Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
A Clinico Pathological Correlation Study of Leiomyoma of Uterus-An Institutional Experience Volume 3 - Issue 4
Kavya Kota* and Manchuru Aruna
- Department of Obstetrics and Gynaecology, JJM Medical College, Davangere, Karnataka, India
Received:July 29, 2019; Published: August 05, 2019
Corresponding author: Kavya Kota, Department of Obstetrics and Gynaecology, JJM Medical College, Davangere, Karnataka, India.
DOI: 10.32474/IGWHC.2019.03.000167
Abstract
Background: Leiomyoma of the uterus forms the most common type of benign tumour of the uterus and also most common pelvic tumour in women. The symptomatology continues to be variable. Surgery has for long been the main mode of therapy for the myomas. For women who wish to retain their uterus for future pregnancies or other reasons myomectomy is known. Recent trend has been towards non surgical approaches like GnRH hormone analogues or agonists, RU486 or selective uterine artery embolization, Laparoscopic cryoablation, radio frequency thermal ablation, MRGUS.
Objective: To analyse the clinico pathological spectrum in cases of Leiomyoma of the uterus in JJM Medical College to know the pattern of presentation, pathological co relation with type of fibroid and endometrial and ovarian changes. Materials and methods: A clinical study of 200 cases of fibroid uterus was made in Department of Obstetrics and Gynaecology, JJM Medical College, Davangere, from July 2016 to May 2019. The cases were selected by random allocation and detailed examination, clinical examination and investigations were made.
Results: Leiomyoma is the most common benign tumour of the uterus commonly found in women of childbearing age, in the third decade 55%. Most common mode of presentation is menstrual disturbances 76% amongst which menorrhagia was seen in 54% of cases, primary infertility was seen in 15% of patients, intramural fibroids are the most common variety accounting for 60%, endometrial pattern was proliferative in 66%, cystic ovaries were seen 8% of patients and adenomyosis in 16% indicating hyperestrogenism.
Conclusion: Leiomyoma is the most common benign tumour of the pelvis commonly affecting women of childbearing age, most common in 3rd decade, most common in multipara. Most common presentation of leiomyoma is menstrual disturbances. Intramural is the most common variety, proliferative and hyperplastic endometrium was commonly reported. The presence of proliferative endometrium, adenomyosis and cystic ovaries are all indicative of hyperestrogenic state associated with development of fibroids.
Keywords: Fibroid; Leiomyoma; Hyperestrogenism; GnRH hormone; Endometrium
Introduction
Leiomyoma of uterus forms the most common type of benign tumour of uterus, and also most common pelvic tumour in women [1]. It occurs one in every four or five women of reproductive age. Fibroid is an estrogen dependent tumour. It is believed that symptomatology depends on number, size and location of tumour, although most leimoyomas are believed to be asymptomatic and progress slowly [2]. Due to their wide spectrum of clinical symptoms like menstrual irregularities, pelvic pain, infertility they represent tremendous public health burden on women and economic costs to the society. They assume importance particularly in our country as they are an important cause for anaemia. So, strategies are needed to prevent the formation, to limit the growth and to treat non surgically [3].
Surgery has for long been the main mode of therapy for the myomas. For women who have completed childbearing, hysterectomy forms an attractive option as it eliminates both symptoms and chances of recurrence [4]. For women who wish to retain the uterus for future pregnancies or other reasons myomectomy is known. Recent trend has been, towards non-surgical approaches like GnRH hormone analogs/agonists, RU 486,22 or selective uterine artery embolization, laparoscopic cryoablation, radiofrequency thermal ablation, magnetic resonance guided ultrasound [5-9].
Objective
To analyse the clinico pathological spectrum in cases of Leiomyoma of the uterus in JJM Medical College to know the pattern of presentation, pathological co relation with type of fibroid and endometrial and ovarian changes.
