Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
ICSI Clinical Outcomes in Correlation to Supplementation of Vitamin D Agent Volume 3 - Issue 4
Amal Elshabrawy Elsayed*
- Obstetrics and Gynecology Department, Ain Shams University, Egypt
Received:August 06, 2019; Published: August 12, 2019
Corresponding author: Amal Elshabrawy Elsayed, Obstetrics and Gynecology Department, Ain Shams University, Egypt
DOI: 10.32474/IGWHC.2019.03.000169
Abstract
Background: With increased desires among both patients and physicians all over the world to get the optimum rates of success from ART management protocols, vitamin D is considered one of the crucial and demanding areas of research efforts that requires clarification of its exact role on various fertility aspects. Aim: to investigate whether vitamin D supplementation enhances ICSI outcomes in cases with vitamin D deficiency without clinical symptoms.
Methodology: A clinical research study 150 females cases having an age range of 18 to 38 years having serum Vitamin D level under 30ng/ml without symptoms of Vitamin D deficiency were recruited in the research study categorized into two research groups equally numbered placebo and vitamin D research group.
Results: Statistical comparative analysis of ICSI outcomes in Vitamin D and placebo research groups in which there was no statistical significant difference as regards number of oocyte, mean ± SD, Fertilization rate (%), Number of embryos, mean ± SD, good quality embryos (%) (p values=0.489, 0.860, 0.212, 0.405 consecutively), however there was statistically highly significant difference as regards endometrial grade (p value=0.001), besides statistically higher rates of chemical and clinical pregnancies among vitamin D research group cases in comparison to placebo research group (p values=0.002, 0.019 consecutively).
Conclusion: Vitamin D supplementation has a positive impact on pregnancy rates and endometrial lining thickness in ICSI practice however future research efforts should be multicentric in fashion taking in consideration racial and ethnic differences besides BMI as a variable that could affect the vitamin D status.
Keywords: Vitamin D; ICSI; ART
Introduction
Vitamin D metabolism and physiological impacts at cellular and hormonal levels is an issue of concern for all infertility specialists all over the globe. The complexity and cornerstone impacts on levels of enzymatic activities and hormonal regulation raised the research debate whether its deficiency or defective activity at receptor level could affect the fertility potential in both males and females [1- 3]. With increased desires among both patients and physicians all over the world to get the optimum rates of success from ART management protocols vitamin D is considered one of the crucial and demanding areas of research efforts that requires clarification of its exact role on various fertility aspects [4-6].
Infertility is multifactorial concerning its pathophysiological development in most clinical scenarios presented in every day practice and it is revealed and displayed by various investigators in numerous research studies to be influenced by various factors involving lifestyle, eating habits or nutritive issues [7-9].
Vitamin D deficiency, has been considered as one of the chief issues in fertility potential among both males and females at reproductive age .Vitamin D in its biochemical nature is a fat soluble vitamin that aids in calcium and phosphorous absorption and maintenance of normal musculoskeletal function beside its crucial role in general cellular metabolic functional activities in all cells situated all over the human body e.g. cellular growth and maturation [10-13].
Vitamin D receptor is classified as a member of nuclear receptor family of transcription factors forming a heterodimer in conjunction with retinoid-X receptor and binds to hormone response elements on DNA regulating specific gene products expressive activity [14-16]. Vitamin D receptors exist all over the female reproductive system involving endometrial epithelial cells, granulosa and cumulus oophorus within the ovary, fallopian tube epithelial cells. Vitamin D have a cornerstone role in biosynthesis of estrogen and progesterone steroid hormones besides the physiologically complex process of embryonic implantation that requires cellular harmony between the endometrial lining and the developing embryo [17-19].
Prior research groups have mentioned that there is prolonged time interval required for conception in cases having vitamin D deficiency although contradicting with other researchers in this aspect it has raised issues of concern among fertility practioners due to other researchers confirming the role of vitamin D supplementation in raising the success rates of IVF management protocols .on the other hand in an interesting manner fertility researchers have previously displayed among their findings that raised vitamin D serum level is linked with reduced embryonic quality and the biochemical and clinical pregnancy rates [20,21].
