Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Fetal rate of Urine Production in Preterm Premature Rupture of Membranes Clinical Scenarios Volume 3 - Issue 5
Naglaa Hussien1* and Mohamed Hashem El Refaey2
- 1Obstetrics and Gynecology Department, Faculty of Medicine, Tanta University, Tanta, Egypt
- 2Diagnostic Radiology Department, Faculty of Medicine, Tanta University, Tanta, Egypt
Received:September 03, 2019; Published: September 23, 2019
Corresponding author: Naglaa Hussien, Lecturer of Obstetrics and Gynecology, Obstetrics and Gynecology Department, Faculty of Medicine, Tanta University, Tanta, Egypt
DOI: 10.32474/IGWHC.2019.03.000173
Abstract
Background: Preterm premature rupture of membranes is a chief clinical scenario in obstetrics causing morbidity and mortality issues at maternal and fetal levels.
Aim: To investigate the correlation and linkage between fetal urinary production rate measured by sonography, and adverse neonatal clinical outcomes in cases with preterm premature rupture of membranes.
Methodology: A prospective observational clinical research trial of cases that are singleton gestations diagnosed having PPROM from 24+0 to 34+6 gestational weeks, from January 2016 and March 2019. Gestational age determination was made using the last menstrual period and verified by first trimester sonography. exclusive research criteria were as follows cases that had spontaneous delivery within 48 hours of PPROM, other gestational medical complications (e.g. DM, hypertension), and cases having fetal congenital malformations PPROM diagnosis have been performed using sterile speculum examination and pH assessment of fluid obtained from the posterior vaginal fornix.
Results: The statistical correlation between adverse neonatal outcome and fetal urinary production rate, adjusted for gestational age comparing between FUPR in neonates with adverse outcome and FUPR in neonates without adverse outcome in which there was no statistical significant difference between both research categorical groups as regards reduced urine output in first 24 hours, Positive cultures (urine, blood, CSF), Early sepsis (p values =0.196, 0.673, 0.192 consecutively) whereas NEC or IVH occurrence and requirement for Blood products transfusion was statistically significantly different between FUPR in neonates with adverse outcome and FUPR in neonates without adverse outcome (p value= 0.001, 0.006 consecutively).
Conclusion: The current study findings reveal that the determination of fetal urinary production rate is one of the cornerstone tools that could be used to predict the arousal of adverse clinical events at maternal and perinatal levels in preterm premature rupture of membranes. Combined with other tools also not overlooking other pathological tests including c-reactive proteins, creatinine.
Introduction
Preterm premature rupture of membranes is a chief clinical scenario in obstetrics causing morbidity and mortality issues at maternal and fetal levels. A real challenge which exists in decision making is to balance between fetal maturity and wellbeing on one hand and risk of pregnancy continuation with arousal of highly risky situation such as chorioamnionitis clinical, sonographic and biomarkers are required to elucidate the possible clinical situation that could arise that would enlighten the decision making in those complex clinical scenarios [1-3].
Noninvasive investigative modes such as serum C-reactive protein, was observed by prior research groups of investigators to have a low predictability potential with inadequate sensitivity although widely performed in practice to predict imminent intrauterine infectious issues in conjunction to total leucocytic count [4-6].
The pathophysiological origin and course of preterm birth and PPROM is correlated to preliminary fetal inflammatory response syndrome that is directly correlated to intrauterine infection, denoting multi-organ affection of the fetus involving the fetal kidneys, that could consequently affect the fetal urinary rate production that would affect the clinical sequalae and prognosis of the neonatal clinical status [7-9].
Aim of the Work
To investigate the correlation and linkage between fetal urinary production rate measured by sonography, and adverse neonatal clinical outcomes in cases with preterm premature rupture of membranes.
Methodology
This study was done at Tanta University hospital in the Obstetrics & Gynecology and Radiology departments
A prospective observational clinical research trial of cases that are singleton gestations diagnosed having PPROM from 24+0 to 34+6 gestational weeks, from January 2016 and March 2019.
Gestational age determination was made using the last menstrual period and verified by first trimester sonography. exclusive research criteria were as follows cases that had spontaneous delivery within 48 hours of PPROM, other gestational medical complications (e.g. DM, hypertension), and cases having fetal congenital malformations PPROM diagnosis have been performed using sterile speculum examination and pH assessment of fluid obtained from the posterior vaginal fornix.
All research study subjects have undergone sonographic evaluation involving fetal presentation, EFW, and amniotic fluid index were established. Fetal urine production rate has been evaluated within 24-48 hours of PPROM and adjusted for gestational age. Assessment of FUPR was performed by ultrasound measurement of change in fetal bladder volume over time fetal bladder measurements were obtained every 1 to 2 minutes for around 45 minutes till observing a full bladder cycle (filling and emptying). Fetal bladder measurements have been evaluated at admission with calculation of fetal urine production rate (mL/ hour).