Materials and Methods
a) Health care setup-Tertiary care hospital
b) Setting-Department of Obstetrics & Gyanecology, Bapuji
Hospital, Chigateri General Hospital and Women & Child Hospital attached to JJM Medical College, Davangere, Karnataka.c) Duration of the study-July 2016 to May 2019 (3 years)
d) Type of the study-Observational study
e) Sample size-200
f) Sampling technique-Random sampling
After getting IEC clearance from the institute and informed written consent from the patients enrolled in our study, they were subjected for thorough examination. On admission, a detailed history, clinical examination and investigations were made. The following points were note in the history.
i. Age and Socio-economic status of the patient.
ii. History of presenting complaints-Menstrual disorder (Menorrhagia / Metrorrhagia / Polymenorrhea / Dysmenorrhea / Post menopausal bleeding), white discharge per vagina, bladder and bowel symptoms and mass per abdomen
iii. Menstrual history-Age of menarche, past menstrual cycle, last menstrual period, date of sterilisation and age of menopause.
iv. Obstetric history-Duration of marriage, abortions, deliveries - preterm/term, nature of delivery and 3rd stage complications
v. Local examination-Per abdomen, per speculum, per vaginum and sounding of the uterus was done.
The diagnosis of fibroid uterus was made by clinical examination in majority of our patients, considering the menstrual history, firm mass in the hypogastric region, transmitting movement from cervix to mass and vice versa. Examination under general anaesthesia was not made in our studies. Diagnosis was confirmed by scanning in all cases. Diagnostic curettage was done to rule out any endometrial pathology especially in elderly patients and to know the hormonal status in infertile patients. In patients with infertility, semen analysis of husband and tubal testing were made before undertaking conservative surgery. All routine investigations were done for all cases. Intravenous pyelography and hysterosalpingography were done in selected cases.
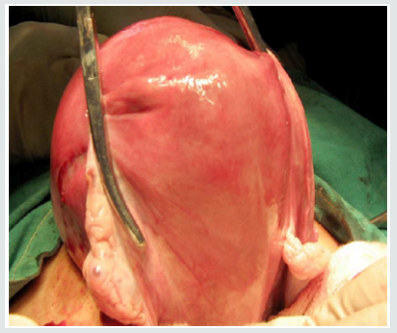
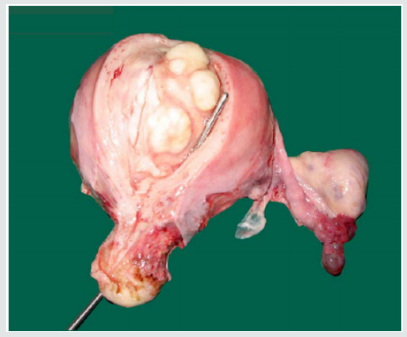
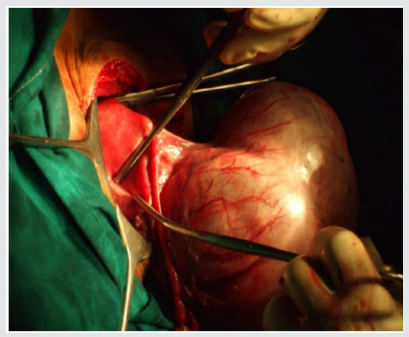
At laparotomy, the size of uterus, number and situation of fibroids, condition of tubes and ovaries were noted. In cases posted for myomectomy, tubal patency was tested utilising methylene blue. The ovaries were conserved in cases of hysterectomies unless associated with pathology and in elderly patients. The removed specimen was cut anteriorly in the midline and near the cornu to inspect the cavity and seedling fibroids. The specimen was sent for histopathological examination of endometrial and myometrium.
