereas fluoroscopic and minimally invasive procedures in cardiac surgeries are some of the popularly used technologies. In the cranial surgeries, neuronavigation or the frameless stereotactic system has been introduced as one of the newest technologies in this field. The recent technological advancement have been widely explored in the field of neurosurgery as the surgeons quest to treat the abnormalities in delicate and tightly organized brain structure is always a tedious and complicated task. The advanced technological leap has uplifted the quality of the surgery and hence improved patients’ post-operative lifestyle with minimal or no deficit [2]. Neuronavigation has provided the surgeons the add-on benefit to locate, determine the size of tumour and analyse the trajectory for excision of lesion before starting the surgical procedure [3]. Such advantage to surgeons has led to increase in success rate of the surgery and less harm to the normal brain tissue leading to decreased post-operative complications and weakness to patients [4].
However, before 1970s, in early ages of neuro imaging system, such facilities were unavailable. Later in the year 1987, the first image guided surgical technology was developed at University of Oulu, Finland, which used pre-operative magnetic resonance imaging (MRI) and intra-operative ultrasound imaging to locate the brain lesions [5]. Later, advanced technologies incorporating, optical tracking, magnetic tracking system were introduced. Optical tracking system requires a computer, an infrared camera, and tracker, where the tracker needs to be in the visual field of camera [6]. On the other hand electromagnetic system has a magnetic field generator system which detects the tracker within the range of magnetic field thus omitting the need of tracker to be in line of sight [7]. With the use of advanced navigation system, complex brain tumours, aneurysms and other neurosurgical procedures are being achieved with small and well centred skin incision, craniotomy and trajectory to approach the lesion/defect with minimal injury and dissection of normal brain tissue. The primary aim was to study the usefulness and effectiveness of the cranial navigation system.
Materials and Methods
With the aim to study the usefulness and effectiveness of cranial navigation system, more than 500 cases who underwent various neurosurgical procedure at Annapurna Neurological Institute and Allied Sciences, Kathmandu were analysed prospectively. The data of the patient from the period of January 2017 to December 2021, who had been operated with the assistance of neuronavigation system were studied. A commercially available optical trackerbased navigation system, EasyNav, developed by Happy Reliable Surgical (HRS) was used for the intra-operative guidance. The system consisted of a navigation camera, a portable computer workstation with navigation software, a dynamic tracker and a handheld probe. Either a Computed Tomography (CT) or MRI imaging was taken under the navigation protocol (DICOM image including tip of the nose to the vertex) was taken pre-operatively. The images were loaded to the navigation software and the easily noticeable and known points on the patients face such as lateral and medial canthus, philtrum were set as landmarks. Once the patient was anesthetized and head was fixed with three-pin holder. The dynamic tracker was attached to the three-pin holder facing the navigation camera. With one of the multiple handheld probes available, the points previously set as landmarks were pointed out and matched, which is known as the process of registration. Once the registration was completed, the system will be then ready for navigation and displays the 3D image (axial, sagittal and cranial view) of the region where the surgeon points their handheld probe to, which thus helps to locate the tumour/lesion and determine the easiest and safest trajectory. The data from more than 500 cases were analysed based on various factors like surgical procedure, location, position and images used for the procedure.