Maternal and neonatal clinical outcomes e.g. chorioamnionitis, placental inflammatory grade, neonatal first creatinine value, length of Neonatal Intensive Care Unit admission, necrotizing enterocolitis diagnosis or intraventricular hemorrhage, blood transfusion, reduced neonatal urine production rate (<4mL/ kg/h), positive culture, and/or early neonatal sepsis all have been recorded for analysis .A total 120 cases were initially recruited cases were excluded if they developed any of the previously mentioned exclusive research criteria leaving a net number of 33 cases that met inclusive research criteria.
Statistical Analysis
Data were collected, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS) version 23. Data were presented as mean and standard deviations for quantitative data with parametric distribution; median with Inter-Quartile Range (IQR) for quantitative data with non-parametric distribution and numbers and percentages for qualitative data. The comparison between two groups was done using independent t-test for parametric and Mann-Whitney test for non-parametric and Chisquare test for qualitative data. Spearman correlation coefficients were used to assess the correlation between fetal urine production rate and duration of NICU stay. The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant at the level of < 0.05.
Results
Table 1 reveal sand displays the comparative statistical analysis between the FUPR group and Singleton PPROM group in which there was no statistical significant difference between both research groups as regards the maternal age (years), mean ± SD, education (years), median (IQR), parity median (IQR), previous cesarean delivery no. (%), gestational age (weeks), mean ± SD, Spontaneous onset of labor, no. (%), Mode of delivery, no. (%), Hospital length of stay (days), mean ± SD (p values =0.385, 0.614, 0.821, 0.278, 0.329, 0.557, 0.881, 0.087 consecutively).
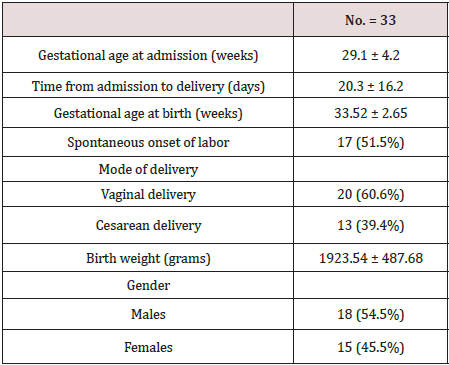
Table 1: Comparison of maternal characteristics and outcomes for the two study groups. Data were presented as mean and standard deviations, median (IQR) and numbers and percentages •: Independent t-test; ≠: Mann-Whitney test; *: Chi-square test.
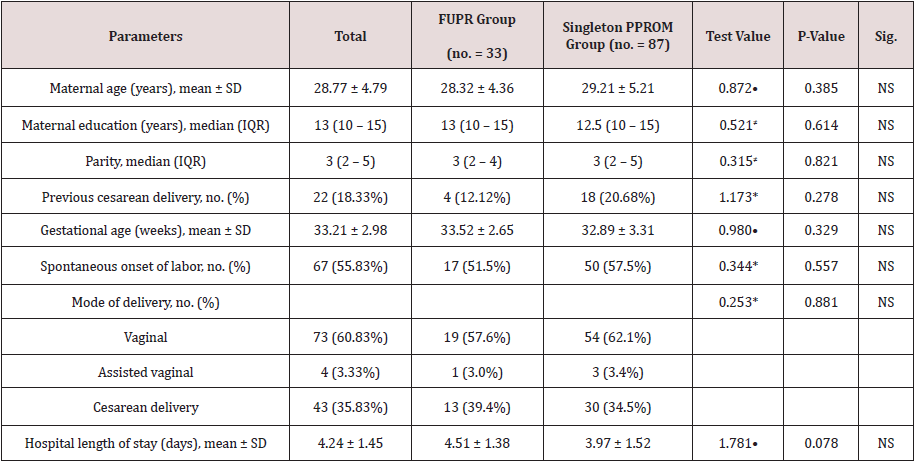
Table 2 reveals and displays the maternal and neonatal descriptive features of recruited research study subjects in which Mean +/-SD Gestational age at admission (weeks), Time from admission to delivery (days), Gestational age at birth (weeks), Birth weight (grams)= 29.1 ± 4.2, 20.3 ± 16.2, 33.52 ± 2.65, 1923.54 ± 487.68 consecutively, whereas 17 cases had spontaneous onset of labor representing 51.5% of recruited cases ,20 cases had vaginal delivery representing 60.6% of recruited cases whereas 13 cases had cesarean section delivery representing 39.4% of the total number recruited. As regards the gender of the neonates delivered there was 18 males (54.5%), 15 females (45.5%).
