Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6628
Case Report(ISSN: 2637-6628) 
Cranio-Cervical Junction Meningioma: A Rare Case Report Volume 4 - Issue 5
Sukriti Das1*, Asit Chandra Sarker1, Dipankar Ghosh1, Kanji Fatema Ishrat Zahan1, Mohammed Shamsul Islam Khan1, Akhlaque Hossain Khan2 and Bipin Chaurasia3
- 1Department of Neurosurgery, Dhaka Medical College & Hospital, Bangladesh
- 2Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Bangladesh
- 3Department of Neurosurgery, Tarai Hospital and research centre, Birgunj, Nepal
Received: November 06, 2020; Published: November 30, 2020
Corresponding author: Sukriti Das, Associate Professor, Department of Neurosurgery, Dhaka Medical College & Hospital, , Dhaka, Bangladesh
DOI: 10.32474/OJNBD.2020.04.000198
Abstract
Background: Meningioma is a benign and slowly growing intradural extramedullary spinal cord tumor. It arises from the arachnoid cap cell of the meninges. Meningioma of the cranio-cervical junction is a rare and unique diagnosis of about 1.8-3.2% of all meningiomas. These tumors usually grow slowly and develop symptoms gradually but, sometimes with sudden onset of quadriplegia. The lesions are usually very large at the time of diagnosis. Post-surgical tumor recurrence is high due to failure of complete removal of the tumor (Simpson grade-I) as critical vascular structures, brainstem and cranial nerves are close to it.
Case Report: We presented a case of a cranio-cervical junction meningioma of a 45-year-old female who presented with neck pain with headache and gradual weakness of all 4 limbs that made her unable to walk without support and bed-ridden gradually. She also developed urinary incontinence and was catheterized. On examination, the patient was conscious and alert, muscle power was of MRC grade 0/5 in all groups of muscles in all 4 limbs. All deep tendon reflexes were exaggerated in both upper and lower limbs with positive Hoffmann sign bilaterally and bilateral planter extensor response. All modalities of sensations were diminished up to C4 vertebral level. MRI of cervical spine was obtained, and the diagnosis of cranio-cervical junction meningioma came out.
Conclusion: After complete surgical removal (Simpson grade I) of the tumor, post-operative ICU management is very vital. Extubation and recovery may need long time to return to normal life. So pre-operative counseling and post-operative ICU support is mandatory to operate cranio-cervical junction meningioma.
Keywords: Cranio-Cervical Junction; Meningioma; Intradural-Extramedullary; Simpson Grade; Gross Total Removal
Introduction
Meningiomas were named by Harvey Cushing in 1922 and described as common tumors that arise from arachnoid cap cells which form the outer lining of the arachnoid membrane and from related cells such as arachnoid fibroblasts and the meningoblast [1-3]. These tumors are generally benign tumors and carry good prognosis. Meningiomas are adult onset tumors with age incidence ranging from 20-60 years and peak at around 40 years. There is also a sex preponderance with female, especially with spinal cord meningioma [4]. Cranio-cervical junction meningioma accounts for 1.8%-3.2% of all meningiomas [5]. These lesions are often large at the time of diagnosis [6]. Meningioma of the cranio-cervical junction is a rare and unique diagnosis among meningiomas [5- 7]. They originate from the arachnoid cap cells of the lower part of the clivus and upper aspect of C2 lamina. They are intradural and extramedullary tumor. Here, meningioma is a well circumscribed oval or round, lobulated tumor attached to the dura. This location often causes compression of the spinal cord with slowly progressive features of myelopathy [4]. Mortality, morbidity and recurrence are 16.7%, 5.5% and 5.5% respectively [8]. Approximately 70% of all tumors in cranio-cervical junction are meningiomas [5]. Complete resection should be the primary goal of surgery but, is often difficult to achieve due to their close relationship with critical vascular structures, the brainstem and cranial nerves. Therefore, Simpson grade-I resection is rarely achieved which might explain the higher risk of recurrence [1,2,7,9].
Case Report
A 45-year-old lady presented with neck pain and weakness of
all four limbs. Weakness was gradual in onset, progressive in nature
and associated with stiffness. Weakness started from right upper
limb, then gradually involved right lower limb followed by left
upper limb and lastly left lower limb. She developed grip weakness
of her right hand at the beginning, then she noticed herself limping
also developed inability to perform household works, difficulty
in walking without support and ultimately became bedridden.
She also developed urinary incontinence and constipation in the
meantime. She complained neck pain for about last 3 years which
was episodic, located in back and side of the neck and lower part
of back of the head being constant dull aching in nature, mild to
moderate in intensity, non-radiating, with no diurnal variation, no
known aggravating factors and usually relieved by pain killer [10].