The microscopic examination were done to confirm the lesions, for degenerative changes, associated endometrial pathology & adenomyosis and for the changes in the ovaries, tubes and cervix. The descriptive analytical statistics were evaluated statistically with IBM SPSS Statistics for Windows, Version 20.0, IBM Corp, Chicago, IL
Results
Leiomyoma is the most common benign tumour of the pelvis. It accounts to maximum gynaecology admissions in our institute, and forms the most common indication for hysterectomy. A total of 200 cases were selected for the study
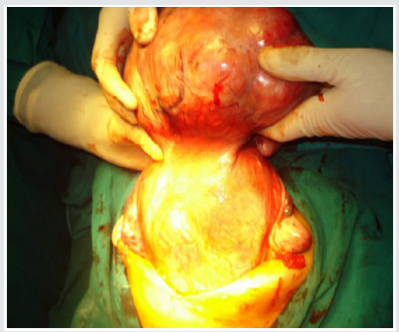
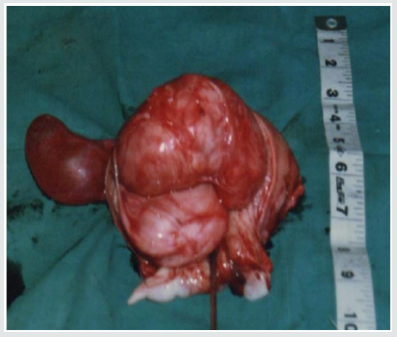
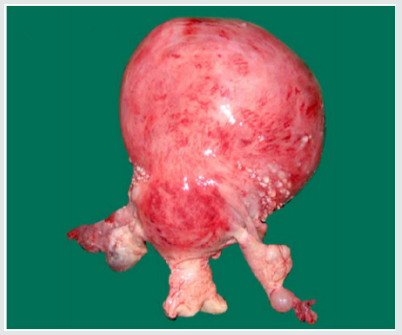
Leiomyomas are most commonly seen in the women of child bearing age, most commonly occurring in the 3rd decade (55%) followed by 4th decade (32%), 2nd decade (10%) and 5th decade (3%) with the mean age being 39 years. The youngest patient in our study was 24 years old, and the oldest was 55 years old. Though Leiomyoma is a disease of low parity, in our study, we have noted it to be common in multiparous women (94%). The interval between last delivery and development of symptoms in most of the cases were significantly long, which in 32% of the cases were 16-20 years back, and in 23% of the cases were more than 20 years back. There was a case within 5 years of last child birth (Figures 1-3).
Figure 2: Incidence of various surgeries performed
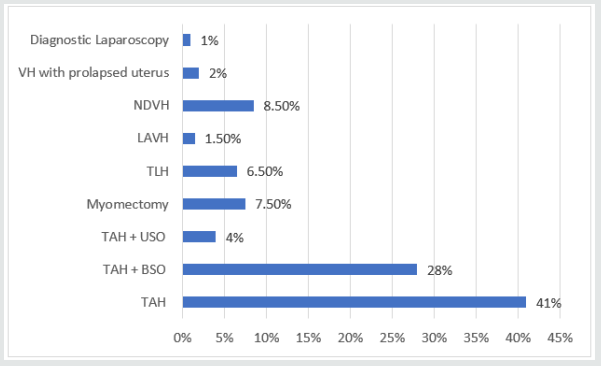
[TAH – Total abdominal hysterectomy; TAH-BSO – Total abdominal hysterectomy with bilateral salpingo-oopherectomy; TAH-USO – Total abdominal hysterectomy with unilateral salpingo-oopherectomy; TLH – Total laparoscopic hysterectomy; LAVH – Laparoscopic assisted vaginal hysterectomy; NDVH – Non descent vaginal hysterectomy].
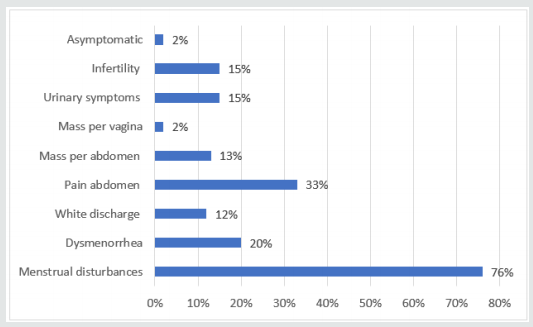
Dysmenorrhea were seen in 20% of the cases. Spasmodic dysmenorrhoea occurs in intramural and submucous fibroid. Congestive dysmenorrhoea resulted from increased vascularity in the pelvis, due to associated pelvic pathology. White discharge per vaginum were seen in 12% of the cases, which were most commonly associated with chronic cervicitis, also seen in cases of fibroid polyp and prolapse. Pain abdomen were seen in 33% of the cases, in most of the cases pain were associated with cystic ovaries, in others pain were due to endometriosis, PID, urinary tract infection or cholelithiasis. The presence of a mass were complained in 13% of the cases. Urinary problems were noticed in 15% of the cases, which typically associated with cervical fibroid / broad ligament fibroid. Primary infertility were observed in 15% of the patients, whether infertility was due to fibroid. The associated male factor for infertility was found only in 1 patient. None of the patients presented with bowel discomfort. Other symptoms like vomiting, fever, post coital bleeding, swelling of lower limbs, mass per vaginum & abdominal discomfort were observed in 5% of the cases. Anaemia was seen 40% of the cases (40% severely anaemic, 30% moderately anaemic & 30% mildly anaemic).
