
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-6628
Review Article(ISSN: 2637-6628) 
An Overview of Definition and Approaches to Petroclival Meningioma Volume 4 - Issue 4
Alireza Khoshnevisan*
- Department of neurosurgery, Tehran university of medical sciences, Tehran, Iran
Received: September 28, 2020; Published: October 08, 2020
Corresponding author: Alireza Khoshnevisan, Associate professor of neurosurgery, Tehran university of medical sciences, Tehran, Iran
DOI: 10.32474/OJNBD.2020.04.000194
Abstract
Meningiomas account for 20 to 25% of all intracranial tumors and 10% are seen in the posterior fossa. Petroclival tumors are defined as arising from the upper two thirds of the clivus, medial to the trigeminal nerve at the petroclival junction. Brain CT scan and MRI are routinely used to evaluate tumor anatomy. The petrous temporal bone is a hindrance to resection of these tumors. Oftentimes neurosurgeons are unskilled with the anatomy of the petrous bone, and so suboccipital and pterional routes are usually preferred. Some authors have encouraged using traditional neurosurgical approaches to these tumors. In this manuscript we review tumor location and approaches used for resection of these challenging tumors.
Keywords: Meningioma; Petroclival; Approaches
Abbreviations:IAM: Internal Auditory Meatus; GTR: Gross total resection; NTR: Near total resection; STR: Subtotal resection.
Introduction
Meningiomas account for 20 to 25% of all intracranial tumors
and 10% are seen in the posterior fossa. Of posterior fossa
meningiomas, those rising from the petroclival region account
for 5 to 11% of meningiomas and thus 0.15% of all intracranial
tumors. Male to female ration is 1 to 4. Petroclival tumors are
defined as arising from the upper two thirds of the clivus, medial to
the trigeminal nerve at the petroclival junction, often extent to the
middle and approaches posterior cranial fossae, and can involve the
posterior cavernous sinus through the Meckel cave [1].
Growth rates were 0.81 mm/yr (Diameter) and 0.81 cm3/
yr (Volume). When only growing tumors were measured, the
mean growth rates were 1.16 mm/yr (Diameter) and 1.10 cm3/
yr (Volume). Untreated tumors may grow at a dissimilar rate than
resected tumors [2]. The petrous temporal bone is a hindrance for
tumor resection in this location. Oftentimes neurosurgeons are
unskilled with the anatomy of the petrous bone, and so suboccipital
and pterional routes are preferred. Some authors have encouraged
using traditional neurosurgical approaches to these tumors.
Discussion
To select an appropriate approach all patients typically undergo
CT to examine the bony architecture and relationships between the
skull base and tumor. MRI is routinely used to evaluate presence
of edema in the brainstem and soft-tissue relationships between
the CNS and the tumor. Angiography to evaluate the arterial supply
and relationship to major vessels is sometimes useful. Selection of
approach depends on location, size, extension of the tumor, venous
sinus anatomy and preoperative hearing evaluation.
Strategies to overcome the petrous temporal bone as an
obstacle are:
a) Resection of the petrous apex with the middle fossa
approach.
b) Resection of presigmoid, retrolabyrinthine petrous bone
with the posterior petrosal approach.
c) Resection of the entire petrous bone with complete
petrosectomy.
Mayberg and Symon believed that the combined sub temporalposterior
fossa approach provided the best results, as did Guthrie
et al. Various alterations of this approach have been described
by Samii et al. and Hakuba et al. Al-Mefty and co-workers have
described in detail a petrosal approach for these tumors [3].
Tumors that are medial to the internal auditory canal and extent
to both middle and posterior cranial fossae are often best treated
with a combined transpetrosal approach, which is particularly
true if there is a preoperative hearing deficit. The anterior petrosal
approach is best appropriate for smaller petroclival meningiomas
that do not spread lateral to the IAM. Once a tumor has extended
farther into the posterior fossa, lateral to the IAM, a posterior
petrosal approach should be used. A retrosigmoid craniotomy
remains a workhorse surgical approach for most petroclival tumors
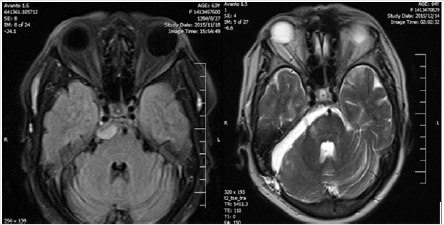
of any size (Figure 1).
Figure 1: Pre and post-operative MRI of small right petrocloval meningioma resected by retrosigmoid approach.
More Recently, the Endoscopic Endonasal Approach has
been “expanded” to the petroclival region. This approach
should be favored for extradural midline tumors (chordomas,
chondrosarcomas) or for cystic lesions when drainage is crucial [4].
GTR is only reported in an average of 49% of patients. Many highvolume
surgical centers have abandoned GTR for NTR or STR later
in their practice. Most describe that STR/NTR does not have an
increased risk or recurrence compared with GTR in most series [5].
Attempts at accomplishing gross- or near-total resections
are associated with an increased rate of morbidity and mortality.
(Adjunctive treatment options such as stereotactic radiosurgery is
attractive options). There has been a tendency to accept subtotal
resections in an effort to minimize neurological morbidity [6].
Radiation therapy is used if a satisfactory decompression cannot
be implemented or there is regrowth after radical subtotal removal
[3].
Motor deficits and facial nerve morbidity are the common
postoperative neurological complications. CSF leak occur in 10% of
patients. In spite of the high morbidity, >75% of patients return to
independence at 1 year, many of which will start again employment
[5].
Conclusion
Petroclival tumors also infrequent still remain a surgical challenge. The petrous temporal bone is an obstacle for tumor resection in this location. Oftentimes neurosurgeons are unfamiliar with the anatomy of the petrous bone, and so suboccipital and pterional routes are used. Some authors have advocated using traditional neurosurgical approaches to these tumors. The infrequency of the tumor, different treatment philosophies, and variations in reporting, complicate the outcome analysis and so choosing a definite approach for these tumors.
References
- H Richard Winn (2017) Youmans & Winn neurological surgery 4-Volume Set, 7th Edition. Elsevier Philadelphia, USA, Pp: 1108.
- Daniel M Fountain, Wai Cheong Soon, Tomasz Matys, Mathew R Guilfoyle, Ramez Kirollos, et al. (2017) Volumetric growth rates of meningioma and its correlation with histological diagnosis and clinical outcome: a systematic review. Acta Neurochir (Wien) 159 (3): 435-445.
- Ojemann Robert G (1992) Convexity Meningiomas. Clinical Neurosurgery. 40(17): 321-383.
- Timothée Jacquesson, Moncef Berhouma, Stéphane Tringali, Emile Simon, Emmanuel Jouanneau, (2015) Which routes for petroclival tumors? A comparison between the anterior expanded endoscopic endonasal approach and lateral or posterior routes. World Neurosurgery 83(6): 929-936.
- Michael L DiLuna, Ketan R Bulsara (2010) Surgery for Petroclival Meningiomas: A Comprehensive Review of Outcomes in the Skull Base Surgery Era. Skull Base 20(5): 337-342.
- Feng Xu, Ioannis Karampelas, Cliff A Megerian, Warren R Selman, Nicholas C Bambakidis (2013) Petroclival meningiomas: an update on surgical approaches, decision making, and treatment results. Neurosurg Focus 35(6): E11.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