Aim of the Work
To investigate whether vitamin D supplementation enhances ICSI outcomes in cases with vitamin D deficiency without clinical symptoms.
Methodology
A clinical research study 150 females cases having an age range of 18 to 38 years having serum Vitamin D level under 30ng/ ml without symptoms of Vitamin D deficiency were recruited in the research study categorized into two research groups equally numbered placebo and vitamin D research group.
To exclude the impact of male factor of infertility and advanced maternal age, cases with abnormal semen indices based on WHO (2010) and/or female age above 38 years have been excluded from the research. Other exclusive research criteria have been secondary female infertility, polycystic ovarian disease, endometriosis, congenital or acquired uterine structural abnormalities, administration of agents that could affect Vitamin D absorption and metabolic pathways e.g. Antiepileptic agents, BMI under 18 or above 30kg/ m2 and hypothyroid cases.
High-performance liquid chromatography was used for vitamin D level assay induction of ovulation: all cases received a combination of recombinant follicle-stimulating hormone (FSH) and human menopausal gonadotrophins (hMG) and have been followed by sequential transvaginal sonography. Gonadotropin releasing hormone antagonist have been administered as the dominant follicular size reached around 12-14mm and continued till hCG trigger day. On hCG trigger day, number of developing follicles above 12mm and endometrial grade was also recorded. Endometrial grade was categorized as follows A (triple-line pattern composed of a central hyperechoic line surround by two hypoechoic layers); B (intermediate isoechogenic pattern with the same reflectivity as the surrounding myometrium and a poorly defined central echogenic line); and C (homogenous, hyperechogenic endometrial lining). Ovulation was induced by administration of 10000 IU hCG as dominant follicles reached a size of 17-18mm. tansvaginal sonographic guided ovum pick up was conducted 36 hours after hCG trigger.
Number of oocytes was recorded on the day of oocyte retrieval. Embryonic quality has been classified as “good quality” that had between 6-8 blastomeres with even size and less than 25% fragmentation. Clinical and chemical pregnancies were recorded, besides multiple gestational sacs have been considered as one clinical pregnancy.
Statistical Analysis
Data were collected, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS) version 23. The quantitative data were presented as mean, standard deviations and ranges when parametric. Also qualitative variables were presented as number and percentages. The comparison between groups regarding qualitative data was done by using Chi-square test and/ or Fisher exact test when the expected count in any cell found less than 5. The comparison between two independent groups with quantitative data and parametric distribution was done by using Independent t-test. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant at the level of < 0.05.
Results
Table 1 reveals and displays the statistical comparative analysis between the vitamin D and placebo research groups as regards basal and clinical characteristics of couples in which there was no statistically significant difference concerning female, male ages, duration of infertility, number of previous ART cycle, female education (%)(high school, Diploma, Master) and BMI (p values =0.144, 0.299, 0.187, 0.585, 0.767, 0.174 consecutively).
Table 1: Comparison of basal and clinical characteristics of couples in vitamin D and placebo groups.
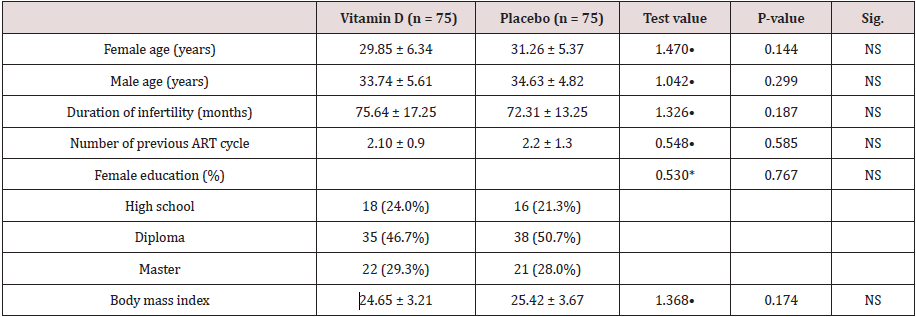
•: Independent t-test; *: Chi-square test
Table 2 and Figure 1 reveal and display the comparative statistical analysis between Vitamin D and placebo research groups regarding vitamin D level in which before intervention there was no statistical significant difference (p value=0.251) and after intervention there was statistically significant increase of vitamin D research group in comparison to placebo research group (p value <0.001).