All the patients were hospitalized, after detailed examination and investigations, the patients were treated for anaemia and other medical disorders. All the patients underwent surgery depending on the age of the patient, associated and pathology. In our study, most of the patients presented with menstrual disturbances (76%). Amongst which menorrhagia (84.3%) were seen most commonly with intramural, subserous and submucous fibroids. In subserous fibroid, the menorrhagia was due to associated endometrial hyperplasia. The other menstrual disturbances like metrorrhagia (15.6%), polymenorrhagia (4.6%), polymenorrhea (12.5%) and postmenopausal bleeding (1.3%). Only one case of postmenopausal bleeding was found which was associated with concomitant adenomyosis.
In our study, 41% patients underwent TAH, 28% TAH-BSO, 4% underwent TAH-USO, 7.5% underwent myomectomy, 6.5% underwent TLH, 1.5% underwent LAVH, 8.5% underwent NDVH, 2% underwent vaginal hysterectomy and 1% underwent diagnostic laparoscopy. Myomectomy was performed in young & nulliparous women, to conserve the fertility, the results of myomectomy could not be evaluated as the study duration was short. Vaginal hysterectomy was performed in 2% patients, who had associated uterovaginal prolapse. The specimen size noted and dissected in the center and at the cornual ends, to look for the situation type and number of fibroids.
In our study, the size of the fibroid uterus varied from a few centimetres to 30 weeks of gravid uterus. About 68% were of the size of 16 weeks gravid uterus, 23% were of the size between 16-20 weeks and huge fibroids of > 20 weeks were encountered in 9% of the patients. The heaviest fibroid noted in the study weighed upto 2 kgs. All the leimomyomata were corporeal and no extra uterine fibroid were encountered. Among the fibroids, 93.9% were in the body & 6.1 % were cervical region. The intramural fibroids were the commonest variety comprising about 60.6% of the cases (as shown in Figure 3). The myxoid degeneration (3%) was the most common degeneration seen in our study population followed by hyaline degeneration (2%) and cystic (1%) & calcareous (1%) degenerations.
The histopathological pattern of endometrial were studied. It showed proliferative endometrial in 66.6%, secretary changes in 12%, endometrial hyperplasia in 4.3% cases, cystic glandular hypertrophy in 2.1%, atrophic endometrium in 8.7% cases. The results were inconclusive in 6.5% of the cases either a large intramural fibroid had totally compressed the endometrium or multiple fibroids lead to distortion of endometrium. The associated pathology in the adnexa and other pelvic structures were studied, which showed cystic ovaries in 8% of the cases. A variety of cysts were noted like, simple serous cyst, follicular cyst, serous/papillary cystadenoma, dermoid cyst, corpus luteal cyst. Associated findings were adenomyosis in 16%, chronic cervicitis in 85%, endometriosis in 2% and PID in 4% of the cases.
Discussion
Recent guidelines for fibroid management
Indications for management [10-13]
i. Asymptomatic women with fibroids where the uterine size is less than 16 weeks in size (and where other causes of pelvic mass have been excluded) do not need further investigations but should be advised to seek medical advice if symptoms occur.
ii. Asymptomatic women with fibroids more than 16 weeks should have specialist referral to discuss options including observation.
iii. Quiescent fibroids may be observed.
iv. Removal of fibroids that distort the uterine cavity may be indicated in infertile women, where no other factors have been identified, and in women about to undergo in vitro fertilization treatment.
v. Concern of possible complications related to fibroids in pregnancy is not an indication for myomectomy, except in women who have experienced a previous pregnancy with complication related to these fibroids.
vi. Women who have fibroids detected in pregnancy may require additional fetal surveillance when the placenta is implanted over or in close proximity to a fibroid.
vii. Size, of the fibroids by itself does not warrant removal.
viii. The possibility of sarcomatous degeneration is less than 0.1% and therefore not a justification for intervention.
