Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6628
Case Report(ISSN: 2637-6628) 
Cerebellar Stroke Causing Ataxia In COVID-19 Patient Presenting with Diarrhea; Time to Re-Think Clinical Picture Of SARS-Cov-2? Volume 5 - Issue 3
Abdul Rafi Mohammed1*, Muneer Abubaker1 and Abdelwahed Abougazia2
- 1Consultant Family Medicine, Primary Health Care Corporation, Qatar
- 2Consultant Radiologist, Primary Health Care Corporation, Qatar
Received: February 18, 2021 Published:February 26, 2021
Corresponding author: Abdul Rafi Mohammed, Consultant Family Medicine, Primary Health Care Corporation, Qatar
DOI: 10.32474/OJNBD.2021.05.000211
Abstract
Coronavirus disease 2019 (COVID-19) predominantly affects respiratory system, typically presenting with fever and cough, but involvement of other systems is not unusual. Neurological manifestations of COVID-19 are rare and may be missed at first presentation. The authors report a case of acute cerebellar stroke in a COVID -19 patient presenting with ataxia and dizziness, three weeks after her first presentation with diarrhea and laboratory confirmation of SARS COV-2 infection. She was found to have an acute cerebellar infarct which resolved over time. The authors are not aware of any previous case reports of COVID-19 related isolated cerebellar stroke with no involvement of other parts of the brain.
Keywords: COVID-19; Pneumonitis; Coagulopathy; Ataxia; Cerebellar Stroke
Introduction
The coronavirus disease 2019 (COVID-19) due to severe acute respiratory Syndrome Coronavirus 2 (SARS-CoV-2) first reported from Wuhan, in the Hubei Province of China in December 2020 started as a cluster of pneumonia cases. Since then, it has been declared a global pandemic and has caused havoc throughout the world with millions being infected. Although the virus predominantly involves respiratory system, it is more evident now that other organ systems are affected too and can be associated with significant morbidity and mortality.
Case Presentatione
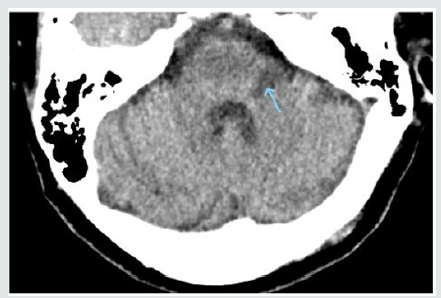
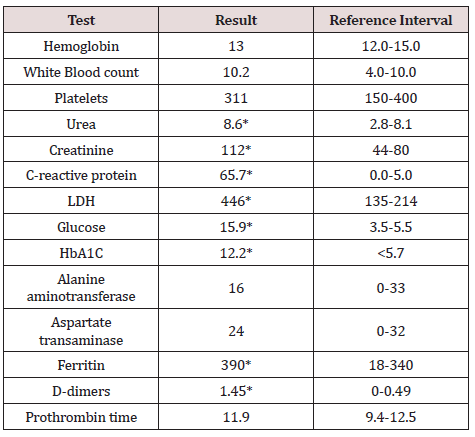
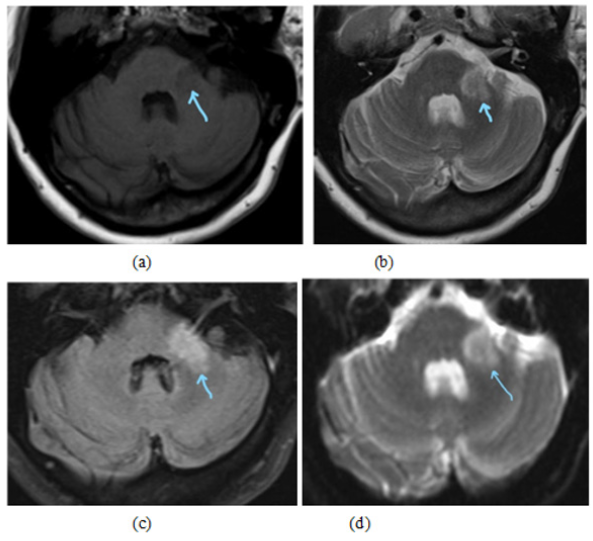
A 63- year-old lady presented to a designated COVID-19 primary health care center with symptoms of diarrhea but no other systemic symptoms. There was no history of any contact with COVID- 19 positive patient. She was diabetic, hypertensive and had chronic kidney disease. In view of the ongoing COVID-19 pandemic, SARS-CoV-2 RT-PCR test was done which was reported positive the following day. She was well clinically, and her vital parameters were stable. Hence as per local protocol she was transferred to a quarantine facility. However, one week later she was admitted to the hospital in view of dyspnea and cough. On arrival to the emergency room, she was afebrile but tachypneic with respiratory rate 30/minute. Oxygen saturation 88%, heart rate 86/minute and BP 162/77 mm of Hg. Chest X-ray showed bilateral diffuse patchy areas of lung consolidation suggestive of COVID Pneumonitis. Results of blood investigations are summarized below. She was treated for Pneumonia as per secondary care COVID-19 protocol along with prophylactic low molecular weight Heparin and was discharged home after 13 days of hospital stay. However, she was re-admitted three days later in view of vertigo and difficulty walking and standing. Detailed examination revealed horizonal nystagmus, delayed tendon