Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-5910
Review Article(ISSN: 2638-5910) 
Nutrition and Pressure Ulcers: An Opportunity to Accelerate the Healing Process Volume 2 - Issue 3
Joanne Chan*
- Accredited Registered Dietitian Sports Specialist Dietitian, Hong Kong
Received:September 04, 2019 Published: September 17, 2019
Corresponding author: Joanne Chan, Accredited Registered Dietitian Sports Specialist Dietitian, Hong Kong
DOI: 10.32474/ADO.2019.02.000138
Abstract
Pressure ulcers, also known as bedsores, are a prevalent and debilitating condition affecting up to 23% of patients in nursing homes or acute hospital settings [1-3]. Inadequate healing of pressure ulcers increases a patient’s susceptibility to life-threatening infections and prolonged hospital stays, leading to increased healthcare expenditure. Therefore, interventions to prevent ulcers or accelerate ulcer healing are essential to improve patient outcomes and reduce the burden of pressure ulcers on healthcare systems.
Introduction
Pressure ulcers are associated with life-threatening complications and high healthcare costs
Pressure ulcers are often caused by a local breakdown of soft tissue as a result of compression between a bony prominence and external surface causing localized tissue damage [3]. An ordinally, older patients, malnourished patients, patients with low mobility and patients with poor sensory perception are at greater risk of pressure ulcers [3,5]. 70-73% of those who develop pressure ulcers are over 6S years old and 25.16% in Hong Kong nursing homes [3]. Typically, pressure ulcers do not heal well, and inadequate healing increases a patient’s susceptibility to life threatening infections, including sepsis and cellulitis [4-6]. Additionally, poor ulcer healing negatively affects the clinical prognosis of comorbid conditions. Mortality rates in patients with pressure ulcers admitted to nursing homes can be as high as 50% after 1 year compared with 27% in patients without pressure ulcers [1]. Therefore, the cost of treating pressure ulcers is high, ranging from £958-£11,606 per patient in the United Kingdom, depending on ulcer severity [7]. Approximately 90% of this cost is a result of increased nursing care, which includes patient monitoring and wound dressing, but antibiotic Costs for treating infections also contribute [7].
Malnutrition is an independent risk factor for pressure ulcers
Malnutrition has been identified as an independent risk factor for both the development of pressure ulcers and delayed healing [8,9]. Additionally, patients with pressure ulcers have high energy expenditure due to the increased nutritional requirements associated with tissue regeneration and an activated immune response [10]. Figures have also been highlighted by Barker et al. [5], approximately 40% of patients in the acute hospital setting are malnourished [5], pin-pointing the need for nutritional assessment upon hospital admission to reduce the risk of complications. The importance of nutrition has been recognized in the National Pressure Ulcer Advisory Panel (NPUAP)/European Pressure Ulcer Advisory Panel (EPUAP)/ Pan Pacific Pressure Injury Alliance (PPPIA), which recommend assessment of nutrition- al status in patients with, or at risk of developing, pressure ulcers. The guidelines. additionally recommend prescription of a high-energy (30-3Skcal/kg body weight/day), high-protein (1.2S-1.5g/kg body weight/day) diet for patients who are malnourished, or at risk of becoming malnourished, that also includes the importance of amino acids such as arginine and micronutrients [11].