Management of a patient with a uterine Leiomyoma depends upon her age, parity pregnancy status, complaints desire to have future conception and last but not least the psychological set up of the patient. It was formerly advised that in women approaching menopause active treatment of even symptom producing fibroids should be delayed in the hope that cessation of ovarian function would lead to control of symptoms and eventually to atrophy of tumours. Such hopes are misplaced and should be abandoned in favour of hysterectomy. Following plan of management has been formulated it is not a standardized approach but rather a guideline which must be individualized for each patient.
Medical management of uterine fibroids
Medical therapy is intended to reduce or eliminate the symptoms related to Leiomyoma by decreasing the size of myoma /amount of bleeding. Medical therapy may also be used as an adjacent to surgical therapy as a preoperative measure to control myoma size, pleading or menstrual suppression or more convenient operative schedule [14-17].
a) Gonadotrophin-Releasing hormone agonist therapy induce a pseudo menopausal hypoestrogenic states as a result of desensitization of gonadotrophin receptors in the anterior pituitary gland. This effect appears to be due to down regulation of pituitary GnRH receptors and ultimately decreased LH and FSH.
b) GnRH hormone and Add-Back therapy minimize the adverse effects of prolonged GnRH-agonist therapy due to hypo estrogenic effect. Most add back regimens have used GnRH agonist first to attain uterine shrinkage and amenorrhoea and then added-back estrogens and progestin in either acyclic or a continuous fashion, the sequential method. This add-back uses low dose hormonal replacement.
c) Innovative add-back therapy-Tibolone alleviates climacteric symptoms and prevents osteoporosis without stimulating endometrial proliferation.
d) GnRH antagonists act via classical competitive blockade of the GnRH receptors on gonadotrophic cells and inhibit micro aggregation of these receptors. Thus initial ‘flare up’ phenomenon observed by agonists is absent.
e) Androgen Therapy (Danazol & Gestrinone) effects at different levels of HPO axis as a direct and indirect result of its high affinity binding to intracellular steroid receptors for androgens, progesterone and glucocorticoids. Its primary action is an androgenic effect, increasing serum free testosterone by decreasing serum sex hormone-binding globulin production and by displacing testosterone from sex hormone binding globulin.
f) Antagonists and Receptor blockers [Mifepristone (RU486)] exerts antiprogesterone and antiglucocorticoid activities.
g) Selective estrogens-receptor modulators (SERMs) reduce leiomyoma size in post menopausal women.
Surgical management of uterine fibroids
a) Myomectomy by abdominal, vaginal or laparoscopic approach
b) Hysterectomy by abdominal, vaginal or laparoscopic approach
c) Laparoscopic assisted myomectomy
I. Myolysis: Laparoscopic myolysis results in the coagulation of myoma blood supply and a subsequent reduction in the size of myoma. This can be achieved either by laser or with a long bipolar, needle electrode with a current density of 50-70 watts concerns about postoperative uterine muscle integrity and postoperative adhesion formation has been expressed.
II. Cryomyolysis: In laparoscopic cryomyolysis,43,55 specialized liquid nitrogen laparoscopic probes are used to bring about freezing of select tissues.
III. Uterine artery embolization: Although majority of leiomyomata can be treated with UAE, exceptions include exophytic subserosal fibroids with a stalk of less than 2cms or sub mucosal intracavitary pedunculated fibroids that may detach and lodge in the uterine cavity or abdominal cavity after embolization, Single dominant fibroid larger than 10cm, which are generally associated with procedural failure rates.
IV. Hysteroscopic Myomectomy: The fibroid is removed by use of a resectoscope which uses high frequency electrical energy to cut tissue. This procedure can be done as an outpatient procedure with either local/ general anaesthesia. Most often recommended for sub mucosal fibroids.
V. Radio frequency ablation: This is the newest minimally invasive treatment for fibroids, where fibroid is shrunk using low frequency electrical currents.
VI. High Intensity Focused Ultrasound (HIFU): Ultrasound energy can be focused to create sufficient heat at a focal point so that protein is denaturated and cell death occurs. Concurrent MRI allows precise targeting of tissue and monitoring of therapy by assessing the temperature of the treated tissue [18-30].