Results
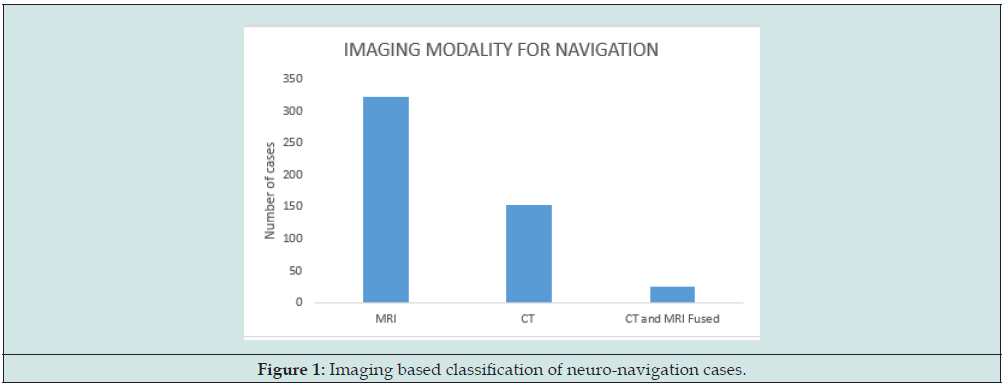
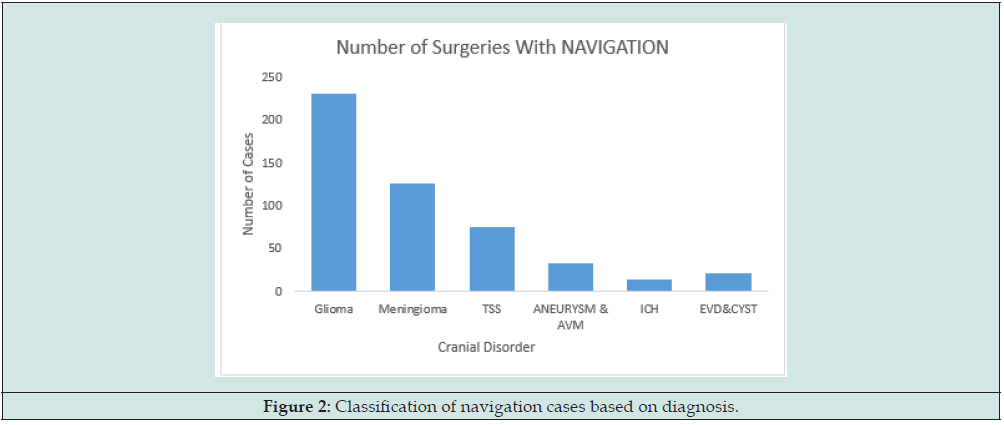
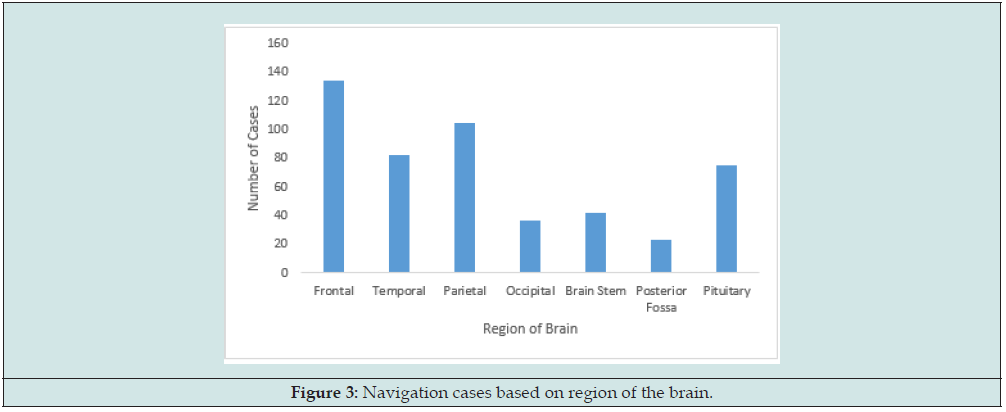
Among the 365 cases studied, 322 cases were based on MRI imaging, 153 with CT imaging and 25 cases included, the CT and MRI fused images (Figure 1). The image fusion method was in built within the navigation software. Out of the total cases analysed, 46% were glioma, 25% were meningioma, 15% pituitary macro adenoma carried out via trans-sphenoidal approach, 7% aneurysm or vascular malformations, 4% cyst and epi-ventricular drain (EVD) placement, 3% Intra Cranial Haemorrhage (ICH) (Figure 2). All the cases performed with the assistance of navigation, led to total excision of space occupying lesion (SOL), easier and efficient tracking of aneurysm and vascular malformations. The subjective analysis concluded a decrease in operative time when the navigation was used for the excision of tumour in similar site, size, vascularity and consistency. The use of navigation based on the surgical site was also carried out, which revealed, on 134 cases the tumour or lesion was on frontal lobe, 82 cases in temporal lobe, 75 cases in pituitary i.e. Trans-sphenoidal surgery (TSS), 105 cases in parietal, 37 in occipital and 23 in posterior fossa. While 42 cases included were at the deep brain structures such as thalamus, basal ganglia or brain stem (Figure 3). The results showed the navigation proved to be efficient in all cases irrespective of the location. However, the accuracy of the target was not perfect in prone position and the location of the lesion was on occipital lobe and in posterior fossa. Besides, these limitations the navigation system proved to be of great assistance in surgeries with supine position of patient. Few of the illustrative cases have been discussed here in this paper to highlight the uses and efficiency of neuronavigation system in cranial surgeries.
