Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-5910
Short Communication(ISSN: 2638-5910) 
Diabetes in Older People: Comprehensive Approach Volume 3 - Issue 2
Óscar Moreno-Pérez1*, Cristina Tejera2 and Rebeca Reyes-García3
- 1Endocrinology and Nutrition department, Alicante General University Hospital - Alicante Institute of Health and Biomedical Research (ISABIAL), Alicante, Clinical Medicine department, Miguel Hernández University, Elche, Spain
- 2Endocrinology and Nutrition department, Complejo Hospitalario Universitario de Ferrol, Spain
- 3Endocrinology and Nutrition department, Torrecárdenas University Hospital, Almería, Spain
Received: November 04, 2020 Published: October 13, 2020
Corresponding author: Óscar Moreno-Pérez, Endocrinology and Nutrition department, Alicante General University Hospital - Alicante Institute of Health and Biomedical Research (ISABIAL), Alicante, Clinical Medicine department, Miguel Hernández University, Elche, Spain
DOI: 10.32474/ADO.2020.03.000157
Abstract
The clinical management of older people with diabetes requires a comprehensive evaluation and a holistic approach for the
individualization of objectives and strategies of treatment. In older people with diabetes, geriatric syndromes, frailty and sarcopenia
are considered at present as a third category of chronic complications. These situations are added to traditional microvascular
and macrovascular complications, leading to significant disability and increasing the costs. In this context, two clinical scenarios
can be considered: the first one, elderly subjects without significant comorbidities and good functional condition, in which an
approach to diabetes similar to that of younger patients must be made. The second scenario, elderly and frail subjects, in which it
will be essential a correct identification of these conditions and the evaluation of geriatric syndromes. This evaluation will guide the
adaptation in the goals of treatment and in global management of diabetes.
Some basic principles should guide our decision-making: starting drugs at low - medium doses, with progressive increase
according to tolerability; selection of drugs according to evidence-based medicine (considering the limited evidence in this age
group), favoring agents with the lowest risk of hypoglycemia, avoid polypharmacy. Finally, patient´s safety and quality of life should
be the main objectives.
Keywords: Diabetes; Older; Frailty; Evidence-Based-Medicine
Opinion
Clinical management of older diabetes people requires
a comprehensive evaluation and a holistic approach for the
individualization of objectives and strategies of treatment. Geriatric
syndromes, frailty and sarcopenia are considered at present as a
third category of chronic complications [1]. These situations
are added to traditional microvascular and macrovascular
complications, leading to significant disability and a significant
increase in costs.
In this context, two clinical scenarios can be considered: first,
elderly subjects without significant comorbidities and without
frailty, in which an approach to diabetes similar to that of younger
patients must be made. The second scenario, elderly and frail
subjects, in which a correct identification of frailty and an evaluation
of geriatric syndromes is mandatory, guiding modifications in the
goals of treatment and in the global management of diabetes.
Initial Approach
1. Consider evaluation of medical, functional (self-care
skills) and geriatric sphere to establish a frame of reference that
determines the objectives and therapeutic strategies diabetes
management (Evidence B) [2].
2. Assess presence of geriatric syndromes (polypharmacy,
cognitive impairment, depression, urinary incontinence,
falls, chronic pain) as conditions that interfere with patient’s
management of diabetes and reduce quality of life (Evidence B)
[2].
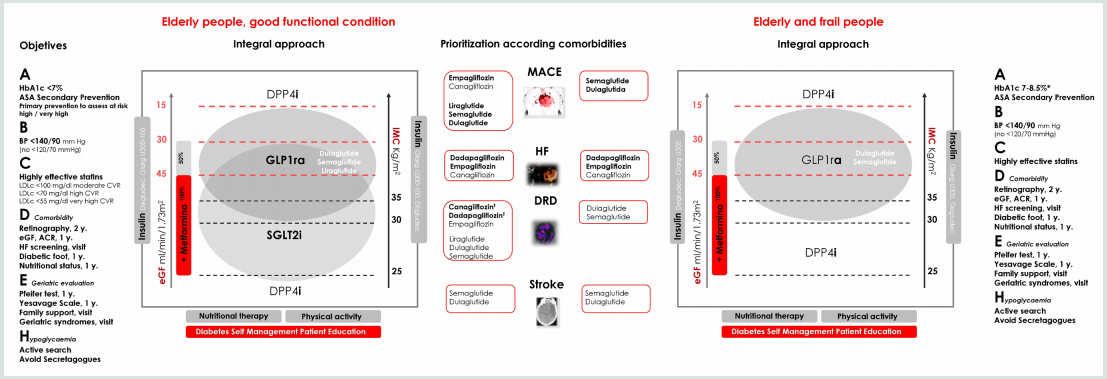
Figure 1: Comprehensive approach in older people with T2DM.
Bold therapy: grade A evidence. * Clinical situation: Intermediate / complex HbA1c 7-8%, TA <140/90 mmHg; very complex HbA1c <8.5%, TA <150/90 mm Hg.