The incidence of leiomyoma is highest in the 3rd decade (55%) which is similar to the incidence quoted by Bhashkar Reddy et al. (50%) [31] and Usha et al. (48.97%) [32] indicating that leiomyoma is a disease seen in women of child bearing age, they are rarely found before puberty, and cease to grow after menopause. The incidence of Leiomyoma was highest among the multiparous group as demonstrated by Bhashkar Reddy et al. (46.5%) [31] and Usha et al. (64.20%) [32]. Though the literature states that, leiomyoma is a disease of low parity. This is probably due to early age at marriage, and long gap between the last child birth and development of symptoms (Figure 4-15).
In our study, most of the patients presented with menstrual disturbances (76%). Similar findings of increased menstrual disturbances were observed in the study conducted by Bhashkar Reddy et al., Usha et al. [32], Poddar et al. [33] and Chhabra et al. [34]. Primary infertility due to fibroid has been ascribed to 15-16% of the patients by different authors. Vilos et al. [21] and Khaund et al. [27] have reported an infertility rate of 1-3% associated with fibroids.
About 60% were intramural fibroids, which is the most common variety. Similar results were obtained by other authors like Usha et al. (77%) [32] and Chhabra et al. (47%) [32]. About 15% of the cases had multiple fibroids in our series. Though the incidence of cervical fibroid has been coated as very low 0.6% by Tiltman et al. [35], the incidence our study is comparatively high 6%. The association with cystic ovaries and adenomyosis also indicate hyperestrogenism which was similar to Madhu Udawat et al. (14%) [36].
The histological pattern of endometrium observed was proliferative type in 66.3%. These results are comparable to Chhabra et al. (40%) [32] and Madhu Udawat et al. (68%) [36]. This indicates the hyper estrogenic states associated with fibroids, endometrial was secretory in 12% of the cases. In our study, though the minimally invasive procedures were not used, we considered standard surgical procedures to treat fibroid uterus. The minimally invasive procedures for fibroid uterus have to be considered for the betterment of the patient and the nature course of the disease per se.
Conclusion
Uterine fibroids can cause multiple bleeding and pain symptoms, which might have a negative impact on women’s life, influencing their sexual, social and work life. Despite these consequences uterine fibroid data, especially on epidemiology, symptomatology and their impact on women’s health are still limited and further research is required.
References
- Okolo S (2008) Incidence, aetiology and epidemiology of uterine fibroids. Best Pract Res Clin Obstet Gynaecol 22(4): 571-588.
- Chen CJ, Buck GM, Courey NG (2001) Risk Factors for uterine fibroids among women undergoing tubal sterilization. Am J Epidemiol 153: 20-26.
- Stewart EA (2001) Uterine fibroids. The Lancet 27: 357.
- Walach EE, Vlahos NF (2004) Uterine myomas- An overview of development. Clinical Features and Management Obstet Gynaecol, pp. 393-406.
- Tropeano G, Amoroso S, Scambia G (2008) Non-surgical management of uterine fibroids. Hum Reprod Update 14(3): 259-274.
- Bradley LD (2009) Uterine fibroid embolization; a viable alternative to hysterectomy. Am J Obstet Gynaecol 201L: 127-135.
- Padubidri VG, Shirish N Daftary (2011) Fibromyomas of uterus and uterine polyps [15th edn] In: Hawkins and Bourne Shaw's Textbook of Gynaecology, New Delhi: Elsevier, pp. 352-366.
- Funki K, Fukunishi H, Sawada K (2009) Clinical outcomes of magnetic resonance guided focused ultrasound surgery for uterine myomas 24-month follow-up. Ultrasound Obstet Gynaecol 34(5): 584-589.
- A1 Hilli MM, Stewart EA (2010) Magnetic resonance guided focused ultrasound surgery. Seminar Reproductive Medicine 28(3): 242-249.
- Segars JH, Parrott EC, Nagel JD (2014) Proceedings from the Third National Institutes of Health International Congress on Advances in Uterine Leiomyoma Research: comprehensive review, conference summary and future recommendations. Hum Reprod Update 20(3): 309-333.
- Bulun SE (2013) Uterine fibroids. N Engl J Med 369(14): 1344-1355.
- Cardozo ER, Clark AD, Banks NK, Henne MB, Stegmann BJ, et al. (2012) The estimated annual cost of uterine leiomyomata in the United States. Am J Obstet Gynecol 206(3): 211.e1-e9.
- Donnez J, Dolmans MM (2016) Uterine fibroid management: from the present to the future. Hum Reprod Update 22(6):665-686.