Illustrative Cases
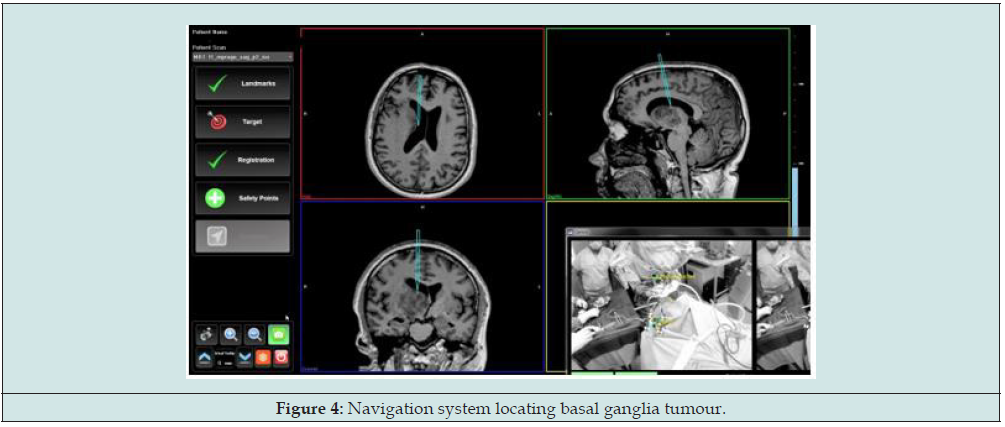
Case I: Basal Ganglia Mass
A 48-year-old man presented to our center with a major complaint of insidious onset of headache for 15 days. However, the headache was not associated with loss of consciousness (LOC), rather he had few episodes of vomiting. The MRI of head revealed a lesion over the basal ganglia and was advised for surgery. The surgery was performed with the assistance of neuronavigation. The patient was placed in supine position and the tumor was approached through the parietal region. With the guidance of navigation, minimal skin incision was done. Small craniotomy was done, and tumor was resected completely with minimal harm to the adjacent brain tissue. Boundaries of the tumor was accurate with respect to the navigation system (Figure 4).