A specific high-energy, high-protein, arginine and micronutrient- enriched oral nutritional supplementation enhances pressure ulcer healing
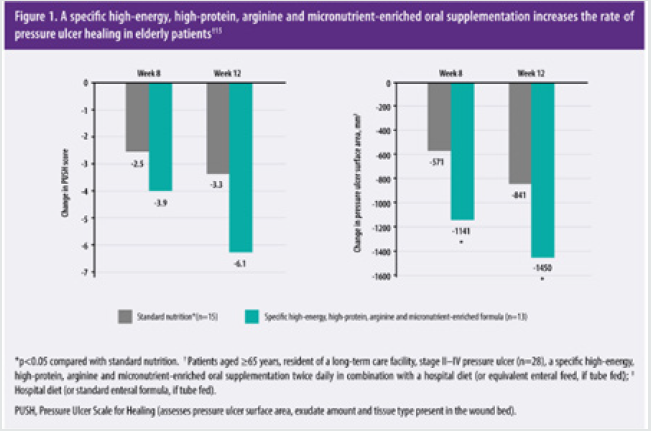
Nutritional support, mostly in the form of high-energy, highprotein oral nutritional supplement can significantly reduce pressure ulcer incidence by 25% in at risk patients compared with standard care [3]. In clinical studies, oral nutrition with specific oral nutritional supplementation enhanced wound healing in patients who were elderly [15] or malnourished [12]. In a 12-week randomized controlled trial, 28 elderly patients with grade II-IV pressure ulcers were randomized to receive a specific high-energy, high-protein, arginine and micronutrient-enriched oral nutritional supplementation twice daily (nutrition formula provided of a total of 500kcaI, 34g protein, 6g arginine, TOOmg vitamin C, and 18mg zinc) in combination with a standard hospital diet (if tube fed, an 1000mL enteral feed with 20% of energy from protein enriched with arginine, zinc and vitamin C [100 kcal, S.S g protein, 0.85 g arginine, 38 mg vitamin C, 2.0mg zinc per 100mL]) or standard nutrition (hospital diet; if tube fed, standard enteral formula comprising 16% of energy from protein without any additional supplement [100kcaI, 4.0g protein, 0g arginine, 10mg vitamin C, 1.2mg zinc per 100mL]). The type and amount of food consumed by each patient was recorded on a clinical register and the mean intake over 3 days standardized to patient weight. Regression analyses were performed to identify the contribution of a specific supplement to any improved outcomes [15]. Results have shown supplementing patients with a high-energy, high-protein, arginine and micronutrient-enriched formula significantly reduced pressure ulcer Scale for healing (PUSH) Score by 85% after 12 weeks (Figure 1; assessment of ulcer surface area, amount of exudate and tissue type), indicating an elevated wound healing with a specific highenergy, high-protein, arginine and micronutrient-enriched oral supplementation. Addition- ally, the specific supplementation was associated with a significant 100% reduction in ulcer surface area after 8 weeks compared with standard nutrition (Figure 1) [15].
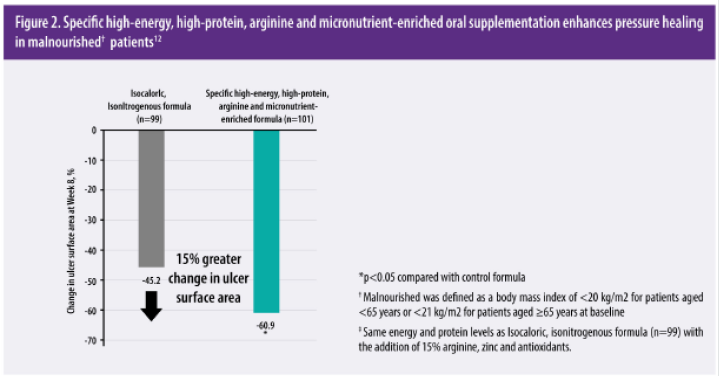
These results have been validated in a large(fi=200), multicenter, randomized controlled trial. The Oligo Element Sore Trial (OEST) reported that the specific oral supplementation significantly enhanced pressure ulcer healing in patients with stage II-lV who were malnourished compared with an isocaloricisonitrogenous formula [12]. Twice-daily supplementation with specific high-energy, high-protein, arginine and micronutrientenriched formula for 8 weeks led to a significantly greater mean reduction in pressure ulcer area (Figure 2) [12].
Management of a sacral pressure ulcer patient by oral supplemented with a specific high protein arginine and micronutrient enriched formula
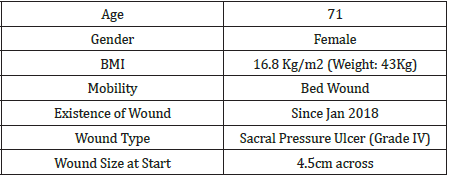
Introduction This
case study describes the management of a patient who developed a sacral pressure sore (Grade IV) during stay in the hospital secondary to hematuria and further care once discharge was followed up in a elderly nursing home setting. Oral Nutritional Supplement was given to promote healing of the wound by Supplementing patient with a high energy, high protein, arginine and micronutrient enriched formula aim promote wound healing.