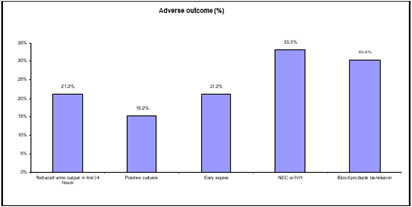
Figure 1 reveals adverse outcomes percentage in which reduced urine output in first 24 hours represented 21.2% of adverse outcomes, positive cultures 15.2 %, early sepsis 21.2%, NEC or IVH 33.3%, blood products transfusion 30.
Table 3 and Figure 2 reveals and displays the statistical correlation between adverse neonatal outcome and fetal urinary production rate, adjusted for gestational age comparing between FUPR in neonates with adverse outcome and FUPR in neonates without adverse outcome in which there was no statistical significant difference between both research categrorial groups as regards Reduced urine output in first 24 hours, Positive cultures (urine, blood, CSF), Early sepsis (p values =0.196, 0.673, 0.192 consecutively) whereas NEC or IVH occurrence and requirement for Blood products transfusion was statistically significantly different between FUPR in neonates with adverse outcome and FUPR in neonates without adverse outcome (p value =0.001,0.006 consecutively).
Table 3: Relation between adverse neonatal outcome and fetal urinary production rate, adjusted for gestational age. FUPR: Fetal Urinary Production Rate; CSF: Cerebrospinal Fluid; NEC: Necrotizing Enterocolitis; IVH: Intraventricular Hemorrhage. •: Independent t-test.
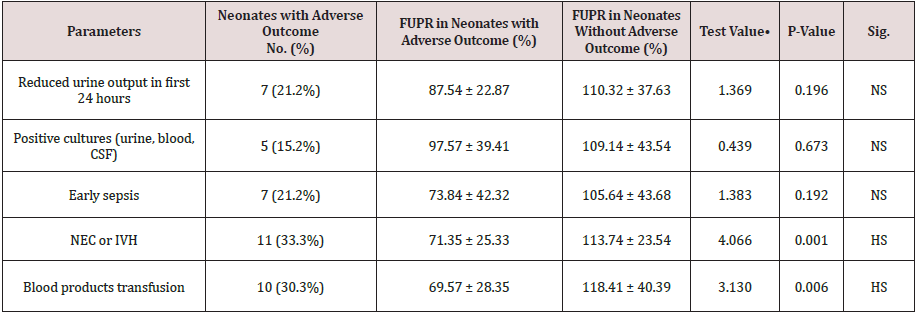
Figure 2: Comparative analysis FUPR in neonates with adverse outcome and FUPR in neonates without adverse outcome.
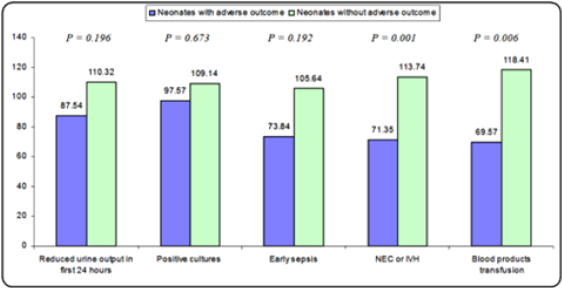
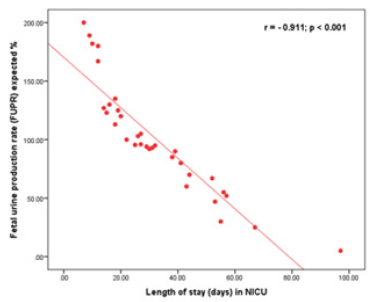
Figure 3 The correlation between percent of expected Fetal Urine Production Rate (FUPR) and Neonatal Intensive Care Unit (NICU) length of stay (days) (r=0.911, p value <0.001).
Figure 3: The correlation between percent of expected fetal urine production rate (FUPR) and neonatal intensive care unit (NICU) length of stay (days) (r=0.911, p value <0.001).