Case II: Aneurysm
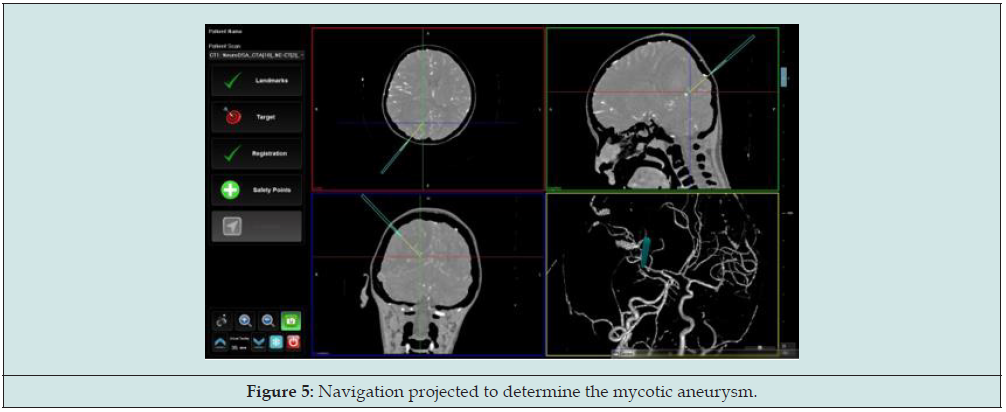
12-year-old boy, presented with sudden onset of severe headache followed by consciousness disturbances. He was immediately taken to another hospital, where CT scan of the head revealed a lesion over right parietal-occipital region, further evaluation with CT angiogram was done, which revealed the fusiform dilatation of P4 segment of right posterior communicating artery (PCA). He was then referred to our centre. On arrival his consciousness was drowsy without any focal neurological deficit. With the provisional diagnosis of PCA aneurysm, he was operated under the guidance of neuronavigation. During surgery patient was placed in semi prone position, the process of registration was conducted as per navigation protocol. The trajectory was preplanned with navigation (Figure 5). The navigation was on target with error less than 1mm, accurate targeting helped locating and clipping of the aneurysm efficiently.
Case III: Meningioma
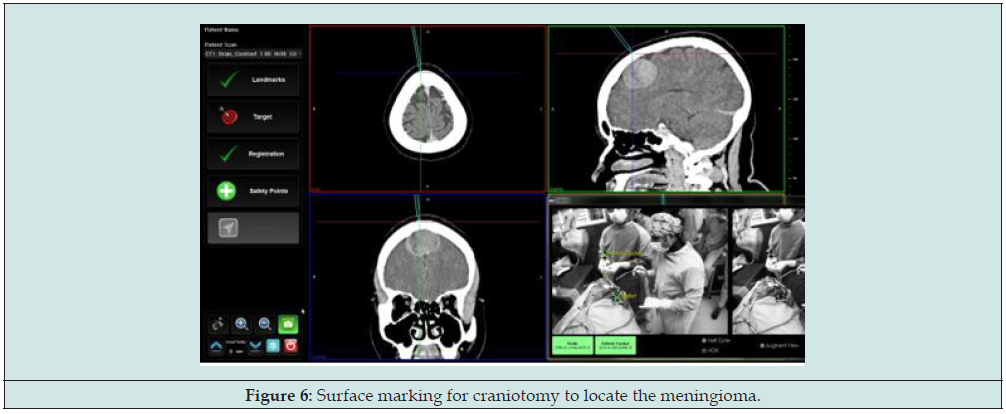
A 38-year-old woman presented to our centre with headache over the parietal and occipital region for two months. The headache was insidious onset but was not associated with vomiting or LOC and any other symptoms. She was advised for MRI and the images showed a well-defined lesion over the right parafalcine region. The lesion likely to be parafalcine meningioma, she was planned for craniotomy and excision of tumour under neuronavigation. The patient was placed in supine position with head slightly flexed. Registration for navigation was done and tumour boundaries were then marked out. Skin incision was made and a small craniotomy just covering the edges of tumour was done. The tumour was accurately pointed out by navigation and total excision was achieved with minimal skin incision and craniotomy (Figure 6). The surrounding brain tissue were almost untouched and no any postoperative complication were seen.