Treatment regimen
Signs of dead tissue developing within the ulcer with wound on measuring approx 4.5cm across. Ulcer was washed with iodopovidone antiseptic solution and new dressing was applied every day. On 27th Jan 2018 patient was referred to dietitian with past medical history of dementia. Aim was set to promote wound healing and nutritional status as current weight was noted at 43kg and a BMI of 16.8 kg/m2. A high energy, high protein oral nutritional supplementation was recommended twice daily (nutrition formula provided of a total of 500kcal, 34g protein, 6g arginine) in addition to their regular diet and standard wound care and was followed up weekly (Table 1).
Result
After one week the ulcer had reduced significantly in size (3cm) and new flesh and skin was noticed to be developing. Appetite was slowly picking up and supplementation was adjusted to once daily (nutrition formula provided of a total of 250kcal, 17g protein, 3g arginine). Weight was noted staple whilst ulcer continue to heal. By March 2018, the ulcer was almost healed, and patient’s appetite has returned to normal.
Conclusion
Pressure ulcers are a major burden on health resources, with inadequate healing potentially leading to life threatening infections and an increased risk of morality [1,4,5]. Nutritional supplementation with specific high energy, high protein, arginine and micronutrient- enriched oral formula a significantly reduced pressure ulcer incidence and enhanced wound healing in patients who were elderly [15] or malnourished [12] Figure 3.
References
- Smith DM (1995) Pressure Ulcers in the Nursing Home. Ann inter Med 123(6): 433-438.
- Vanderwee K, Clark M, Dealey C, Gunningberg L, Defloor T (2007) Pressure ulcer prevalence in Europe: A pilot study. J Eval Clin Pract 13(6): 227-235.
- Liu KW (2011) The Hong Kong Medical diary. Medical Bulletin September 16(9): 1-40.
- Allman R, Goode PS, Burst N, Bartolucci AA, Thomas DR (1999) Pressure ulcers, hospital complications, and disease severity: impact on hospital costs and length of stay. Adv Wound Care 12(1): 22-30.
- Barker LA, Gout BS, Crowe TC (2011) Hospital malnutrition: Prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health 8(2): 514-527.
- Allaman R (1997) Pressure ulcer prevalence, incidence, risk factors, and impact. Clin Geriatr Med 13(3): 421-436.
- Bennett G, Dealey C, Posnett J (2004) The cost of pressure ulcers in the UK. Age Ageing 33(3): 230-235.
- Stratton RJ, Ek AC, Engfer M, Moore Z, Rigby P, et al. (2005) Enteral nutritional support in prevention and treatment of pressure ulcers: A systematic review and meta-analysis. Ageing Res Rev 4(3): 422-450.
- Banks MD, Bauer J, Graves N, Ash S (2010) Malnutrition and pressure ulcer risk in adults in Australian health care facilities. Nutrition 26(9): 896-901.
- Cereda E, Klersy C, Rondanelli M, Caccialanza R (2011) Energy balance in patients with pressure ulcers: a systematic review and meta-analysis of observational studies.J Am Diet Assoc 111(12): 1868-1876.
- National pressure Ulcer Advisory panel, European Pressure ulcer Advisory panel and Pan pacific Pressure injury Alliance. Prevention and treatment of pressure ulcers: Quick reference guide.
- Cereda E, Klersy C, Serioli M, Crespi A, D Andrea F, et al.(2015) A nutritional formula enriched with arginine, zinc, and antioxidants for the healing of pressure ulcers: a randomized trial. Ann Intern Med 162(3): 167-174.
- Soneja A, Drews M, Malinski T (2005) Role of nitric oxide, nitroxidative and oxidative stress in wound healing. Pharmacol Rep 57: 108-119.
- Molnar J, Underdown MJ, Clark WA (2014) Nutrition and Chronic Wounds. Adv Wound care (New Rochelle) 3(11): 663-681.
- Cereda E, Gini A, Pedrolli C, Vanotti A (2009) Disease-specific, versus standard, nutritional support for the treatment of pressure ulcers in institutionalized older adults: A randomized controlled trial. J Am Geriatr Soc 57(8): 1395-1402.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...