Table 2: Comparison between Vitamin D and placebo groups regarding vitamin D level before and after intervention.
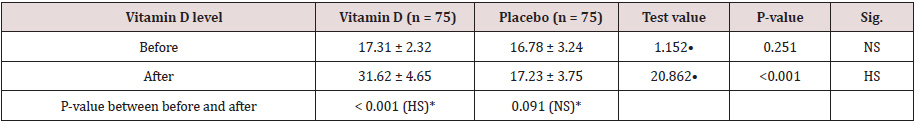
•: Independent t-test; *: Paired t-test
Figure 1: Comparison between Vitamin D and placebo groups regarding vitamin D level before and after intervention.
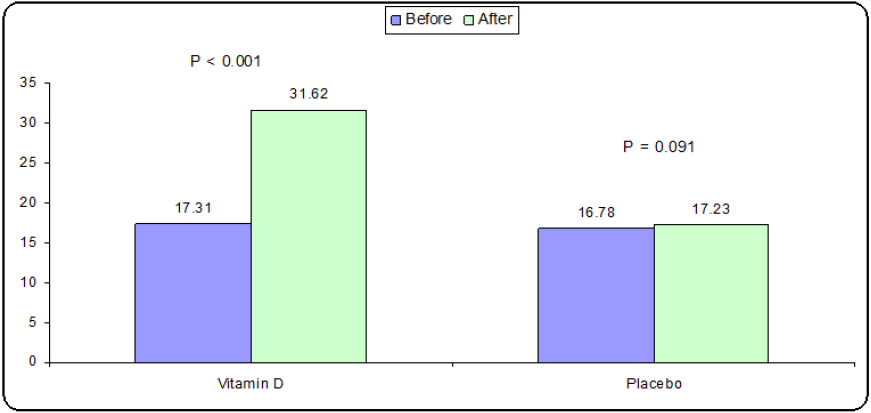
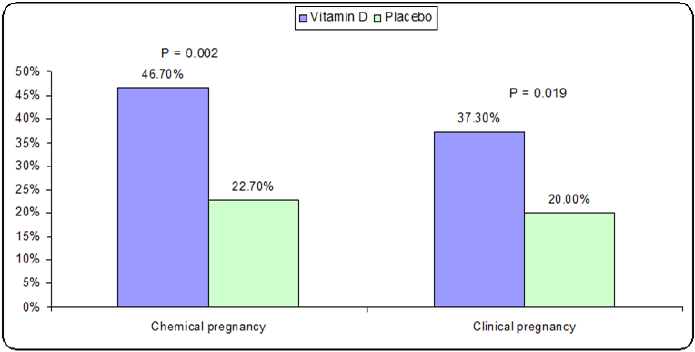
Table 3 and Figure 2 reveals and displays statistical comparative analysis of ICSI outcomes in Vitamin D and placebo research groups in which there was no statistical significant difference as regards number of oocyte, mean ± SD, Fertilization rate (%), Number of embryo, mean ± SD, good quality embryo (%)(p values=0.489, 0.860, 0.212, 0.405 consecutively) however there was statistically highly significant difference as regards endometrial grade (p value= 0.001), besides statistically higher rates of chemical and clinical pregnancies among vitamin D research group cases in comparison to placebo research group (p values=0.002,0.019 consecutively).
Table 3: Comparison of ICSI outcomes in Vitamin D and placebo groups.
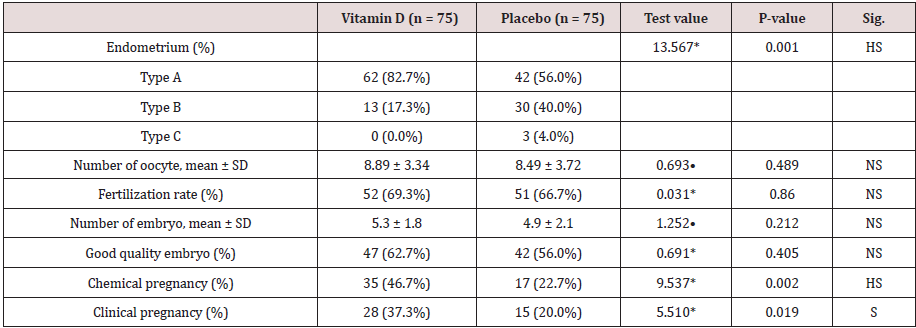
•: Independent t-test; *: Chi-square test
Discussion
Vitamin D has a cornerstone role in human reproduction, Vitamin D status evaluation and assay have been integrated in daily fertility practice. On the other hand, Vitamin D supplementation role during assisted reproductive management protocols is an issue of research debate [22,23].