On examination- the patient was conscious and alert, but
ill looking and bed ridden. Motor examination of all four limbs
revealed- bilateral symmetrically reduced muscle bulk, increased
muscle tone. Muscle power was of MRC grade-0/5 in all groups of
muscle in all four limbs, all deep tendon reflexes of upper and lower
limbs were exaggerated with bilateral planter extensor and bilateral
positive Hofmann sign. Clinical diagnosis was made as a case of
spastic quadriplegia due to compressive cervical myelopathy (High
cervical).
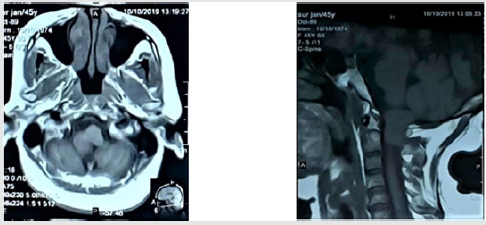
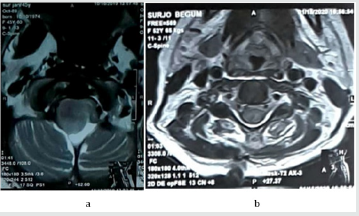
MRI of cervical spine with and without contrast revealed a welldefined
lobulated mass measuring about 56.3 mm x17.4 mm that
is intermediate in intensity in both T1Wl & T2Wl, is seen at craniocervical
junction & upper cervical canal causing compression at
lower pons, upper cervical cord and also over corresponding C2
nerve roots. After IV contrast—Contrast enhancement of the lesion
is seen. X-ray of cervical spine was normal.
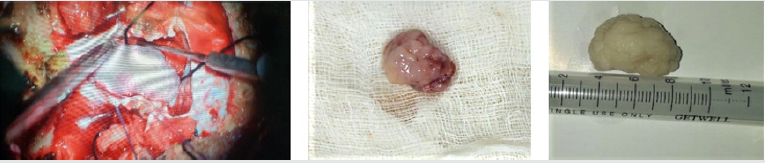
The patient was diagnosed as a case of spastic quadriplegia
due to cranio-cervical junction meningioma. She underwent
midline sub-occipital craniectomy with laminectomy at C1 and
C2 with complete surgical excision of tumor (Simpson grade-I).
Histopathology report also revealed meningioma (WHO grade-I).
Post-operative follow-up was given in ICU and on the 10th POD the
patient was extubated with motor power of MRC grade 3/5 as she
was shifted to general ward. She was discharged on the 15th POD.
Now, after 2 months following operation, she is able to walk with
support having motor power of MRC grade 4+/5 in all four limbs
(Figures 1-8).
Figure 5:‘a’ pre op T1WI sagittal film showing tumor and ‘b’ post op T1WI sagittal film showing complete removal of tumor.
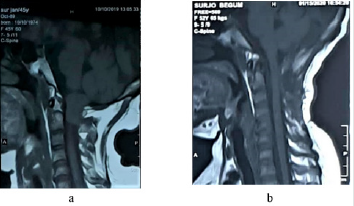
Figure 6:‘a’ pre op T2WI sagittal film showing tumor and ‘b’ post op T2WI sagittal film showing complete removal of tumor.
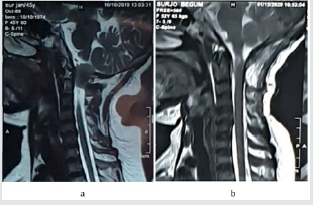
Figure 7:‘a’ pre op T1WI axial film showing tumor and ‘b’ post op T1WI axial film showing complete removal of tumor.
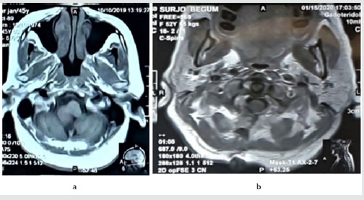
Figure 8:‘a’ pre op T2WI axial film showing tumor and ‘b’ post op T2WI axial film showing complete removal of tumor.
Discussion
We presented our experience in managing cranio-cervical meningioma and its outcome as such tumors are rare (1.8 to 3.2% of all meningiomas) [1]. It is usually benign intradural extramedullary tumor arising from arachnoid cap cells of outer arachnoid layer.
Based on the origin of the tumor matrix or dural attachment, these lesions are of two types-
(i) cranio-spinal and
(ii) spino-cranial.
They are different in their origin, anatomical location and relation with neighboring structures. Spino-cranial tumors are associated with higher rates of total resection with fewer postoperative complications like cranial nerve deficits and vascular damage as mean tumor volume are smaller than cranio-spinal variety. These tumors impinge on the spinal cord earlier than their cranial counterparts, so they cause symptoms at a smaller size resulting in earlier diagnosis. They are about 30% of all craniocervical junction tumor and having higher rate of total resection whereas cranio-spinal meningiomas are relatively asymptomatic with often delayed symptoms and become large at the time of diagnosis along with invasion of surrounding neuro-vascular structures. In these cases, total resection becomes difficult and surgical removal sometimes invite complications. Vertebral artery encasement and cranial nerve deficits are two very vital factors that have to be considered before planning surgery.