Case IV: Pituitary Macro Adenoma
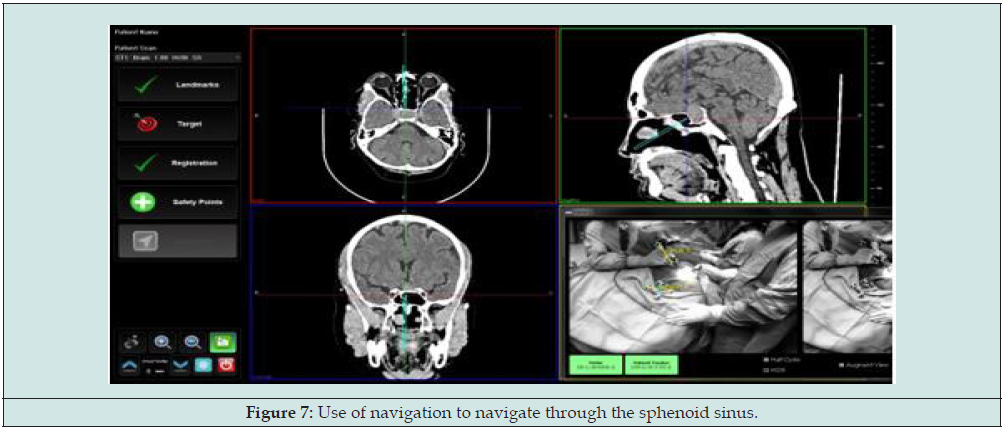
A 49-year-old man visited to our hospital with headache in posterior occipital area. The headache persisted for 5-6 hours along with dizziness and difficulty of vision. For evaluation CT scan of head was performed, where a mass of size approximately 26*25*25mm was observed at sellar region extending up to suprasellar region which was compressing the optic chiasma. With the diagnosis of pituitary macro adenoma, he was suggested for trans-sphenoidal surgery. The patient was placed in supine position with neck extended and lesion was approached through the right nasal septum. With the guidance of navigation it was easier to locate the complex bony structures, sinuses and lesion even though the point of entry was too small (Figure 7). The total resection of tumour was done and patient was free of pre-operative symptoms.
Case V: EVD Placement
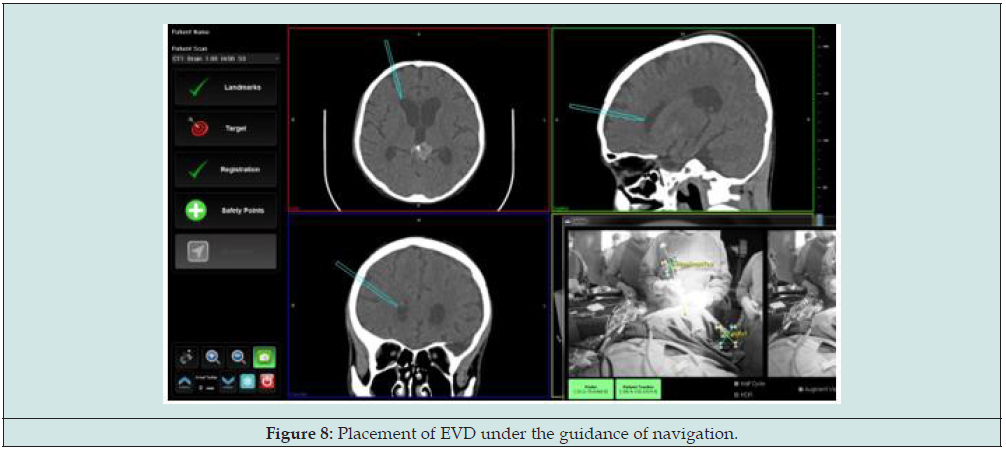
An 18-year-old boy, presented with sudden onset of severe headache and consciousness disturbances. CT scan of head showed pineal bleed and hydrocephalus. He was referred to our centre for further treatment. Then, he was planned for placement of EVD and removal of hematoma. The navigation guided EVD placement procedure allowed the surgeons to easily locate the anterior horn of lateral ventricle and the projection of path via navigation software helped the surgeon to predict the shortest and safest path (Figure 8). However, after the placement of EVD and draining around 10ml of cerebro-spinal fluid (CSF), the navigation got off target as the brain got relaxed and shifted as the CSF was released. Thus, the accuracy of locating the bleed was not achieved successfully through navigation, which however was detected visually through microscope.