A prior research debate revealed and displayed that despite demographic and fertility research characteristics between the two research groups, Vitamin D supplementation statistically significantly enhanced Vitamin D serum level in comparison to placebo research group [1,4,9].
Comparison of the mean value of serum Vitamin D between both research groups before intervention revealed no statistically significant difference between the two research groups and 50000 units of Vitamin D supplementation per week for 6 weeks based on a prior research study caused a statistically significant raise in serum level of Vitamin D in comparison to before management [3,7,13].
Indicating that the level of Vitamin D raised to higher than 30ng/l, the cut of value for Vitamin D deficiency, denoting that Vitamin D dosage supplementation is an efficient at enhancing the serum vitamin D level. Prior research groups have revealed and displayed that improved serum level of Vitamin D is correlated with statistically significant difference was noticed in endometrial lining but no statistical significant difference have been revealed and displayed that among investigated parameters, involving mature oocytes percentage, rates of fertilization and embryonic quality. Prior research groups in animal research studies that vitamin D receptors defective expression in mice cause them to suffer from uterine hypoplasia. Those research studies findings were justified “the activity of Vitamin D on estrogenic biosynthesis is explained by calcium homeostasis maintenance [10,16,19].
Another prior research group of investigators have reveled and displayed among their findings that the mean value of serum vitamin D, oocytes number, oocytes fertilized and endometrial lining thickness was statistically significantly higher in women who got pregnant by ICSI procedures, a statistically significant positive correlation was observed as regards vitamin D levels and rates of clinical pregnancy and endometrial thickness. Another research team of investigators in similar prior research study to the current study have come to the conclusion that vitamin D deficiency delays reaching to the optimal endometrial thickness required for implantation of embryo after ICSI management protocols [2,21].
Furthermore another research group of investigators have shown among their results that administering Vitamin D agent is an efficient line in enhancing the ICSI clinical outcomes. Those research findings are in harmony and similarity to the current study findings and could be justified by the fact that vitamin D is a crucial hormone in cellular growth, maturation with critical value in enhancing endometrial receptivity [15,23].
Conclusion and Recommendations
Vitamin D supplementation has a positive impact on pregnancy rates and endometrial lining thickness in ICSI practice however future research efforts should be multicentric in fashion taking in consideration racial and ethnic differences besides BMI as a variable that could affect the vitamin D status.
References
- Polyzos NP, Anckaert E, Guzman L, Schiettecatte J, Van Landuyt L, et al. (2014) Vitamin D deficiency and pregnancy rates in women undergoing single embryo, blastocyst stage, transfer (SET) for IVF/ICSI. Hum Reprod 29(9): 2032-2040.
- Abdullah UH, Lalani S, Syed F, Arif S, Rehman R (2017) Association of Vitamin D with outcome after intra cytoplasmic sperm injection. J Matern Fetal Neonatal Med 30(1): 117-120.
- Vanni VS, Vigano' P, Somigliana E, Papaleo E, Paffoni A, et al. (2014) Vitamin D and assisted reproduction technologies: current concepts. Reprod Biol Endocrinol 12: 47.
- Zhao J, Zhang Q, Li Y (2012) The effect of endometrial thickness and pattern measured by ultrasonography on pregnancy outcomes during IVF-ET cycles. Reprod Biol Endocrinol 10: 100.
- Aflatoonian A, Arabjahvani F, Eftekhar M, Sayadi M (2014) Effect of Vitamin D insufficiency treatment on fertility outcomes in frozen-thawed embryo transfer cycles: a randomized clinical trial. Iran J Reprod Med 12(9): 595-600.