Cranio-cervical junction meningiomas are diagnosed by CT scan and MRI of brain with CTA and MR angiogram being sometimes in need. Tumor may be anterior to the neuroaxis- that is anterior or antero-lateral tumors are located ventral to the dentate ligament while posterior and postero-lateral tumors are dorsal to the dentate ligament. The extent of tumor resection was complete or sub-total, but our target was the complete excision of the tumor (Simpson grade-I). As it is a benign tumor, its recurrence rate is scanty. Total resection of cranio-cervical junction meningioma in previous studies was achieved typically in 61-100% of cases. When the tumor engulfs critical neuro-vascular structures sometimes it is treated conservatively. Sometimes radiotherapy is used in conjunction with surgery, but result is not good. In our patient, posteriorly placed cranio-spinal tumor was big and presented with quadriplegia without cranial nerve palsy or vascular encasement. We planned for posterior midline suboccipital craniectomy with laminectomy of C1 and C2. After durotomy, the whole big tumor was revealed, and excision of the tumor was done piece by piece.
Gross total resection was achieved in 45% of patients and sub-total in 55% of cases. But, in our case we performed complete resection (Simpson grade-I) of the tumor. The most common postoperative complications were dysphagia, palsy of cranial nerve- IX, X, XI, XII. But, in our case the patient having no visible cranial nerve palsy, but she had delayed extubation. We obtained an MRI at 15 days after surgery to detect any residual tumor or any collection or pseudo meningocele or CSF leak. The patient was advised to have MRI scan at 2, 6 and 12 months after surgery.
Our patient improved gradually regarding neck pain, hypoesthesia, paresthesia and sphincter disturbance at 2 around months around following surgery and became able to walk with support. NO evidence of any cranial nerve deficit, CSF leak or cerebellar infarction was seen.
Conclusion
Surgical management of cranio-cervical junction meningioma is a challenge to neurosurgeons especially in case of tumors involving neighboring neurovascular structures. Our case had quadriplegia with autonomic disturbances but no vertebral artery encasement or cranial nerve palsy. Though cranio-spinal tumor presents lately and becomes large in size at the time of diagnosis and usually involves surrounding neurovascular elements, it is very difficult to perform complete resection with high rate of post-operative complications. We are happy to say that in our case, we performed complete resection of the tumor without any neurovascular complication. Functional outcome was good (the patient became able to walk with support at 2 months following surgery) with significant improvement of sphincter dysfunction and sensory symptoms.
References
- Cushing H and Eisenhardt L (1939) Meningiomas: Their Classification, Regional Behavior, Life History and Surgical End Results. Arch NeurPsych 41(3): 657-658.
- Alam S, Chaurasia BK, Shalike N, Uddin AN, Chowdhury D, et al. (2018) Surgical management of clinoidal meningiomas: 10 cases analysis. Neuroimmunol Neuroinflammation 5: 21.
- Moududul Haque, Nwoshin Jahan, Shahnawaz Bari, KM Tarekul Islam, Shamsul Alam, et al. (2019) Two cases of atypical foramen magnum meningioma presenting as rotatory paralysis. J Neurol Stroke 9(4): 180-182.
- Wilkins RH and Rengachary SS (1985) Neurosurgery. Vol 1, Section D. McGraw Hill, New York Pp: 614.
- Arnautovic KI, Al-Mefty O, Husain M (2000)Ventral foramen magnum meningiomas. J Neurosurg 92: 71-80.
- Boulton MR, Cusimano MD (2003) Foramen magnum meningiomas: concepts, classifications, and nuances. Neurosurg Focus 14(6): e10.
- Yasuoka S, Okazaki H, Daube JR, MacCarty CS (1978) Foramen magnum tumors. Analysis of 57 cases of benign extramedullary tumors. J Neurosurg 49(6): 828-838.
- Dührsen L, Emami P, Matschke J, Abboud T, Westphal M, et al. (2016) Meningiomas of the Craniocervical Junction – A Distinctive Subgroup of Meningiomas. PLoS ONE 11(4): e0153405.
- Bassiouni H, Ntoukas V, Asgari S, Sandalcioglu EI, Stolke D, e al. (2006) Foramen magnum meningiomas: clinical outcome after microsurgical resection via a posterolateral suboccipital retrocondylar approach. Neurosurgery 59(6): 1177-1185.
- Hwang WL, Marciscano AE, Niemierko A, Kim DW, Stemmer-Rachaminov AO, et al. (2016) Imaging and extent of surgical resection predict risk of meningioma recurrence better than WHO histopathological grade. Neuro oncology 18(6): 863-872.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...