reflexes and power of 4/5 in both upper and lower extremities. Finger to nose test and heel to shin test were negative. There was no dysarthria or tremor, and speech was intact. Gait could not be assessed due to severe vertigo. She had an emergency CT brain which showed focal hypodense changes in left middle cerebellar peduncle representing infarcts (Figure 1). MRI done the next day confirmed the same findings as noted on CT (Figure 2), following which she was started on Aspirin and Statin. Echocardiography showed mild concentric Left ventricular hypertrophy with normal global systolic function and no regional wall motion abnormality. She received input from Physiotherapist and was discharged home 5 days later. She made a gradual recovery without any further intervention. She is being reviewed in COVID follow up clinic and remains well so far six months since the diagnosis of cerebellar stroke with no residual neurological deficit (Table 1).
Figure 2: Axial MRI images show an acute infarction at the left cerebellar peduncle. The lesion appears hypointense on T1(a) and hyperintense on T2 (b), FLAIR (c) and DWI (d) (blue arrows).
Discussion
During the early stages of COVID-19 pandemic, it was believed that the virus affects only the lungs but subsequently evidence emerged that it could involve other organ systems too. In our reported patient, diarrhea was the presenting symptom of COVID-19 and studies have shown that gastrointestinal symptoms may be the only clinical feature in some COVID -19 patients [1]. Even though most COVID-19 patients have predominantly respiratory disease, neurological manifestations are being increasingly recognized with common reported symptoms being headache and anosmia [2]. The plethora of neurological features in COVID-19 are varied and depend on the primary pathophysiological mechanisms. These include direct effects of the virus on the nerve cells, infection related immune-mediated disease, and neurological complications arising from the general systemic effects of COVID-19 [3].
COVID-19 associated acute cerebrovascular events are rare but well recognized. In a recent meta-analysis, it had a reported incidence of 1.4% among COVID-19 patients [4]. Even though pre-existing cardiovascular risk factors could play a role in the development of stroke in COVID patients, studies have shown that COVID-19 infection has a significant independent association with acute ischemic stroke [5]. A large multicenter comparison study conducted in UK on COVID-19 related and unrelated strokes concluded that patients with COVID-19 related strokes were more likely to have multiple large vessel occlusions, more severe strokes and were associated with more severe disability on discharge and more inpatient deaths [6]. An interesting point to note is the delayed presentation of stroke in our reported patient, with symptoms developing 23 days after testing positive for COVID-19 This is in keeping with the results of a systematic review of COVID-19 patients with acute ischemic stroke, which reported a mean duration of 10 +/- 8 days, from the onset of COVID-19 related symptoms [7]. This could be explained by the proposed pathophysiological mechanisms of early hyperinflammatory state from cytokine storm followed by a prothrombotic state complicated by arterial and venous thromboembolism in patients who develop stroke complicating severe COVID-19 infections [8].
