Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6628
Short Communication(ISSN: 2637-6628) 
Global Suicide Rate Among Youngsters Increasing Significantly Volume 3 - Issue 5
Bahman Zohuri1* and Siamak Zadeh2
- 1Electrical Engineering and Computer Department, University of New Mexico, New Mexico, USA
- 2Golden Gate University, Ageno School of Business, San Francisco, USA
Received: March 05, 2020; Published: March 17, 2020
Corresponding author: Bahman Zohuri, Electrical Engineering and Computer Department, University of New Mexico, Albuquerque, New Mexico, USA
DOI: 10.32474/OJNBD.2020.03.000175
Abstract
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
Suicide is a key health concern and a major cause of death among persons aged 10 – 24 years in the United States. In 2017, suicide was the second leading cause of death among this group and from 2007 to 2018, the suicide rate increased 56% among those aged 14 – 19 years. Overall, among teenagers 12 – 19 years, suicide is the third leading single cause of death, after accidents (unintentional injuries) and homicides. According to the latest World Health Organization (WHO), suicidal behavior is also a major health concern in many countries, developed and developing alike. Nearly 800,000 are estimated to die annually from suicide worldwide. Many more, particularly the young and the middle-aged individuals, attempt suicide. In this paper, it is suggested that modern technology plays a significant role in the increase in the rate of suicide among the youths. It is suggested that increasing engagement with social media, driven by new generation of electronic gadgets and smart phones, is an important factor behind the increase in the rate of suicides. Heavy usage of smart phones, such as texting, twitting, or having some other forms of engagement through social media, is a contributing factor.
Keywords: Depression; Suicide Attempt and Suicide Rate; Youngsters; Suicide Risk Management; Augmentation of Artificial Intelligence in Depression Treatment
Introduction
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
Suicide is a major public health problem and a leading cause
of death among the persons 10 – 24 years in the United States.
The effects of suicide go beyond the person who acts to take his or
her life. It can also have a lasting effect on family, friends, and the
public at large. The suicide attempts among youth and youngsters
between age of 14 to 30, globally has been increasing in recent
years. According to the statistics, there is a shocking rise in suicide
attempts among youngsters. In fact, between 2000 and 2007, the
suicide rate among youth ages 10 to 24 hovered around 6.8 deaths
per 100,000 people. Then, the rate curved upward, reaching a rate
of 10.6 deaths per 100,000 by 2017 — a 56-percent increase in less
than two decades. The suicide rate among people ages 10 to 24
years old climbed 56% between 2007 and 2017, according to the
report from the Centers for Disease Control and Prevention. The
rate of homicide deaths decreased by 23% from 2007 to 2014 but
then increased by 18% through 2017 [1].
Violent death, including homicide and suicide, is a major cause
of premature death for the age group. Around 2010, the death rate
of suicides among adolescents and young adults surpassed the rate
of homicide deaths, according to the report. Suicide was the secondleading
cause of death among 10- to 24-year-olds in 2016, up from
third place in earlier years, according to the Centers for Disease
Control (CDC) and Prevention [1].In this context, the researchers
are calling for more study of possible gender differences in youth
mental health, noting previous findings of a larger rise in depression
in teenage girls compared with boys in the decade leading up to
2014. One of the main and major cause of suicide attempt among is
the Impact of “Technology on Mental Health” among these youths
[2,3].
In a nutshell, Mental health refers to our cognitive, behavioral,
and emotional wellbeing - it is all about how we think, feel, and behave. The term ‘mental health’ is sometimes used to mean
an absence of a mental disorder. Neurological disorders with
symptoms such as chronic pain, depression, and insomnia are
widespread. Very weak electric fields applied through the skull
can enhance or diminish neural activity and modulate brain waves
in order to treat many of these common medical problems. This
approach is to be contrasted with well-established pharmacological
methods or more recent invasive electrical Deep Brain Stimulation
(DBS) techniques that require surgery to insert electrodes deep
into the brain. We claim that Non-Invasive Brain Stimulation (NIBS)
will provide new treatment methods with much greater simplicity,
lower cost, improved safety and in some cases, possibly greater
effectiveness.
Mental health can affect daily life, relationships, and even
physical health. Mental health also includes a person’s ability to
enjoy life - to attain a balance between life activities and efforts
to achieve psychological resilience [4].One of the side effects of
modern technology and our dependency on electronic gadget is
isolation and living in a silo mode among the youths and being
member of a social media is like adding salt to injury as far as we
are concerned (Figure 1). Furthermore, Neurological disorders
with symptoms such as chronic pain, depression, and insomnia
are widespread among “Global Population” in particular among
youngsters in more developed countries and the fast paste life that
these youths are living in. Very weak electric fields applied through
the skull can enhance or diminish neural activity and modulate
brain waves in order to treat many of these common medical
problems. This approach is to be contrasted with well-established
pharmacological methods or more recent invasive electrical Deep
Brain Stimulation (DBS) techniques that require surgery to insert
electrodes deep into the brain. We claim that Non-Invasive Brain
Stimulation (NIBS) will provide new treatment methods with much
greater simplicity, lower cost, improved safety and in some cases,
possibly greater effectiveness. This emerging use of NIBS is a branch
of a new multidisciplinary field that we coined Neuro-systems
Engineering [5]. This field involves neuroscientists, psychologists,
and electrical engineers. This emerging field relies on existing
standards for the safe implementation of these novel treatment
modalities. Methods of stimulating the brain are based on emerging
electro-technologies such as transcranial [6]. As summary of this
introduction, we can express that, Depression is a serious medical
illness. It’s more than just a feeling of being sad or “blue” for a few
days. If you are one of the more than 19 million teens and adults in
the United States who have depression, the feelings do not go away.