ASA, acetylsalicylic acid; BP, blood pressure; LDLc, LDL cholesterol; y., every “number” years; eGF, estimated glomerular filtration; ACR, urine albumin creatinine
ratio; HF, heart failure (evidence limited to patients at risk of heart failure or patients with FH diagnosis and reduced ejection fraction); Ŧ eGFR <30 mL/min/1.73 m2:
Initiation not recommended, but once established, it can be maintained until the start of dialysis.
GLP1ra, glucagon-like peptide-1 receptor agonists; SGLT2i, sodium-glucose transport protein 2 inhibitors; DPP4i, dipeptidyl peptidase 4 inhibitors; Glarg, glargine
3. Evaluation of frailty. The most validated and simple
evaluation tools are Fried criteria and FRAIL scale. Consider
potentially reversible causes that contribute to frailty such as
presence of hypothyroidism, vitamin D deficiency, anemia, etc.,
is advised [3].
4. In those over 65 years of age, an early diagnosis of
mild cognitive alterations is recommended, at diagnosis and
subsequently annually [2]. Pfeiffer questionnaire or Minimental
test are validated tools. In patients with cognitive dysfunction,
simplify treatment, and adapt care structure.
5. Patient safety, preferences and quality of life should be the
main objectives.
Treatment objectives, therapeutic approach and the assessment
of comorbidities, are shown in (Figure 1).
Treatment Objectives (ABCDEH):
A. Glycemic control (A1c)
General recommendation, which should always be individualized, is a target of HbA1c 7.5-8.5% (58-69 mmol/l) in advanced frailty, and HbA1c 7-8% (53-64 mmol/l) in mild to moderate frailty. In frailty subjects, HbA1c <7% (53 mmol/l) should be avoided, especially if drugs with risk of hypoglycemia are used [2]. Many frail subjects have medical conditions that can interfere with HbA1c determination (chronic kidney disease, anemia, transfusions), and capillary blood glucose measurement may be necessary for assessing glycemic control [2].
B. Blood pressure (BP)
The objective of elderly subjects with diabetes, including those with dementia, is <140/90 mmHg, avoiding values <120/70 mmHg. A goal of <150/90 mmHg may be more suitable for the frail and dependent elderly. Whenever possible, measure BP standing and sitting, to detect orthostatic hypotension that increase the risk of falls. Withdrawal of treatments should be evaluated as frailty progresses [2,3].
C. Hypercholesterolemia
Statin treatment is recommended in the same situations as in non-elderly subjects: secondary prevention and primary prevention with high cardiovascular risk. Treatment of hypercholesterolemia in elderly patients has some differential characteristics. Lifestyle changes may not be possible. Furthermore, statin myopathy is more frequent (up to 10%) due to sarcopenia, so it is advisable to use low or moderate doses of statins. Treatment of vitamin D deficiency can improve statin-associated myalgia [3]. In situations of advanced frailty and dependency, suspension of statins may be considered.
D. Assessment of chronic complications
It must be individualized, with particular attention to those with higher influence on functional state (retinopathy, diabetic macular edema and diabetic foot). Heart failure, chronic kidney disease, and vitamin B12 deficiency should not be forgotten [2,4].
E. Geriatric Evaluation
Consider the assessment of geriatric syndromes: polypharmacy (use of three or five drugs simultaneously or the need to indicate one drug to supply the side effects of another), cognitive impairment, depression (Yesavage scale annually), urinary incontinence, falls, chronic pain (visual analogue pain scale), and frailty [2,3].
F. Hypoglycemia
In older people prevention of hypoglycemia is especially important because of the repercussions on the risk of falls, fractures, and emergency department visits and hospitalization. Elderly patients have impaired recognition of hypoglycemia and difficulties in acquiring basic skills for self-care and for resolution of hypoglycemia, which determines a greater severity of the episodes. Also, there is a bi-directional relationship between hypoglycemia and cognitive decline [5].
Comprehensive Pharmacological Treatment in the Elderly with T2DM
In general terms, disease modifying therapies should be used
in combination with metformin, that is, with benefit in morbidity
- associated mortality, low risk of hypoglycemia, and benefits in
terms of control of BP and excess of weight (if appropriate) [6].
The patient and their caregivers should be aware of the “sick
days” rule for metformin and sodium-glucose transport protein
2 inhibitors (SGLT2i), to avoid the potential risk of impaired
renal function, lactic acidosis, and euglycemic ketoacidosis. Also,
simplification of complex regimens is recommended, especially in
patients with insulin therapy, to reduce the risk of hypoglycemia
and polypharmacy, always based on individualized HbA1c targets.
The use of SGLT2i in frail elderly patients with a diagnosis
of heart failure (HF) with reduced ejection fraction (FEr), is a
reasonable therapeutic option, given its potential benefits. Diuretic
and blood pressure treatment must be revised to avoid volume
depletion (hypotension, orthostatic hypotension, dizziness,
syncope, and dehydration), and impaired kidney function.
DPP4 inhibitors (DPP4i) may be reserved for elderly people
with renal function contraindicating other therapies, or those
patients with normal weight, in whom the additional weight loss
may be a problem; in this case, sitagliptin [7]. and linagliptin [8]
must be prioritized. Sulfonylureas and glinides (hypoglycemia
risk), and pioglitazone (risk of heart failure and fractures), must be
avoided.
