Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-5910
Research Article(ISSN: 2638-5910) 
Multidisciplinary foot Clinic Reduces Diabetic Lower Limb Amputation but Cannot Prevent it Completely: 13 Year Experience at a Vascular Tertiary Centre Volume 2 - Issue 4
J Padee1, UP Ranasinghe2, RS Jayatilake2, M Sullivan3, A Egun1 and S Rajbhandari1*
- 1Department of vascular surgery, UK
- 2Deptartment of Diabetes, Lancashire Teaching Hospital, United Kingdom
- 3Department of Clinical Audit, Lancashire Teaching Hospital, United Kingdom
Received: October 25, 2019 Published: November 12, 2019
Corresponding author:S Rajbhandari, Department of vascular surgery, United Kingdom
DOI: 10.32474/ADO.2019.02.000141
Abstract
Objectives: Assess the effect on lower limb major amputation rate following the introduction of the multi-disciplinary foot clinic in a defined relatively static population in the North West of England.
Methods: Data surrounding all lower limb amputations in diabetic patients between 1997 and 2010 were retrospectively collected and analysed.
Results: Results demonstrated significant increase in minor amputations but numerical reduction in major amputations. There was significant change in ratio of minor to major amputation. When annual fluctuation was averaged out over 5-year period, the annual major amputation per 100,000 patients reduced from 6.6 to 5.1 with increase in minor amputations from 2.0 to 5.9.
Discussion: A reductions in major amputations rate with increase in minor amputations occurred over the 13-year period following implementation of the Multi-Disciplinary Foot Clinic. This suggests that a patient centered and multi-disciplinary approach to the care of these high-risk patients can improve outcomes and lead to limb preservation over time.
Introduction
Foot complications are a major cause of morbidity and mortality
amongst diabetic patients [1]. Amputation is the most feared
diabetic complication [2]. In the UK alone 20 major amputations
are performed every day [3]. Diabetic patients are 36 times more
vulnerable to lower limb amputations than non-diabetics [4]
and foot problems can frequently be limb or life threatening to
the diabetic individual [1] - survival is often bleak, with a 5-year
mortality of approximately 70% [5]. The burden on the economy
is great and although difficult to estimate due to the involvement
of many different specialties contributing at the point of care, some
reports state the direct cost of each diabetic associated amputation
is estimated to be between £15000 - £30000 [6]. Recent Department
of Health data suggests diabetes will affect 4.6million adults in the
UK by the year 2030 [7] so it is important that there is an urgency
to improve outcomes for these patients.
Amputations can be a clearly defined endpoint [8] in assessing
the effectiveness of prevention and treatment of diabetic foot both
regionally and nationally. Approximately 80% of amputations are
preventable and despite this, in 2007/2008 nearly a quarter (23%)
of diabetics did not have a foot check [9]. The 2010 Department
of Health recommendations suggested establishing integrated
multi-disciplinary diabetic specialist teams in an effort to improve
amputation rates nationally. Most diabetic patients will likely
present with symptoms suggestive of complications prior to
eventual amputation, and this suggest that a programme for active
prevention and optimal treatment of diabetic foot complications
may decrease the risk of amputation [2]. This has been suggested
following a case control study in Germany which was performed
to quantify the relationship between amputation and diabetes. The
results of the study concluded that there is a strong association between amputation and diabetes and through better foot care it
is possible to reduce the number of lower limb amputations [10].
Background
In 2001 a Diabetic Multi-Disciplinary Foot Clinic was started in Lancashire Teaching Hospitals NHS Trust. This clinic was set up to manage diabetic patients referred from the community team. The Clinic would be led by a Consultant Diabetologist and attended by a podiatrist in close liaison with the community podiatrist, and occasionally the Consultant Orthopaedic Foot Surgeon. The orthotics department and the plaster room were made easily accessible to manage the ‘Charcot joint’ patients appropriately. Clinic review would involve review of the patients’ diabetic control, and a thorough assessment of the feet including sensory examination and pedal pulse assessment. Simultaneously, a Diabetic Multi-Disciplinary Team (MDT) was created and highrisk patients discussed monthly at a lunchtime meeting at Royal Preston Hospital. This team consisted of a Consultant Vascular Surgeon, Consultant Diabetologist, Consultant microbiologist, Orthotist, community and hospital podiatrist and Specialist Nurses (including Tissue Viability, Vascular and Diabetic Nurses) with access to Consultant Orthopaedic Surgeon, musculoskeletal radiologist, vascular interventional radiologist and Post - Amputation Rehabilitation Consultant as needed. The main objective of this MDT delivered approach was to improve foot care of diabetic patients and through improved patient education and early recognition of diabetic complications, reduce the number of major amputations performed. The aim of this study was to assess whether the implementation of this MDFC and MDT approach had improved the outcomes for diabetic patients in the Lancashire area.