- Hoellen F, Griesinger G, Bohlmann MK (2013) Therapeutic drugs in the treatment of symptomatic uterine fibroids. Expert Opin Pharmacother 14(15): 2079-2085.
- Chabbert-Buffet N, Esber N, Bouchard P (2014) Fibroid growth and medical options for treatment. Fertil Steril 102(3): 630-639.
- Stewart EA (2015) Uterine fibroids. N Engl J Med 372(17): 1646-1655.
- Laughlin-Tommaso SK (2016) Alternatives to hysterectomy: management of uterine fibroids. Obstet Gynecol Clin North Am 43(3): 397-413.
- Chrisman HB, Saker MB, Ryu RK (2000) The impact of Uterine fibroid embolization on resumption of menses and ovarian function. J Vascular Intervention Radiol 11: 699-703.
- Spies JB, Ascher SA, Roth AR, Kim J, Levy EB (2001) Uterine artery embolization for leiomyomata obstet Gynecol 98: 29-34.
- Spies JB, Spector A, Roth AR, Baker CM, Mauro L (2002) Complications after uterine artery embolization for leiomyomas. Obstet Gynecol 100(5): 873-880.
- Vilos GA (2003) Uterine fibroids: relationships to reproduction. Minerva Ginecol 55(5): 417-423.
- Errico Zupi, Alessio Piredda, Daniela Marconi, Duane Townsend, Caterina Exacoustors, et al. (2004) Directed laparoscopic cryomyolysis, A possible alternative to myomectomy and/ or hysterectomy for symptomatic leiomyomas. Am Jr of Obstet & Gynec 190(3): 639-43.
- Valentin Bergamini, Fabio Ghezzi, Antonella Cromi, Bellini, Giovani Zanconata Massimo Franchi (2005) Laparoscopic radiofrequency thermal ablation: A new approach to symptomatic uterine myomas. Am Journal Obstet Gynaec 192(3): 768-773.
- Cura M, Cura A, Bugnone A (2006) Role of magnetic resonance imaging in patient selection for uterine artery embolisation. Acta Radiol 47: 1105-1114.
- Wakler WJ, McDowell SJ (2006) Pregnancy after uterine artery embolization for leiomyomata: a series of 56 completed pregnancies. Am J Obstet Gynecol 195: 1266-1267.
- Pratap Kumar, Narendra Malhotra (2008) Tumours of Corpus uteri Principles of Gynecology (7th edn). In: Jeffcoat's Principles of Gynecology, New Delhi: Jaypee Publications, pp. 487-502.
- Khaund A, Lumsden MA (2008) Impact of fibroids on reproductive Function. Clinical Obstet Gynecol 22(4): 748-760.
- Lesley L Breech, John A Rock (2009) Leiomyomata uteri and myomectomy (10th edn). In: Tetinde's Operative Gynecology, New Delhi: Wolters Kluwer, pp. 687-721.
- Linda D Bradley (2009) Uterine fibroid embolization a viable alternative to hysterectomy. Am Jr of Obstet Gynec, pp. 127-135.
- Moty Pansky, Bryan D Cowan, Maya Frank, Stephen Zimberg, Harriette L Hampton (2009) Laparoscopically assisted Uterine fibroid cryoablation. Am Jr Obstet Gynec 201(6): 571.
- Bhaskar Reddy D (1933) Study of 325 cases of fibromyoma of uterus. Jar Obstetric and Gynaec of India 13: 340.
- Usha, Nurang BR, Tiwari PV, Asthna AK, Gupta RM (1992) Clinicopathological study of benign tumours of the uterus. Indian Medical Gazette, pp. 68-72.
- Poddar II (1957) Fibromyoma of uterus. Indian Jr Obstet Gynaec 8: 109.
- Chabbra S, Neeru Ohri (1993) Leiomyoma of uterus - A clinical study. Journal of Obstetrics and Gynaec of India 33: 438-439.
- Tiltman Andrew J (1998) Leiomyomas of the uterine cervix: A study of frequency. International Journal of Gynaecological Pathology 17(3): 231-234.
- Madhu Udawat (1988) A study of menstrual disturbances in cases of fibroid uterus. Jr Obstet Gynaec of India 367: 10-12.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...