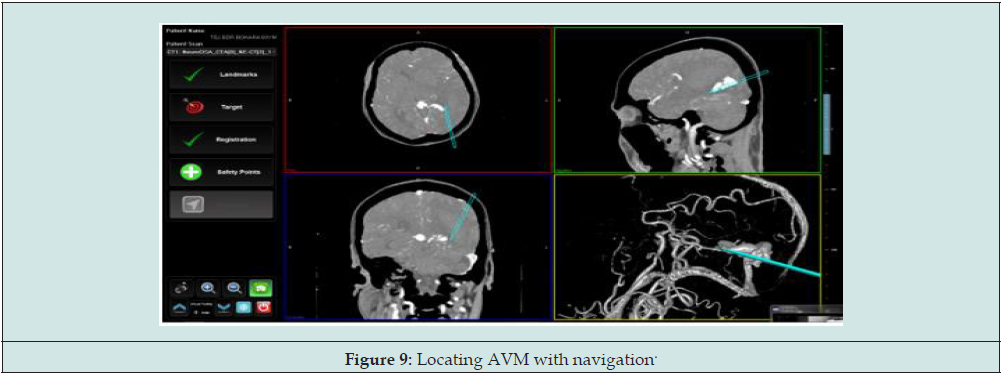
Case VI: Arterial-Venous Malformation (AVM)
A 64-year-old man with chief complaint of headache associated with nausea and vomiting was referred to our institute from the other centre. Initially diagnosed as probable tumour bleed or AVM bleed, he was admitted to our hospital for further management. On CT angiogram of head, the AVM at the occipital lobe was diagnosed and was planned for craniotomy and excision of AVM under navigation. The surgical procedure was done in prone position. The registration procedure for navigation was completed and craniotomy was done. With the help of navigation it was easier to identify the region of bleed. Furthermore, the use of digital subtraction angiogram (DSA) image for navigation, the feeders and draining vessels were able to be visualized during the surgery (Figure 9). This allowed the surgeons to approach the AVM, identify its feeder vessels and preserve the draining veins till the end. Accurate identification of feeder helped to reduce the intraoperative bleed and other complications.
Discussion
Based on the results of the study, neuronavigation provided positive surgical outcomes and was found particularly effective in brain tumors with difficult approaches and critical anatomical structures nearby. Many studies have been performed to determine the accuracy and reliability of the frameless stereotactic system on cranial surgeries. All of the studies revealed the frameless system to be as accurate as the framed stereotactic system [8- 10]. However, the frameless navigation system being dependent on manual registration, error of few millimeter can be observed in few cases, hence it is not suitable for procedure like deep brain stimulations [11]. With better targeting of the lesions and vascular malformations while using the neuronavigation system, no significant comorbidities related to surgical procedure was seen. On average the hospital stay of the patient with surgical procedure done with navigation was around 10 days, which suggests the lesser harm to normal tissue. The precise targeting was accompanied by minimal craniotomy or cortectomy, which led to lesser surgical time and anesthetic doses were reduced significantly. This eventually had less after effect on patient and early recovery from anesthesia [12].
Neuronavigation was equally significant in the case of TSS and posterior fossa, however in some cases of posterior fossa and prone approach around 3-5mm off target were observed. This was identified as the error occurred due to CT and MRI being done in supine position, while registration for navigation had to be done in prone position [13]. The other reason was probably due to difficulty in patient registration as the landmarks were quite hard to locate in prone position. Such errors were minimized by slight change in registration procedures. Taking the landmarks as bony projections of mastoid had helped in increasing the accuracy in case of prone surgeries. Furthermore, the navigation came out to be beneficial in epilepsy surgeries as well. Some studies have also illustrated its potential role in epilepsy in localizing the hippocampus and in corpus callosotomy [14]. In relation to this, we have done 25 cases for seizure disorder under navigation guidance and found neuronavigation to be beneficial in identifying the important cranial structures.