Discussion
Preterm premature rupture of membranes prediction of clinical risk of occurrence is an obstetric challenge since it is of great concern the neonatal clinical outcome that could be affected particularly when delivery is delayed and chorioamnionitis develops. The fetal urinary production is one of the cornerstone areas of research interest that determines the intactness of the physiological fetus hemostasis that could be implemented in future clinical practice as a sign that could reveal if any unfavorable outcomes could arise due to systemic inflammatory response at molecular and cellular levels which could affect the fetal renal function one of the pathological responses to fetal systemic inflammatory response is preterm premature rupture of membranes that could occur due to raised inflammatory mediators such as prostaglandins [10- 12]. A prior research study like the current study in approach and methodology have revealed and displayed that lower range fetal urinary production could be a critical for pathological development of chorioamnionitis and adverse neonatal clinical outcomes. A possible justification for the correlation between oligohydramnios development and fetal inflammatory response syndrome is the inherent antimicrobial properties of amniotic fluid in conjunction to reduced renal blood flow consequently resulting in oligohydramnios [12,13]. A prior research group of investigators have demonstrated that the mean fetal urine rate of production rise from 5mLper hour at 20 gestational weeks’ to 51mL per hour at 40 gestational weeks. serial bladder volume measuring using a 2D sonographic technique, including bladder filling and emptying full cycle was previously used by prior research teams of investigators besides other techniques assessing fetal blood flow redistribution pattern, e.g. Doppler sonography have the privilege that to quantify renal blood flow [1,4,6]. Physiologically the process of fetal urinary production is complex in nature due to interaction between, diuretic and antidiuretic factors interestingly it was shown similar to the current study findings it was previously demonstrated by investigators that that fetal rate of urine production in PPROM clinical scenarios is correlated and linked in a statistically significant fashion to occurrence of chorioamnionitis and perinatal morbidity issues such as, necrotizing enterocolitis early onset neonatal sepsis, and longer NICU admission. furthermore, in a similar manner to the current study findings it was shown by previous research groups that the decreased rate of fetal urine production is correlated to reduced neonatal urine production rate within the 24 first hours of life that verifies the technique implemented in measuring the in-utero urinary production rate of the fetus. Interestingly showing great harmony with the current study results it was previously observed that the fetal urinary production rate is not correlated to placental pathology [2,7,9].
Conclusion and Recommendations for Future Research
The current study findings reveal that the determination of fetal urinary production rate is one of the cornerstone tools that could be used to predict the arousal of adverse clinical events at maternal and perinatal levels in preterm premature rupture of membranes, however future research studies are recommended to be multicentric in fashion with larger sample sizes to verify the current study findings. Recommend a longer study period and a larger sample size. Also, to look at the mother’s health status e.g. diabetic, HIV, hepatitis, history of sexually transmitted infections like syphilis.
References
- Hofer N, Kothari R, Morris N, Muller W, Resch B (2013) The fetal inflammatory response syndrome is a risk factor for morbidity in preterm neonates. Am J Obstet Gynecol 209(6): 542 e1- 542 e11.
- Frenette P, Dodds L, Armson BA, Jangaard K (2013) Preterm prelabour rupture of membranes: Effect of latency on neonatal and maternal outcomes. J Obstet Gynaecol Can 35(8): 710-717.
- Pappas A, Kendrick DE, Shankaran S, Stoll BJ, Bell EF, et al. (2014) Chorioamnionitis and early childhood outcomes among extremely low-gestational-age neonates. JAMA Pediatr 168(2): 137-147.
- Oh KJ, Park KH, Kim SN, Jeong EH, Lee SY, et al. (2011) Predictive value of intra-amniotic and serum markers for inflammatory lesions of preterm placenta. Placenta 32(10): 732-736.
- Romero R, Dey SK, Fisher SJ (2014) Preterm labor: one syndrome, many causes. Science 345(6198): 760-765.
- Kim CJ, Romero R, Chaemsaithong P, Chaiyasit N, Yoon BH, et al. (2015) Acute chorioamnionitis and funisitis: Definition, pathologic features, and clinical significance. Am J Obstet Gynecol 213(4 Suppl): S29-52.
- Heyden JL, Ham DP, Kuijk S, Notten KJ, Janssen T, et al. (2013) Outcome of pregnancies with preterm prelabor rupture of membranes before 27 weeks' gestation: a retrospective cohort study. Eur J Obstet Gynecol Reprod Biol 170(1): 125-130.
- Gezer A, Parafit Yalciner E, Guralp O, Yedigoz V, Altinok T, et al. (2013) Neonatal morbidity mortality outcomes in pre-term premature rupture of membranes. J Obstet Gynaecol 33(1): 38-42.
- Mura T, Picaud JC, Larroque B, Galtier F, Marret S, et al. (2013) Cognitive impairment at age 5 years in very preterm infants born following premature rupture of membranes. J Pediatr 163(2): 435-440.
- Melamed N, Ben Haroush A, Pardo J, Chen R, Hadar E, et al. (2011) Expectant management of preterm premature rupture of membranes: Is it all about gestational age? Am J Obstet Gynecol 204(1): 48 e1-8.
- Ham DP, Heyden JL, Opmeer BC, Mulder AL, Moonen RM, et al. (2012) Management of late-preterm premature rupture of membranes: The PPROMEXIL-2 trial. Am J Obstet Gynecol 207(4): 276 e1-10.
- Kim CJ, Romero R, Chaemsaithong P, Kim JS (2015) Chronic inflammation of the placenta: Definition, classification, pathogenesis, and clinical significance. Am J Obstet Gynecol 213(4 Suppl): S53-69.
- Hoseini R, Otukesh H, Rahimzadeh N, Hoseini S (2012) Glomerular function in neonates. Iran J Kidney Dis 6(3): 166-172.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...