In frail elderly people with obesity, the use of weekly glucagonlike
peptide-1 receptor agonists (GLP1ra) may be a good option given the low risk of hypoglycemia, the weight loss benefit, the
potential benefits in comorbidities and the weekly administration
[9]. Its use must be accompanied by adapted nutritional therapy,
and appropriate physical activity recommendations (aerobic and
resistance training) to avoid the loss of muscle mass, including
strength, flexibility and balance exercises [10]. Also, the appearance
of gastrointestinal effects should be monitored.
Opinion
- Wong E, Backholer K, Gearon E, Harding J, Freak-Poli R, et al. (2013) Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 1(2): 106-114.
- American Diabetes Association (2020) 12. Older Adults: Standards of Medical Care in Diabetes-2020. Diabetes Care 43(Supplement 1): S152-S162.
- Alan Sinclair, Alison Gallagher (2019) Managing frailty and associated comorbidities in older adults with diabetes: Position Statement on behalf of the Association of British Clinical Diabetologists (ABCD) | ABCD (Diabetes Care) Pp: 1-17.
- American Diabetes Association (2020) 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Medical Care in Diabetes-2020. Diabetes Care 43(Supplement 1): S37-S47.
- Sheen Y-J, Sheu WHH (2016) Association between hypoglycemia and dementia in patients with type 2 diabetes. Diabetes Res Clin Pract 116: 279-287.
- Reyes-García R, Moreno-Pérez Ó, Tejera-Pérez C, Fernández-García D, Bellido-Castañeda V, et al. (2019) Document on a comprehensive approach to type 2 diabetes mellitus. Endocrinol Diabetes Nutr 66: 443-458.
- Bethel MA, Engel SS, Green JB, Huang Z, Josse RG, et al. (2017) Assessing the Safety of Sitagliptin in Older Participants in the Trial Evaluating Cardiovascular Outcomes with Sitagliptin (TECOS). Diabetes Care 40(4): 494-501.
- McGuire DK, Alexander JH, Johansen OE, Perkovic V, Rosenstock J, et al. (2019) Linagliptin Effects on Heart Failure and Related Outcomes in Individuals with Type 2 Diabetes Mellitus at High Cardiovascular and Renal Risk in CARMELINA. Circulation 139(3): 351-61.
- Valencia WM, Florez HJ, Palacio AM (2019) Suitable Use of Injectable Agents to Overcome Hypoglycemia Risk, Barriers, and Clinical Inertia in Community-Dwelling Older Adults with Type 2 Diabetes Mellitus. Drugs Aging 36(12):1083-1096.
- Deutz NEP, Bauer JM, Barazzoni R, Biolo G, Boirie Y, et al. (2014) Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr 33(6): 929-936.
References
- Wong E, Backholer K, Gearon E, Harding J, Freak-Poli R, et al. (2013) Diabetes and risk of physical disability in adults: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 1(2): 106-114.
- American Diabetes Association (2020) 12. Older Adults: Standards of Medical Care in Diabetes-2020. Diabetes Care 43(Supplement 1): S152-S162.
- Alan Sinclair, Alison Gallagher (2019) Managing frailty and associated comorbidities in older adults with diabetes: Position Statement on behalf of the Association of British Clinical Diabetologists (ABCD) | ABCD (Diabetes Care) Pp: 1-17.
- American Diabetes Association (2020) 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Medical Care in Diabetes-2020. Diabetes Care 43(Supplement 1): S37-S47.
- Sheen Y-J, Sheu WHH (2016) Association between hypoglycemia and dementia in patients with type 2 diabetes. Diabetes Res Clin Pract 116: 279-287.
- Reyes-García R, Moreno-Pérez Ó, Tejera-Pérez C, Fernández-García D, Bellido-Castañeda V, et al. (2019) Document on a comprehensive approach to type 2 diabetes mellitus. Endocrinol Diabetes Nutr 66: 443-458.
- Bethel MA, Engel SS, Green JB, Huang Z, Josse RG, et al. (2017) Assessing the Safety of Sitagliptin in Older Participants in the Trial Evaluating Cardiovascular Outcomes with Sitagliptin (TECOS). Diabetes Care 40(4): 494-501.
- McGuire DK, Alexander JH, Johansen OE, Perkovic V, Rosenstock J, et al. (2019) Linagliptin Effects on Heart Failure and Related Outcomes in Individuals with Type 2 Diabetes Mellitus at High Cardiovascular and Renal Risk in CARMELINA. Circulation 139(3): 351-61.
- Valencia WM, Florez HJ, Palacio AM (2019) Suitable Use of Injectable Agents to Overcome Hypoglycemia Risk, Barriers, and Clinical Inertia in Community-Dwelling Older Adults with Type 2 Diabetes Mellitus. Drugs Aging 36(12):1083-1096.
- Deutz NEP, Bauer JM, Barazzoni R, Biolo G, Boirie Y, et al. (2014) Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr 33(6): 929-936.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...