Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-5910
Research Article(ISSN: 2638-5910) 
A Review of Diabetic Admissions in a Tertiary Hospital in Sierra Leone Volume 4 - Issue 3
Joshua Coker1,2*, Gibrilla Fadlu Deen1,2, Onome Abiri2,3, Antonius Gbow1, Alhaji Gbla1 and James Russell1,2
- 1Connaught Hospital, University of Sierra Leone Teaching Hospitals Complex, Sierra Leone
- 2University of Sierra Leone, Sierra Leone
- 3Pharmacy Board of Sierra Leone, Sierra Leone
Received: September 19, 2022 Published: November 16, 2022
Corresponding author: Joshua Coker, Connaught Hospital, University of Sierra Leone Teaching Hospitals Complex, Sierra Leone
DOI: 10.32474/ADO.2022.04.000186
Abstract
Background: The burden of diabetes mellitus is on the rise posing significant threats on health systems, health expenditures and the livelihood of affected patients. In sierra Leone, there has been no data on diabetic admissions. This study intends to close this gap in knowledge and give preliminary data on the profile of patients admitted with diabetes mellitus.
Methods: This is a retrospective review of 250 case notes of patients admitted into medical wards or intensive care unit with diabetes mellitus over a 6-month period.
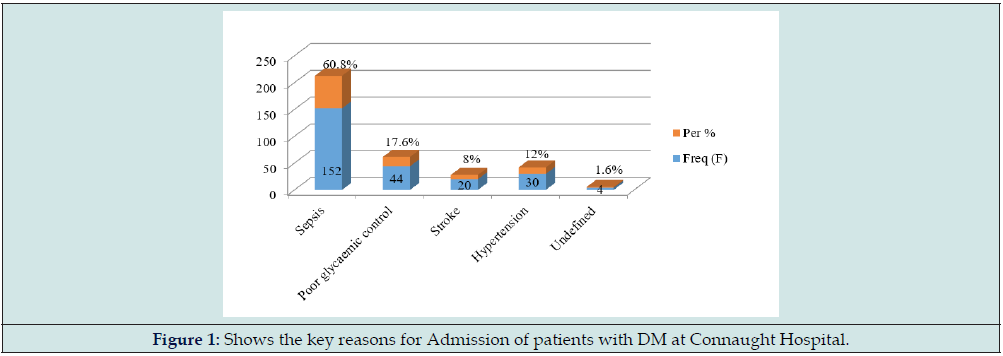
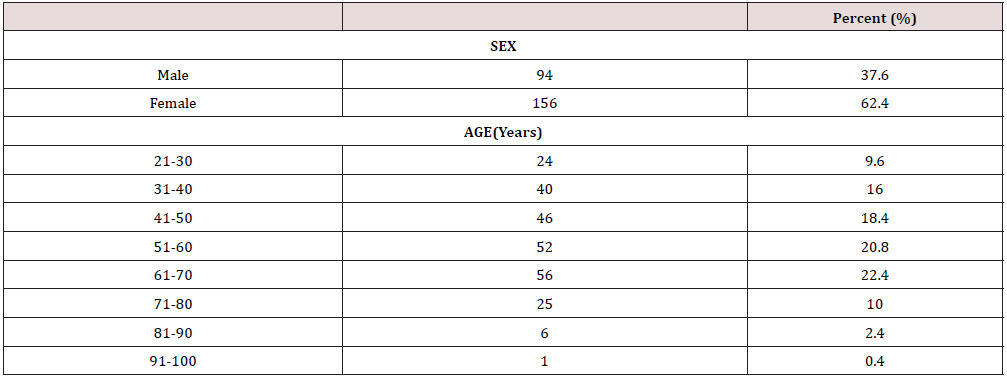
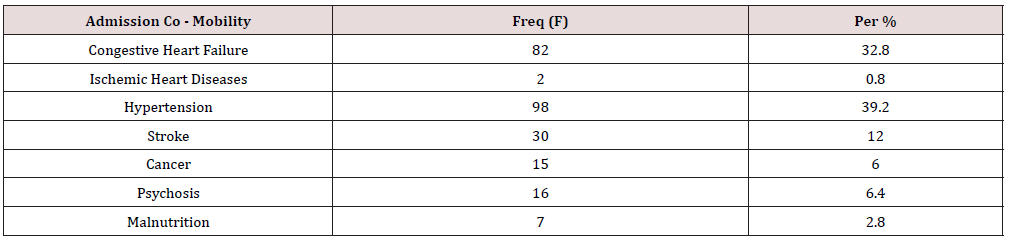
Results: We estimated an admission burden of 20.1% during the study period; patients were mainly females (62.4%) with type 2 diabetes mellitus. The commonest reasons for admissions were sepsis (60.8%) and hyperglycaemia or poor glycaemic control (17.6%). The commonest comorbidities were systemic hypertension (39.2%) and heart failure (32.8%); 17.2% of admissions were due to acute complications of diabetes mellitus.