The ability of navigation system to freeze the image, project the probe length to measure the estimated distance between the point of tracker placement to the lesion, able to record images (snapshots) has made it even more user friendly and effective during the surgeries. However, certain technical drawbacks are to be mentioned which makes the use of EasyNav neuronavigation below perfect. The use of infrared camera and tracker, one of the optical navigation system, movement of the surgeon and staff is restricted, microscope has to be momentarily moved to maintain an uninterrupted line of sight between the dynamic frame reference, tracker and camera. Though, new camera system with better tracking abilities have been introduced, these still need to maintain line of sight between camera and tracker. The head position has to be kept fixed once the image registration process completes and cannot be changed during the surgery even if the surgeon finds that position to be less convenient afterward. Due to unavailability of real-time imaging system, this neuronavigation system was not much effective if there was brain shift during surgery.
Conclusion
With all these observations, the EasyNav neuro-navigation system is simpler, accurate, reliable and affordable navigation system. The navigation system has helped in locating and tracking the tumor at few quiet difficult sites. The use of navigation for various surgeries during the mentioned time period in this institute has helped enhance the quality of surgery in terms of total resection, minimal invasion and less damage to the brain tissue, thereafter, reducing the post-operative complications and deficits.
References
- Orringer DA, Golby A, Jolesz F (2012) Neuronavigation in the surgical management of brain tumors: Current and future trends. Expert Review of Medical Devices 9(5): 491-500.
- Mezger U, Jendrewski C, Bartels M (2013) Navigation in surgery. In: Langenbeck’s Archives of Surgery 398(4): 501-514.
- Roberts DW, Strohbehn JW, Hatch JF, Murray W, Kettenberger H (1986) A frameless stereotaxic integration of computerized tomographic imaging and the operating microscope. J Neurosurg 65(4): 545-549.
- Li F, Lin J, Zhu G, Meng H, Wu N, et al. (2011) Neuroimaging and functional navigation as potential tools to reduce the incidence of surgical complications of lateral ventricular meningiomas. Clin Neurol Neurosurg 113(7): 564-569.
- Hiffbauer HS (1999) Clinical beta-phase of the Oulu Neuronavigator System 505: 1-159.
- Cleary K, Peters TM (2010) Image-guided interventions: Technology review and clinical applications, Annual Review of Biomedical Engineering. Annu Rev Biomed Eng 12: 119-142.
- Mascott CR (2005) Comparison of magnetic tracking and optical tracking by simultaneous use of two independent frameless stereotactic systems. Neurosurgery 57(4): 295-301.
- Spivak CJ, Pirouzmand F (2005) Comparison of the reliability of brain lesion localization when using traditional and stereotactic image-guided techniques: A prospective study. J Neurosurg 103(3): 424-427.
- Miller K, Joldes GR, Bourantas G, Warfield SK, Hyde DE, et al. (2019) Biomechanical modeling and computer simulation of the brain during neurosurgery, International Journal for Numerical Methods in Biomedical Engineering. Wiley-Blackwell 35(10): 3250.
- Dorward NL, Alberti O, Palmer JD, Kitchen ND, Thomas DG (1999) Accuracy of true frameless stereotaxy: In vivo measurement and laboratory phantom studies: Technical note. J Neurosurg 90(1):160-168.
- Bjartmarz H, Rehncrona S (2007) Comparison of accuracy and precision between frame-based and frameless stereotactic navigation for deep brain stimulation electrode implantation. Stereotact Funct Neurosurg 85(5):235-242.
- Khoshnevisan A, Allahabadi NS (2012) Neuronavigation: Principles, clinical applications and potential pitfalls. Iran J Psychiatry 7(2):97-103.
- Dho YS, Kim YJ, Kim KG, Hwang SH, Kim KH, et al. (2020) Positional effect of preoperative neuronavigational magnetic resonance image on accuracy of posterior fossa lesion localization. J Neurosurg 133(2): 546-555.
- Golfinos JG, Fitzpatrick BC, Smith LR, Spetzler RF (1995) Clinical use of a frameless stereotactic arm: Results of 325 cases. J Neurosurg 83(2): 197-205.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...