- Diamond T, Wong YK, Golombick T (2013) Effect of oral cholecalciferol 2,000 versus 5,000 IU on serum Vitamin D, PTH, and bone and muscle strength in patients with Vitamin D deficiency. Osteoporos Int 24(3): 1101-1105.
- Spedding S, Vanlint S, Morris H, Scragg R (2013) Does Vitamin D sufficiency equate to a single serum 25-hydroxyVitamin D level or are different levels required for non-skeletal diseases? Nutrients 5(12): 5127-5139.
- Asadi M, Matin N, Frootan M, Mohamadpour J, Qorbani M, et al. (2014) Vitamin D improves endometrial thickness in PCOS women who need intrauterine insemination: a randomized double-blind placebo-controlled trial. Arch Gynecol Obstet 289(4): 865-870.
- Luk J, Torrealday S, Neal Perry G, Pal L (2012) Relevance of vitamin D in reproduction. Hum Reprod 27(10): 3015-3027.
- de Angelis C, Galdiero M, Pivonello C, Garifalos F, Menafra D, et al. (2017) The role of vitamin D in male fertility: a focus on the testis. Rev Endocr Metab Disord 18(3): 285-305.
- Voulgaris N, Papanastasiou L, Piaditis G, Angelousi A, Kaltsas G, et al. (2017) Vitamin D and aspects of female fertility. Hormones (Athens) 16(1): 5-21.
- Paffoni A, Ferrari S, Vigano P, Pagliardini L, Papaleo E, et al. (2014) Vitamin D deficiency and infertility: insights from in vitro fertilization cycles. J Clin Endocrinol Metab 99(11): E2372-E2376.
- Dressler N, Chandra A, Aguirre Dávila L, Spineli LM, Schippert C, et al. (2016) BMI and season are associated with Vitamin D deficiency in women with impaired fertility: a two-centre analysis. Arch Gynecol Obstet 293(4): 907-914.
- Long MD, Sucheston-Campbell LE, Campbell MJ (2015) Vitamin D receptor and RXR in the post-genomic era. J Cell Physiol 230(4): 758-766.
- Nandi A, Sinha N, Ong E, Sonmez H, Poretsky L (2016) Is there a role for vitamin D in human reproduction? Horm Mol Biol Clin Investig 25(1): 15-28.
- Muscogiuri G, Altieri B, de Angelis C, Palomba S, Pivonello R, et al. (2017) Shedding new light on female fertility: the role of vitamin D. Rev Endocr Metab Disord 18(3): 273-283.
- Lerchbaum E, Obermayer Pietsch B (2012) Vitamin D and fertility: a systematic review. Eur J Endocrinol 166(5): 765-778.
- Pagliardini L, Vigano' P, Molgora M, Persico P, Salonia A, et al. (2015) High prevalence of vitamin D deficiency in infertile women referring for assisted reproduction. Nutrients 7(12): 9972-9984.
- Somigliana E, Paffoni A, Lattuada D, Colciaghi B, Filippi F, et al. (2016) Serum levels of 25-hydroxyvitamin D and time to natural pregnancy. Gynecol Obstet Invest 81(5): 468-471.
- Møller UK, Streym S, Heickendorff L, Mosekilde L, Rejnmark L (2012) Effects of 25OHD concentrations on chances of pregnancy and pregnancy outcomes: a cohort study in healthy Danish women. Eur J Clin Nutr 66(7): 862-868.
- Pacis MM, Fortin CN, Zarek SM, Mumford SL, Segars JH (2015) Vitamin D and assisted reproduction: should Vitamin D be routinely screened and repleted prior to ART? A systematic review. J Assist Reprod Genet 32(3): 323-335.
- Rudick BJ, Ingles SA, Chung K, Stanczyk FZ, Paulson RJ, et al. (2014) Influence of Vitamin D levels on in vitro fertilization outcomes in donor-recipient cycles. Fertil Steril 101(2): 447-452.
- Garbedian K, Boggild M, Moody J, Liu KE (2013) Effect of Vitamin D status on clinical pregnancy rates following in vitro fertilization. CMAJ Open 1(2): E77-E82.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...