They persist and interfere with your everyday life [7].
Symptoms can include:
• Feeling sad or “empty”
• Loss of interest in favorite activities
• Overeating, or not wanting to eat at all
• Not being able to sleep, or sleeping too much
• Feeling very tired
• Feeling hopeless, irritable, anxious, or guilty
• Aches or pains, headaches, cramps, or digestive problems
• Thoughts of death or suicide
Depression is a disorder of the brain. There are a variety
of causes, including genetic, biological, environmental, and
psychological factors. Depression can happen at any age, but it
often begins in teens and young adults. It is much more common in
women. Women can also get postpartum depression after the birth
of a baby. Some people get seasonal affective disorder in the winter.
Depression is one part of bipolar disorder.
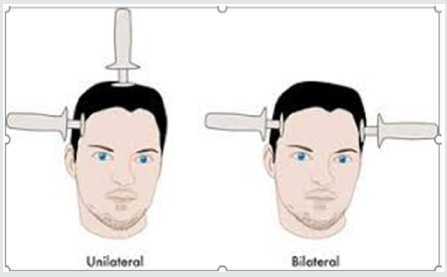
There are effective treatments for depression, including antidepressants, talk therapy, or both. Although the common treatment of severe depression is the hospitalization these types of patients following series electrical shock therapy such as Electroconvulsive Therapy (ECT) highly recommended by phycologist and physiatrist these days, which is very invasive approach, yet there are other suggested treatment that may have similar result yet not being as invasive as ECT. As (Figure 2) illustrates two electrode probe is used to send electrical shock to patient brain and side effect of beside putting patient under anesthesia, in a long would cause permanent lapse of patient memory which is very common among patients going through this procedure. However, these authors do suggest another way of treating depression using a non-invasive approach such as Transcranial Magnetic Stimulation (TMS) or Transcranial Electric Stimulation (TES) or any other aspect of these types of treatments such as r TMS or r TES that are standing for repetitive TMS or TES respectfully [2,3]. There are mind research centers that are seriously looking for this noninvasive treatment these days and their data shows a good evidence of a positive and conclusive results.
Who is at Risk for Suicide and Why?
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
According to the MedlinePlus web site [8], suicide does not
discriminate. It can touch anyone, anywhere, at any time. But
there are certain factors that can contribute to the risk of suicide,
including:
• Having attempted suicide before
• Depression and other mental health disorders
• Alcohol or drug use disorder
• Family history of a mental health disorder
• Family history of an alcohol or drug use disorder
• Family history of suicide
• Family violence, including physical or sexual abuse
• Having guns in the home
• Being in or having recently gotten out of prison or jail
• Being exposed to others’ suicidal behavior, such as a
family member, peer, or celebrity
• Medical illness, including chronic pain
• Stressful life event, such as a job loss, financial problems,
loss of a loved one, a breakup of a relationship, etc.
• Being between the ages of 15 and 24 years or over age 60
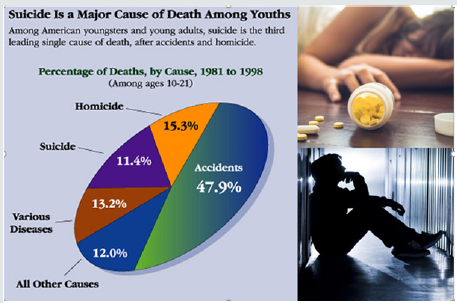
Suicide is a major cause of death among youths as we stated at
the beginning of this article is on exponential rise and it is becoming
a serious threat to our future national brain investment of our
youths and has such devesting on the family that are losing their
youngsters to such episode. (Figure 3) is indication of American
youngsters and young adults, that are victim of suicide that is
seriously drive by depression scenario and it is leading single cause
of death, after accidents and homicide. “The chances of a person at
the young age range dying by suicide are greater than homicide,
when it used to be the reverse,” said Sally Curtin, a statistician at
the CDC and an author of the report. “When a leading cause of death
among our youth is increasing, it behooves all of us to pay attention
and figure out what’s going on”.