Recognizing stroke in COVID-19 patients can be difficult as presentations tend to be atypical with a high proportion of patients having non focal neurological presentations [9]. Cerebellar infarction after COVID-19 infection is extremely rare with only few sporadic cases reported in literature [10]. But these were a part of multiple infarcts involving other parts of the brain and we could not find any cases of isolated cerebellar stroke following COVID-19. Cerebellar symptoms such as ataxia in COVID-19 patients either during the acute phase or later, should prompt physicians to undertake further detailed targeted examination and investigations as there has been a case report of cerebellitis associated with COVID-19 without any associated infarction or hemorrhages [11]. Higher levels of biomarkers such as C-reactive protein, D-dimers, interleukin-6, ferritin, white blood cell count and platelet count are associated with increased severity of disease, quick progression and poor prognosis [12]. Apart from inflammatory markers, pre-existing diseases such as diabetes and hypertension, have been found to be risk factors for severe disease with neurological involvement [13]. This was very true in our patient too, who was poorly controlled diabetic and hypertensive increasing her risk for progression to severe disease. She was also found to have increased C-reactive protein, d-dimers and ferritin, even though her white blood cell and platelet count was normal. Interleukin-6 was not checked in our patient. Our patient was treated with antiplatelets which is the standard secondary prevention approach to cerebrovascular disease There are studies suggesting anticoagulation in all highrisk patients in view of the thrombotic tendency in COVID-19. But the duration and type of anticoagulation is still not clear [14].
Conclusion
Cerebellar stroke even though very rare in COVID -19 can be a serious complication especially in the presence of other risk factors. Clinicians should have a low threshold for investigating COVID-19 patients presenting with atypical features such as dizziness, vertigo and gait abnormalities. If not recognized early, it can result in neurological deterioration which may need surgical decompression. In view of the potential for hypercoagulative state in severe COVID-19 infection, prophylactic anticoagulation could be considered as a part of COVID-19 treatment regimens.
References
- Han C, Duan C, Zhang S, Spiegel B, Shi H, et al. (2020) Digestive Symptoms in COVID-19 Patients with Mild Disease Severity: Clinical Presentation, Stool Viral RNA Testing, and Outcomes. Am J Gastroenterol 115(6): 916-923.
- Whittaker A, Anson M, Harky A (2020) Neurological Manifestations of COVID-19: A systematic review and current update. Acta Neurol Scand 142(1): 14-22.
- Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, et al. (2020) Neurological associations of COVID-19. Lancet Neurol 19(9):767-783.
- Nannoni S, de Groot R, Bell S, Markus HS (2021) Stroke in COVID-19: A systematic review and meta-analysis. Int J Stroke 16(2): 137-149.
- Belani P, Schefflein J, Kihira S, Rigney B, Delman BN, et al. (2020) COVID-19 Is an Independent Risk Factor for Acute Ischemic Stroke. AJNR Am J Neuroradiol 41(8): 1361-1364.
- Perry RJ, Smith CJ, Roffe C, Simister R, Narayanamoorthi S, et al. (2020) Characteristics and outcomes of COVID-19 associated stroke: a UK multicentre case-control study. J Neurol Neurosurg Psychiatry 92(3): 242-248.
- Tan YK, Goh C, Leow AST, Tambyah PA, Ang A, et al. (2020) COVID-19 and ischemic stroke: a systematic review and meta-summary of the literature. J Thromb Thrombolysis 50(3): 587-595.
- Joly BS, Siguret V, Veyradier A (2020) Understanding pathophysiology of hemostasis disorders in critically ill patients with COVID-19. Intensive Care Med 46(8): 1603-1606.
- Katz JM, Libman RB, Wang JJ, Sanelli P, Filippi CG, et al. (2020) Cerebrovascular Complications of COVID-19. Stroke 51(9): 227-231.
- Patel HN, Syed A, Lobel JS, Galler R, Georges J, et al. (2020) Cerebellar infarction requiring surgical decompression in patient with COVID 19 pathological analysis and brief review. Interdiscip Neurosurg 22: 100850.
- Fadakar N, Ghaemmaghami S, Masoompour SM, Shirazi Yeganeh B, Akbari A, et al. (2020) A First Case of Acute Cerebellitis Associated with Coronavirus Disease (COVID-19): A Case Report and Literature Review. Cerebellum 19(6): 911-914.
- Henry BM, de Oliveira MHS, Benoit S, Plebani M, Lippi G (2020) Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med 58(7): 1021-1028.
- Hu Y, Sun J, Dai Z, Deng H, Li X, et al. (2020) Prevalence and severity of corona virus disease 2019 (COVID-19): A systematic review and meta-analysis. J Clin Virol 127: 104371.
- Flaczyk A, Rosovsky RP, Reed CT, Bankhead Kendall BK, Bittner EA, et al. (2020) Comparison of published guidelines for management of coagulopathy and thrombosis in critically ill patients with COVID 19: implications for clinical practice and future investigations. Crit Care 24(1): 559.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...