Research Design and Methodology
The study evaluated the number of people who have undergone diabetic associated lower limb amputations from 1997 – 2010 in a mixed rural/urban population served by Lancashire Teaching Hospitals NHS Foundation Trust. Over the study period the defined ‘diabetic population’ increased and it is important to note that in 2005 the Quality & Outcome Framework was introduced whereby practitioners are given financial incentives to achieve outlined diabetes targets. Following this, the number of diabetics almost doubled without any significant increase in population. Amputations were divided into major (defined as above ankle) and minor (defined as below ankle). It was decided that patients who had both major and minor amputations were categorized only under majors. Amputations of the lower limb due to trauma or tumor related disease was excluded. The project was registered with the audit and coding department. The raw data was retrospectively collected by members of the diabetic medical team from hospital activity data from 1997 to 2010 using the coding data obtained from the Trust coding department. As yearly amputation rate fluctuated, data of initial five years (1997 to 2001) were averaged out as early group and compared with that of last five years (2006 to 2010) as late group. The incidence of amputation was therefore expressed as per 100,000 general populations with census data from 2001 & 2011 [11].
Results
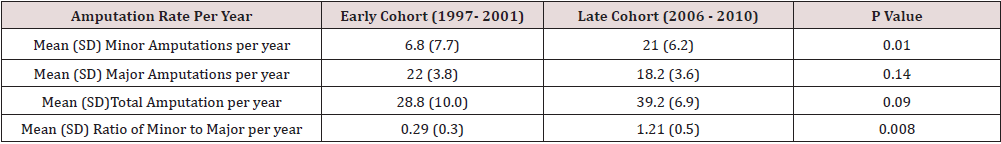
Between 1997 and 2010, we were able to identify a total of 498 lower limb amputations in diabetic patients were performed. Of these 498 amputations, 282 were major amputations Table 1. Results in Table 1 demonstrated a clear reduction in the proportion of major to minor amputation over this study period. The ratio of minor to major amputation rose from 0% in 1997 to 192% in 2010. The number of minor amputations and total amputation rose but the number of major amputations reduced. The effect of introduction of foot clinic in 2001 was clear in this trend Figure 1. When the early group (1997 to 2001) was compared to late group (2006 to 2010) there was significant increase in minor amputations, but no change in major or total amputations. There was significant increase in ratio of minor to major amputations Table 2. The number of newly diagnosed diabetes increased significantly around 2003 in the UK as general practitioners were given incentives to identify undiagnosed diabetes. As a result, amputation rate per 1000 diabetes population would not give correct picture. Therefore, we analysed amputation rate per 100,000 population. The population of area covered by Lancashire Teaching Hospital increased from 333,900 to 356500 between 2001 to 2011. The major annual amputation rate per 100,000 people reduced from 6.6 to 5.1 but minor amputation rate rose from 2.0 to 5.9 between the early and late groups.
Figure 1: Incidences of major, minor and total amputation per 100,000 general populations. The black arrow indicates the introduction of the MDFC at Lancashire Teaching Hospitals NHS Foundation Trust.
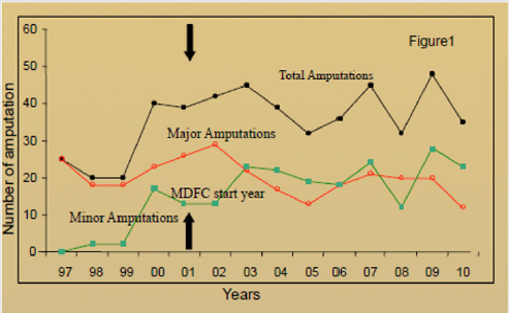
Table 1: Minor and major amputation rates and Minor: Major amputation ratio 1991-2010. Figures in () represent proportion of amputations that year distributed between major and minor amputations.
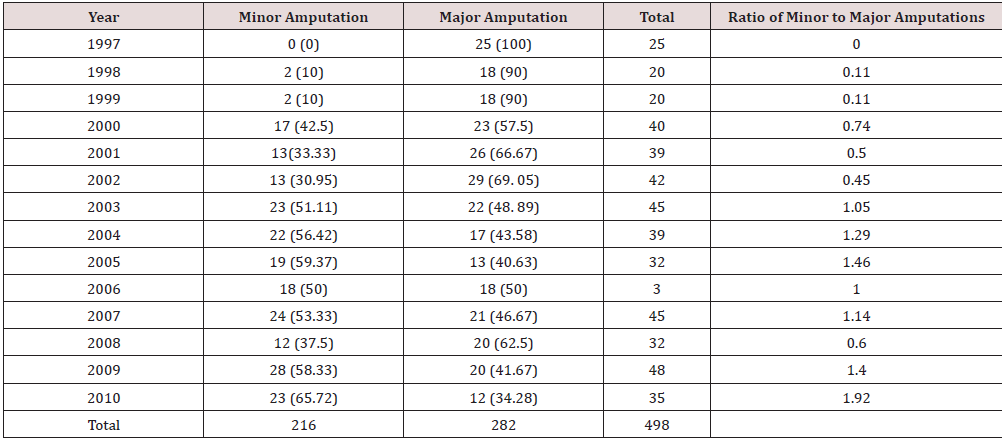
Table 2: Mean annual amputation rate (standard deviation) per year in ‘Early’ (1997–2001) and ‘Late’ (2006–2010) cohorts showing significant rise in minor amputations.