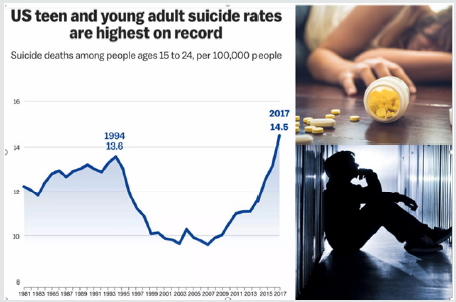
Suicide rates in general have increased [8] in the U.S. across all ages and ethnic groups, rising roughly 30% from 1999 to 2016. In 2017, suicide was the second-leading cause of death among those ages 10 to 24, behind unintentional injuries, such as car crashes or drug overdoses (Figure 4). Suicide death rates have risen significantly in most states since the late 1990s, with 25 states recording increases of more than 30%, the Centers for Disease Control and Prevention said. The rates rose in men and women and across all age and ethnic groups, propelled by mental illness, substance-use disorders, financial hardship and relationship problems, the CDC said. Death by firearm was the most common method of suicide, accounting for 48.5% of cases.
The data that is pulled from death-certificate data from CDC National Vital Statistics System, looking at the underlying cause of death for people ages 10 to 24. They analyzed data from 2000 to 2017, the most recent year of CDC’s available data. Both suicide and homicide deaths among the age group were relatively stable from 2000 to 2007, the report says [1]. Within the next few decade, suicide deaths increased from 6.8 deaths per 100,000 people to 10.6 deaths, with 2,449 more suicides in 2017 than in 2007 time period. While the youth in the ages between 10- to 14-year-olds had by far the lowest rate of suicides, that rate nearly tripled from 2007 to 2017 [1].
Unfortunately, it’s not surprising, but it is highly disturbing,”
said Benjamin Shain, a child and adolescent psychiatrist at
NorthShore Medical Group in Illinois, who says he is increasingly
seeing adolescent patients at risk for suicide. “To see it statistically
across the country hits me in a different way.” Homicide deaths
ranked third, according to a CDC report from June 2019. Despite
concern over the rising suicide rates, researchers aren’t sure of
the exact causes. A rise in depression among adolescents, drug
use, stress and access to firearms might all be contributing factors,
experts say.
Some mental-health experts suggest that social-media use
among teens might be fueling the increase in mental-health
conditions and leading to greater suicide risk, and some early
studies have linked smartphone use to anxiety, depression and sleep
deprivation among adolescents. The recent visibility of suicide in the
media and online might also increase suicide death rates, experts
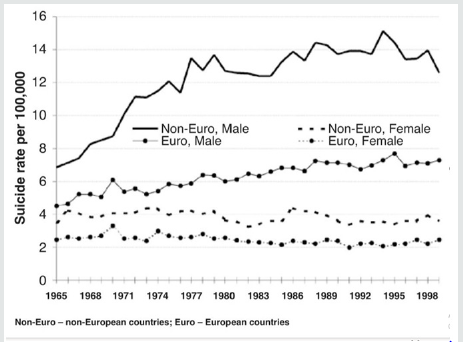
say. (Figure 5) obtained from the article reported by Wasserman
et. al. and quoted from the latest World Health Organization (WHO)
is good indication of suicide rate in 26 countries (areas), data that
were available for the whole period studied between period of
1965 – 1999 and they are broken by gender and expended during
three periods (1965-1979, 1980-1989 and 1990-1999).
Suicidal behavior is a major health concern in many countries, developed and developing alike. At least a million people are estimated to die annually from suicide worldwide [9] Many more people, especially the young and middle-aged, attempt suicide [10]. Some worldwide analyses of suicide trends and rates in the world have been published [11-14] but very little is known worldwide about the causes of death and suicide rates among young people aged 15-19. International comparability of data is also discussed in these refences. The information used is reflecting the official figures reported to WHO by member states, is based on death certificates signed by legally authorized personnel - usually doctors or police officers in the respective country. Usually these professionals have specific routines. How these routines differ between countries and regions, and how they influence suicide statistics, remains to be demonstrated through comparative studies of mortality statistics [1].
What are the Warning Signs for Suicide?
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
Some people may tell others about their suicidal thoughts.
But others may try to hide them. This can make some of the signs
harder to spot [8].
The warning signs for suicide include:
• Talking about wanting to die or wanting to kill oneself
• Making a plan or looking for a way to kill oneself, such as
searching online
• Buying a gun or stockpiling pills
• Feeling empty, hopeless, trapped, or like there’s no reason
to live
• Being in unbearable pain
• Talking about being a burden to others
• Using more alcohol or drugs
• Acting anxious or agitated, behaving recklessly
• Sleeping too little or too much
• Withdrawing from family or friends or feeling isolated
• Showing rage or talking about seeking revenge
• Displaying extreme mood swings
• Saying good-bye to loved ones, putting affairs in order
One of the initial approaches by anyone who is feeling
depressed, is that she or he should stay connected rather than
staying in a total isolation and continue with silo day-to-day life. As
a friend, member of family, co-worker etc. we should ask the person
if they are thinking about killing themselves or keep them safe by
finding out whether they have a plan for suicide and keep them
away from things that they can use to kill themselves that even may
include keep them away from their electronic gadget such as Smart
Phone as well as social media and Internet as part of driven factor
by modern technology.
To be there with them, when they need us and listen carefully
and find out what are they thinking and feeling and finally helped
them connected to resources that can help them, such as:
• Calling the National Suicide Prevention Lifeline at 1-800-
273-TALK (1-800-273-8255). Veterans can call and press 1 to
reach the Veterans Crisis Line.
• Texting the Crisis Text Line (text HOME to 741741)
• Texting the Veterans Crisis Line at 838255
These are very important steps that people around youngsters
can do to help them by keeping them away from their suicide
thoughts and commitment to it.
The Impact of Technology on Mental Health
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
As we have stated at the beginning, mental health can affect
daily life, relationships, and even physical health. Mental health also
includes a person’s ability to enjoy life - to attain a balance between
life activities and efforts to achieve psychological resilience [4].
“Emotional, behavioral, and social maturity or normality; the
absence of a mental or behavioral disorder; a state of psychological
well-being in which one has achieved a satisfactory integration of
one’s instinctual drives acceptable to both oneself and one’s social
milieu; an appropriate balance of love, work, and leisure pursuits”.
As it can be observed in (Figure 6), the mental health problems
have no age limit and can affect anyone at any age and statics shows
a growing epidemy among youths in globally driven by fast paste
modern technology and world of electronic and gadgets.
According to the World Health Organization (WHO), mental
health is “…a state of well-being in which the individual realizes his
or her own abilities, can cope with the normal stresses of life, can
work productively and fruitfully, and is able to make a contribution
to his or her community”. Experts say we all have the potential
to develop mental health problems, no matter how old we are,
whether we are male or female, rich or poor, or which ethnic group
we belong to.
Almost 1 in 5 Americans experiences mental health problems
each year (18.5 percent). In the United States, in 2015, an estimated
9.8 million adults (over 18) had a serious mental disorder. That
equates to 4.8 percent of all-American adults. A large proportion of
the people who have a mental disorder have more than one. In the
U.S. and much of the developed world, mental disorders are one of
the leading causes of disability. Mental illnesses are common in the
United States. Nearly one in five U.S adult’s lives with a mental illness
(44.7 million in 2016). Mental illnesses include many different
conditions that vary in degree of severity, ranging from mild to
moderate to severe. Two broad categories can be used to describe
these conditions: Any Mental Illness (AMI) and Serious Mental
Illness (SMI). AMI encompasses all recognized mental illnesses. SMI
is a smaller and more severe subset of AMI. Additional information
on mental illnesses can be found on the National Institute of Mental
Health (NIMH) Health Topics Pages [15].
Note that The National Institute of Mental Health (NIMH), the
lead federal agency for research on mental disorders, offers basic
information on mental disorders, a range of related topics, and
the latest mental health research. It is not the intention of NIMH
to provide specific medical advice, but rather to provide users
with information to better understand their health and their
diagnosed disorders. Consult with a qualified health care provider
for diagnosis, treatment, and answers to your personal questions.
Dealing with the subject of this section, one important question
that we need to ask is How modern life affects our physical and
mental health given fast paste growth of modern technology and
increasing volume of information that brain needs to process?
[16] Modern day living is a multifaceted compendium of evolving
technology and social media. Communication outlets are changing
every part of our lives so rapidly that it can be tough to adjust. Are
technology and media affecting our physical and mental health? See (Figure 7). Technology has improved the lives of many people,
with almost half of adults in the United States unable to imagine life
without their smartphone.
As (Figure 8) is illustrating, the technological and social media
advances of the past decade have taken over our lives. As this
illustration presents, today’s vast volume of data and consequently
information has tremendous impact on day-to-day life of folks
to the point that we can observe everyone is on their Personal
Device Assistant (PDA) at any moment of their life. Do they affect
our physical and mental health? The American Psychological
Association’s Stress in America Survey 2017 shows that 99 percent
of adults own an electronic device, around 86 percent own a
computer, 74 percent own a smartphone, and 55 percent own a
tablet.
The survey also reports that between 2005 and 2015, the
percentage of adults using social media skyrocketed from 7 percent
to 65 percent, with usage rates of young adults aged between 18
and 29 increasing from 12 percent to 90 percent in that period.
Rates of technology and social media use are therefore swiftly
climbing. Facebook and Instagram alone boast a combined monthly
user base of 2 billion people. Recent research by The Associated
Press-NORC Center for Public Affairs Research found that teenagers
aged 13 to 17 years old have shifted their preferred social media
platforms and are now most likely to use Snapchat and Instagram.
Key findings of the survey included the fact that around 76
percent of teenagers use Instagram, 75 percent use Snapchat, 66
percent use Facebook, 47 percent use Twitter, and fewer than
30 percent use Tumblr, Twitch, or LinkedIn. They also found
that although 91 percent of teens use regular text messaging, 40
percent also use messaging apps such as WhatsApp, Kik, or Line. Social media and text messaging have become an integral part of
how individuals interact with their social groups. In fact, for many
teenagers and young adults, text messaging and social media
communication is now more likely than in-person interactions.
The more details about this issue can be chapter 4 of the book
by Zohuri [2] and we strongly recommend the readers of this article
to refer to this reference as well. Furthermore, while many people
strongly agree that unplugging or taking a digital detox now and
then is important for mental health, in reality, only 28 percent of
those people periodically switch off from technology. Across the
generations, 48 percent of Millennials, 37 percent of Gen Xers, 22
percent of Boomers, and 15 percent of Matures are worried about
the negative effects of social media on their physical and mental
health.