Discussion
The development of the multi-disciplinary foot clinic has
demonstrated that the multidisciplinary approach to diabetic
patients can lead to earlier and better recognition of diabetic foot
complications. This can lead to prompt and effective referral to
the appropriate specialist for swift management. Management of
diabetic lower limb complications varies nationally [12] depending
on vascular experience, variability in regional protocols and we
are hopeful that this approach will encourage a consensus on the
management of these complex patients within the Lancashire
Vascular Tertiary Referral Centre. The multi-disciplinary approach
may have led to change in attitudes around the detection and
management of diabetic lower limb complications. The increase
in number of diabetic patients following QOF introduction in 2003
without any significant increase in population slightly affected the
way we expressed our data. In order to be more representative,
we favored the incidence of amputation being expressed as
per 100,000 general populations, in order to avoid bias change
based on increasing in diabetes prevalence. Despite the observed
increasing diabetic population, the proportion of them requiring
major amputation is decreasing which is reassuring that our
approach is having the desired effect. We noticed increase in minor
amputations. This is because same patient could have 5 minor
amputations before undergoing major amputation of a leg. Each
minor amputation would have prevented one major amputation.
However major amputations can be delayed but not totally
prevented in many cases as seen by surge in major amputation after
few years gap.
Researchers reporting in a study performed in Ipswich Hospital
in 2008 found very similar results following the introduction of a
multi-disciplinary foot team [2]. This suggests that, irrespective of
location, population and other associated risk factors they might
harbour, a team-based approach to the care of these high risk
patients can result in dramatic improvements in long term limb
preservation. The study does have several limitations. The study
was performed retrospectively which can mean that the data is less
accurate as it relies on coded data which may have been entered
incorrectly. The management of diabetic lower limb complications
is also affected by the variability in individual surgeon practice.
Some surgeons are very aggressive in their limb preservation while
others are more pragmatic, and this will affect the outcome.
Conclusion
These findings support the suggestion that a multi-disciplinary approach to these high-risk patients plays an important role in the reduction of lower limb major amputation rates. Over the study period there have been improvements in the vascular, radiological and microbiological management of patients. These disciplines have improved their ability to communicate and work as a multidisciplinary team which will have improved the management of diabetic related complications. Early detection of such complications may allow limb preservation or limb-length preservation over time and we have clearly demonstrated significant improvement in outcomes for one of the most feared and most costly complications for diabetic patients. Improvement in foot care through a multidisciplinary approach and continuous assessment of practice can only ensure long term outcomes will mirror those found in this 13- year study period.
References
- NK Chammas,RLR Hill, MEEdmonds (2016) Increased Mortality in Diabetic Foot Ulcer Patients: The Significance of Ulcer Type. Journal of Diabetes Research 2016: 1-7.
- Krishnan S, Nash F, Baker N, Fowler D, Rayman G (2008) Reduction in Diabetic Amputations Over 11 years in a defined UK population. Diabetes Care31(1): 99-101.
- Diabetes UK.
- Rayman G, Krishnan S, Baker N, Wareham A, Rayman A (2004) Are we under-estimating Diabetes-Related Lower-Extremity Amputation Rates? Diabetes Care 27(8): 1892-1896.
- NICE Guideline.
- Amputation linked to diabetes.
- NICE Guideline (2017) Type 2 diabetes: prevention in people at high risk.
- Winell K, Niemi M, Lepantalo M (2006) The National Hospital Discharge Register Date on Lower limb amputations. Eur J Endovasc Surg32(1): 66-70.
- (2010) NHS Atlas of Variation. Endocrine, Nutritional and Metabolic Problems. Department of health, USA.
- Trautner C, Haastert B, Giani G, Berger M (2002) Amputations and diabetes: A case-control study, University of Bielefeld, School of Public Health, Bielefeld, Germany. Diabet Med19(1):35-40.
- (2011) Lancashire's population.
- Holman N, Young RJ, Jeffcoate WJ (2012) Variation in the recorded incidence of amputation of the lower limb in England. Diabetologia55(7): 1919-1925.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...