As (Figure 9) indicates using social media for extended periods
is associated with depression. Interactions on social media can
have a major impact on an individual’s well-being and satisfaction.
Many studies have observed that more time spent on social media
is associated with an increased risk of loneliness and depression,
which poses the question: are unhappy people using social media,
or does social media use affect happiness?
Transcranial Magnetic Stimulation Driving Depression Treatment
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
As we start introducing Transcranial Magnetic Stimulation
(TMS) as most effective and non-invasive way of treating at least
mild-depression along with other branches of this technology
such as RTMS, TES and RTES, we need to present a holistic
description of TMS approach for those readers that do not have
any background such technological background what is the TMS.
Transcranial magnetic stimulation (TMS) is a noninvasive method
to excite neurons in the brain: weak electric currents are induced
in the tissue by rapidly changing magnetic fields (electromagnetic
induction) [16] This way, brain activity can be triggered with
minimal discomfort, and the functionality of the circuitry and
connectivity of the brain can be studied.
The principle of inductive brain stimulation with eddy currents
has been noted since the 19th century. The first successful TMS
study was performed in 1985 by Anthony Barker [17] in Sheffield,
England. By stimulating different points of the cerebral cortex and
recording responses, e.g., from muscles, one may obtain maps
of functional brain areas. By measuring functional imaging (e.g.
Magnetic Resonance Imaging (MRI)) or Electroencephalogram
(EEG), where this test records the electrical signal of the brain and
the information may be obtained about the cortex (its reaction to
TMS) and about area-to-area connections.
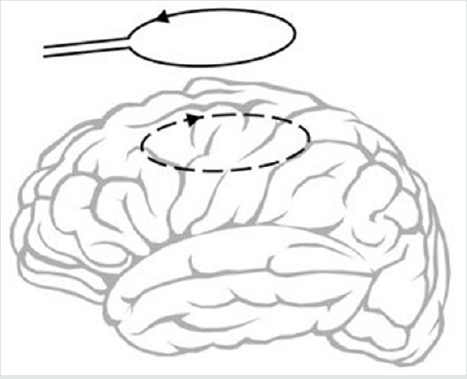
The basic principle of Transcranial Magnetic Stimulation is
shown schematically in (Figure 10), where TMS is showing a timevarying
pulse of current in an external coil causing inducing currents
in the brain. Magnetic stimulation can be used as an alternative to
conventional electrical stimulation of nerves in some applications
because it has a number of advantages which are discussed later.
Applications include deep peripheral nerve stimulation and the
non-invasive and painless stimulation of the human brain, both to
elicit responses directly and to modify excitability and plasticity.
Magnetic stimulation can be used as an alternative to conventional
electrical stimulation of nerves in some applications because it has
a number of advantages which are discussed later. Applications
include deep peripheral nerve stimulation and the non-invasive and
painless stimulation of the human brain, both to elicit responses
directly and to modify excitability and plasticity. Repetitive TMS
stimulation is known as RTMS and can produce longer lasting changes. Numerous small-scale pilot studies have shown it could be
a treatment tool for various neurological conditions (e.g. migraine,
stroke, Parkinson’s disease, dystonia, tinnitus) and psychiatric
conditions (e.g. major depression, auditory hallucinations). TMS
is becoming more widely used for treating nonresponsive severe
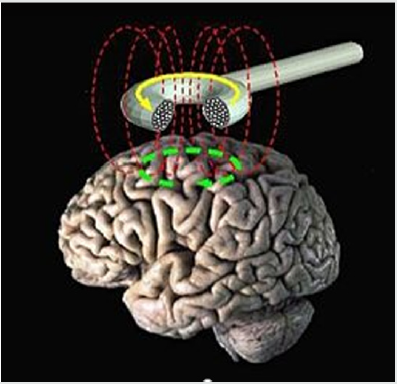
depression. (Figure 11) shows how the TMS coil produces that
fields, where noninvasively interact with the brain. In this figure,
the time-changing magnetic field (Red Color) induces the electric
field and currents (Green color) in the brain. (Courtesy E.M.
Wassermann) and current in the coil (Yellow color).
In the last 20 years, the use of Non-Invasive Electrical Brain
Stimulation (NIBS) has transitioned from the ad hoc use of a variety
of techniques and methods to a more system engineering approach
to achieving desired methods to treat neurological disorders
tailored to specific problems and individual characteristics [18]. We
have described this approach to the combination of neuroscience,
psychology, and electrical engineering as the new field of Neuro
systems Engineering [19] We believe this new multidisciplinary
engineering approach will have a profound and lasting impact
on serious health problems. Our specific and original concept is
a systematic combination of methods described in the following
sub-sections, TACS, TRNS, and real time control to achieve major
cognitive benefits. This is to be compared with prescriptive
application of NIBS, or the use of pharmacological prescriptions
that treat disease, but create undesirable outcomes: neither are
individualized to the disorder or the individual except through a
process of trial and error. We are proposing an approach based on
treating specific problems from a Neuro system Engineering point
of view.
A Neuro systems Engineer approaches the solution to problems
through first focusing on the specific problem, and then applying the scientific method of hypothesis, experimentation, data
collection, and modification of the process and the hypothesis until
a consistent explanation is achieved in order to solve the problem.
We believe this approach resulted in our thinking about tailored
control to focus the dose, duration, frequency spectrum, and
electrode geometry to deal with the individual and the disorder.
Individualized treatment approaches, using neuroimaging, are
beginning to be used in the field of ECT [20] and we believe that
this approach can be applied more broadly and with a high degree
of fidelity.
Transcranial Alternating Current Stimulation (TACS)
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
Relatively few studies of transcranial Alternating Current Stimulation (TACS) have been undertaken, a technique designed to change intrinsic cortical oscillations. The current can be applied to the earlobes or the sides of the head, known as Cranial Electrotherapy Stimulation – (CES) [21]. This technique opens up the possibility of actively synchronizing cortical rhythms through external means particularly when administered in the so-called “ripple” frequency range (between 100 and 250 Hz) associated with memory encoding [22]. This technique must be used at relatively low frequencies or retinal flashes will be induced; moreover, at higher amplitudes, safety concerns - including seizures - remain. In spite of these very particular reservations, active synchronization of cortical oscillatory activity provides particularly enticing possibilities regarding very fine-tuned experiments involving stimulation, behavior modification, recording of neuronal activity, and alteration of stimulation in real time. Currently, the TACS method is primarily used to treat depression, anxiety, and other mood related disorders.
Transcranial Random Noise Stimulation (TRNS)
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
The most recent player to the electrical stimulation field is transcranial Random Noise Stimulation (TRNS). This method, akin to adding “white noise” to ongoing neural activity, is thought to open ion channels at the neuron [23] In one of the first studies in normal human subjects, stimulation over the motor cortex (between 100 and 640 Hz for 10 minutes at 1.5 mAmp) was found to increase cortical excitability [24] These authors hypothesize that, like TACS, TRNS “can possibly interfere with ongoing oscillations and neuronal activity in the brain and thus result in a cortical excitability increase.”
There are several potential advantages of TRNS over TDCS:
a. While Transcranial direct current stimulation (TDCS) can
open ion channels once, TRNS can do so repeatedly through
multiple ionic influxes.
b. TRNS works around problems associated with stimulation
of different sides of a folded cortex which can lead to effects
which cancel each other out;
c. TRNS does not create a “tingling” sensation, as does TDCS
when applied;
d. safety concerns are minimized.
A recent study found superior performance of high frequency
(100 - 640 Hz) tRNS over tDCS (1.5 mAmp) in normal subjects
on a perceptual learning task [25] A second study did not find
improved performance of TRNS over TDCS in normal subjects on
a working memory paradigm [26] Only a handful of studies have
been undertaken with TRNS; however, this technique appears to
combine the main benefits of both TDCS (e.g., ionic influx/neuronal
excitation) and TACS (e.g., entrainment of oscillations) without
many of the potential downsides (e.g., burning, retinal stimulation,
possible seizures, etc.).
In conclusion for the above methodology of treatment
depression and brain disorder, we believe that this Neurosystems
Engineering approach will provide improved understanding
of many neurological disorders and the ability to achieve real
improvements in a nonpharmacological, painless, low cost, and
practical approach that will have an enduring impact on society.
Future advances in this electrotechnology must be achieved in
coordination with the standards community.
Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
With the increase in the suicide rate, particularly among
the youths, researchers and clinicians have explored the utility
of Artificial Intelligence (AI) in suicidal risk prediction and
management [27] have conducted a general review of the
scholarly works on the utility of AI in suicidal risk prediction and
management. According to these authors, several studies have
been directed toward the role of AI in identifying suicidal risk and
clinical factors such as state of depression, past clinical diagnosis,
substance abuse, and treatment history [28,29] while other studies
have explored the environmental factors [30,31].
The starting point for most of such studies is Machine Learning
(ML), depending on the availability of data, to do modeling and
potentially prediction. A key challenge in this nascent field is access
to adequate and appropriate data. According to [27] though suicidal
risk factors have been generally identified, data has not yet been
fully integrated into a reliable predictive model. The clinical process
of identifying risk factors and other related diagnosis are still very
subjective and varies among therapists and clinicians. As a result,
common statistical analytical approaches, which are generally
limited in analyzing complex data, have not so far been successful
in predicting suicidal behaviors [32].
As the volume and variety of clinical data are increasing
significantly, there is hope that AI can help with potential
prediction of risk factors to supplement clinical diagnosis. Some
studies and exploratory analyses have shown early promises in identifying predominant suicide risk domains. These works have
identified clinical risk, such as sudden mood change, recent history
of low mood, self-injury, psychiatric comorbidity and previous
hospitalizations [33,29] and cognitive risk, such as sentiments
around life satisfaction, purpose, hopelessness, self-esteem and selfperceived
competency [34,35] Sentiment analysis is one area with
potential promise for suicidal risk prediction and management.
Another AI-related area that has received quite a bit of attention
recently is the so called ‘conversational agents’. Conversational
agents utilize Natural Language Processing (NLP) by simulating
conversations with individuals and generating human-like
responses using a text- or voice-based connectivity [36] This new
approach has been increasingly adopted by therapists and clinicians
to deliver psychological interventions such as social therapy [37]
cognitive behavioral therapy [38] and trauma therapy [39]. With
the increase use of devices such as smartphones, intervention
delivery can be provided to a patient’s emotional state [37]. Though
AI-based approaches to suicide risk prediction and management
are still in their early stage, the advancement in technology and
clinical processes, such as better clinical data integration and
sentiment analysis, can perhaps enhance the current prediction
and prevention attempts, to identify risk factors in real time and
potentially allow for mitigation of the increasing likelihood of
suicides among the youths.
Concluding Remarks
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
Globally, suicide is an epidemic and a dangerous silent disease
among individuals 14 to 28 years old and is rising at an alarming
annual rate in the United States. Youngsters are often resorting
to suicide due to severe depression and the current efforts to
predict the risk factors and mitigate them are falling short. Modern
electronic-based interactions, such as virtual socialization(esocialization),
texting, and social media, have often replaced
simple human interactions and dialogue such as ‘Hello, How Are
You’ among most members of this demographic. The proliferation
of electronic devices such as iPod, iPad, smart phones and any
personal computers or electronic game platforms appears to
have contributed to the seclusion of this vulnerable group, further
diminishing personal interactions that can possibly mitigate the
increasing rate. Young individuals nowadays do not often socialize
and interact with family members and the community at large
as much as our previous generations did. Lack of daily routine
personal interactions appears to add to the severity of depression
in particular among the youth.
Moreover, pharmacological treatments of depression via
medications or an invasive treatment such as Electroconvulsive
Therapy (ECT) do not appear to be highly effective for Major
Depressive Disorder (MDD). The first author of this article
recommends other methodology such as Transcranial Magnetic
Stimulation (TMS) or repetitive TMS (RTMS) as alternative and
non-invasive approaches [2,3]. Recent studies, however, underline that both the size and complexity of data collected from health
institutions, including patient records, images, and test results.
The growing volume and variety of data can provide a basis for
better analyses leading to better diagnosis and prognosis. AIbased
approaches, integrating medicine and data science, have the
potential to supplement the current efforts at suicide risk factors
identification and management, as well as intervention delivery
[40-42].
References
- Abstract
- Introduction
- Who is at Risk for Suicide and Why?
- What are the Warning Signs for Suicide?
- The Impact of Technology on Mental Health
- Transcranial Magnetic Stimulation Driving Depression Treatment
- Transcranial Alternating Current Stimulation (TACS)
- Transcranial Random Noise Stimulation (TRNS)
- Feasibility of Artificial Intelligence in Suicide Risk Prediction and Management
- Concluding Remarks
- References
- Jean Whalen (2018) Youth Suicidal Behavior Is on the Rise, Especially Among Girls. The Wall Street Journal, USA.
- Bahman Zohuri, Patrick J McDaniel (2019) Electrical Brain Stimulation for the Treatment of Neurological Disorders. Apple Academic Press and CRC Press (CRC) Taylor & Francis Grouppp.550.
- Bahman Zohuri, David R Modisette (2019) Electrical Brain Stimulation to Treat Neurological Disorder Journal of Health Science 7:123-128.
- Christian Nordqvist, https://www.medicalnewstoday.com/articles/154543.php, UK.
- Yonas G, Jung R(2008) Fixing brains. Innovation: America’s Journal of Technology Commercialization6(3).
- Wassermann EM (1998) Risk and Safety of Repetitive Transcranial Magnetic Stimulation: Report and Recommendations from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, June 5-7, 1996. Electroenceph. Clin. Neurophysiol. 108(1):1-16.
- https://medlineplus.gov/depression.html, USA.
- https://www.wsj.com/articles/cdc-finds-rise-in-suicide-rates-across-the-u-s-1528417378?mod=article_inline
- Bertolote JM (2001) Suicide in the world: an epidemiological overview, 1959-2000. In: Wasserman D editor. Suicide - an unnecessary death. London: Dunitz, UK pp: 3-10.
- Wasserman D (2001) Suicide- an unnecessary death. London pp: 160.
- La Vecchia C, Lucchini F, Levi F (1994) Worldwide trends in suicide mortality, 1955-1989. Acta PsychiatrScand 90(1):53-64.
- Diekstra RFW (1996) The epidemiology of suicide and parasuicide. Arch Suicide Res 2(1):1-29.
- Schmidtke A, Weinracker B, Apter A, Batt A, Berman A, et al. (1999) Suicide rates in the world: update. Arch Suicide Res 5(1):81-89.
- Yang B, Lester D (2004) Natural suicide rates in nations of the world. Crisis 25(4):187-188.
- https://www.nimh.nih.gov/health/topics/index.shtml
- Lefaucheur JP (2009) Methods of therapeutic cortical stimulation. Neurophysiologie Clinique/Clinical Neurophysiology 39(1):1-14.
- http://www.scholarpedia.org/article/Transcranial_magnetic_stimulation
- Priori A (2003) Brain polarization in humans: a reappraisal of an old tool for prolonged non-invasive modulation of brain excitability. Clinical Neurophysiology 114(4):589-595.
- Yonas G, R Jung (2008) Fixing brains Innovation:America's journal of Technology Commercialization 6(3).
- Ujkaj M, DavidoffDA (2012) A novel approach to individualized treatment in psychiatry: use of neuroimaging to predict efficacy and tolerability of ECT treatment for depression in routine clinical practice. Journal of ECT 28(2): 149-149.
- Zaghi S, Acar M, Hultgren B, Boggio PS, Fregni F (2010) Noninvasive brain stimulation with low-intensity electrical currents: putative mechanisms of action for direct and alternating current stimulation. The Neuroscientist 16(3):285-307.
- Vera Moliadze, Andrea Antal, Walter Paulus (2010) Boosting brain excitability by transcranial high frequency stimulation in the ripple range. journal of Physiology 588(24):4891-4904.
- Schoen I, Fromherz P (2008) Extracellular stimulation of mammalian neurons through repetitive activation of Na+ channels by weak capacitive currents on a silicon chip. I. Neurophvsiol 100(1):346-357.
- Terney D, Chaieb L, Moliadze V, Antal A, Paulus W, et al. (2008)Increasing human brain excitability by transcranial high-frequency random noise stimulation. Journal of Neuroscience 28(52): 14147-14155.
- Fertonani A, Pirulli C, Miniussi C, (2011) Random noise stimulation improves neuroplasticity in perceptual learning. journal of Neuroscience 31(43):15416-15423.
- Mulquiney, PG, Hoy KE, Daskalakis ZJ, Fitzgerald PB (2011) Improving working memory: Exploring the effect of transcranial random noise stimulation and transcranial direct current stimulation on the dorsolateral prefrontal cortex. Clinical Neurophysiology 122(12):2384-2389.
- Trehani M Fonseka, Venkat Bhat, Sidney H Kennedy (2019) The utility of artificial intelligence in suicide risk prediction and the management of suicidal behaviors. Australian & New Zealand Journal of Psychiatry 53(10):954-964.
- Jenkins AL, Singer J, Conner BT, Shawna Calhoun MPH, Guy Diamond (2014) Risk for suicidal ideation and attempt among a primary care sample of adolescents engaging in nonsuicidal self-injury. Suicide and Life-Threatening Behavior 44(6):616-628.
- Passos IC, Mwangi B, Cao B, Hamilton JE, Wu MJ, et al. (2016) Identifying a clinical signature of suicidality among patients with mood disorders: A pilot study using a machine learning approach. Journal of Affective Disorders 193:109-116.
- Bonner RL, Rich AR (1990) Psychosocial vulnerability, life stress, and suicide ideation in a jail population: A cross-validation study. Suicide and LifeThreatening Behavior 20(3):213-224.
- Fernandez-Arteaga V, Tovilla-Zarate CA, Fresan A, González-Castro TB, Juárez-Rojop IE, et al. (2016) Association between completed suicide and environmental temperature in a Mexican population, using the knowledge discovery in database approach. Comput Methods Programs Biomed 135:219-224.
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, et al. (2017) Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin 143(2):187-232.
- Liu Y, Sareen J, Bolton JM, Wang JL (2016) Development and validation of a risk prediction algorithm for the recurrence of suicidal ideation among general population with low mood. Journal of Affective Disorders 193:11-17.
- Barros J, Morales S, Echavarri O, García A, Ortega J, et al. (2017) Suicide detection in Chile: Proposing a predictive model for suicide risk in a clinical sample of patients with mood disorders. RevistaBrasileira de Psiquiatria 39(1):1-11.
- Jordan P, Shedden-Mora MC, Lowe B (2018) Predicting suicidal ideation in primary care: An approach to identify easily assessable key variables. General Hospital Psychiatry 51: 106-111.
- Dahiya M (2017) A tool of conversation: Chatbot. International Journal of Computer Sciences and Engineering 5(5):158-161.
- D’Alfonso S, Santesteban-Echarri O, Rice S, Wadley G, Lederman R, et al. (2017) Artificial intelligence-assisted online social therapy for youth mental health. Frontiers in Psychology 8:PP796.
- Fitzpatrick KK, Darcy A, Vierhile M (2017) Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (Woebot): A randomized controlled trial. JMIR Mental Health 4(2):e19.
- Tielman ML, Neerincx MA, Bidarra R, Kybartas B, Brinkman WP (2017) A therapy system for post-traumatic stress disorder using a virtual agent and virtual storytelling to reconstruct traumatic memories. Journal of Medical Systems 41(8): PP125.
- TurkerTekingErguzel, NevzatTarhan (2016) Machine Learning Approaches to Predict Repetitive Transcranial Magnetic Stimulation Treatment Response in Major Disorder. SAI Intelligent System Conference, London, United Kingdom PP: 1-6.
- Danuta Wasserman, QI Cheng, Guo-Xin Jiang (2005) Global suicide rates among young people aged 15-19. World Psychiatry 4(2):114-120.
- Wassermann EM (1998) Risk and safety of repetitive transcranial magnetic stimulation: report and recommendations from the international workshop on the safety of repetitive transcranial magnetic stimulation, June 5-7,1996. Electroenceph clin Neurophysiol 108(1):1-16.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...