Conclusion: There is a significant admission burden of diabetes mellitus, mainly in females with type 2 diabetes mellitus. The main reasons for admission were sepsis and poor glycaemic control.
Introduction
Diabetes mellitus poses a significant burden on health services worldwide [1]. It is a major public health threat with negative outcomes for individuals, communities, and health systems[2]. Diabetes mellitus accounts for an increase in all-cause mortality by 2-3 fold [3]. This may be related to increased mortality from infections, cardiovascular disease, stroke, chronic kidney disease, chronic liver disease, and cancer [4,5]. Over approximately 27 years, the global burden of disease estimated a 102.9% increase in incidence, 129.7% increase in prevalence, 125.5% increase in deaths and a 116.7% increase in disability-adjusted life years attributable to diabetes mellitus [6]. The number of patients with diabetes mellitus is estimated to increase to 693 million by 2045 [7]. In sub Saharan Africa, an estimated 19.8 million adults are living with diabetes mellitus, with Nigeria having 3.9million cases [8]. In Sierra Leone, the prevalence of diabetes mellitus was estimated at 2.4 % in an urban population and 0% in a rural population [9]. The authors attributed this to the adverse effects of a western diet and lifestyle.
This article aims to describe the profile of patients admitted with diabetes mellitus into the medical wards of Connaught Hospital in terms of key reasons for admission, underlying co morbidities and pattern of complications. Due to the lack of published data on DM admissions in our environment, this study will close this gap in knowledge, identify predictors of admissions as well as estimate the burden of hospital admissions. The findings from this study may sensitize the appropriate authorities to intervene and remind the diabetics on the need to participate in an integrated community directed efforts to practice the culture of early reporting in order to avert the impacts of complications to the barest minimum.
Methods
Study Setting
This study was conducted at Connaught Hospital, University of Sierra Leone Teaching Hospitals Complex, located in Freetown, (Sierra Leone). It is a tertiary hospital and also serves as the main referral hospital for medical and surgical cases in the country with a bed capacity of 312.
Study Design, Study Population and Sample Size
This is a retrospective review of case notes of patients admitted into medical wards or intensive care unit with diabetes mellitus over a 6-month period (March – August 2021) who met the inclusion or exclusion criteria. A total of 250 patients were admitted with diabetes mellitus during the study period.
Inclusion and Exclusion Criteria
All patients admitted with diabetes mellitus during the study period. Patients admitted for other illnesses other than diabetes mellitus.
Data Collection
This was done using a well-structured cross-sectional study proforma. Details obtained from the proforma included demographic data, history of DM, reasons for admission, blood pressure at admission, random blood glucose at admission, presence of co-morbidity, Complications(acute and chronic) at presentation. Patients were included as diabetics if they are already on an antidiabetic drug or previously diagnosed with diabetes mellitus or admitted with a random blood glucose ≥11.1 mmol/l (with associated symptoms).
Data Presentation
The collected data was entered into Microsoft excel software and analyzed using Statistical Package for Social Sciences (SPSS) software version 26 and results were presented in the form of tables and figures. Quantitative variables were summarized using mean and standard deviation.
Results
A total of 250 patients were admitted with diabetes mellitus at the medical wards of Connaught Hospital during the study period. The total number of medical admissions during this period was 1209 patients. This gives an admission burden of 20.1%. The study suggests that 90.4% of the participants presented with type 2 diabetes mellitus. 32.8% of the patients were either obese or overweight. The majority of admissions with Diabetes mellitus (82.8%) were due to non- diabetes related causes; 17.2% of admissions were related to acute or chronic complications of Diabetes mellitus. The acute complications were represented as follows: hyperglycaemic hyperosmolar state (50%); diabetic ketoacidosis (31.8%); lactic acidosis (4.6%) and hypoglycaemia (13.6%). The occurrence of chronic complications of diabetes mellitus were distributed as follows: stroke (28.1%); diabetic eye disease (23.1%); diabetic nephropathy (20.2%);diabetic foot, ischaemic heart disease and diabetic neuropathy were each represented as 9.5% (Tables 1 & 2) (Figure 1).
Discussion
The summary of findings from this study revealed a 20.1% admission burden attributable to diabetes mellitus. Majority of these patients were middle- aged females and were empirically classified as type 2 diabetes mellitus. A significant proportion of these patients were overweight or obese. The key reasons for admissions were sepsis and poor glycaemic control. The commonest comorbidity in patients with diabetes mellitus is systemic hypertension. The admission burden accounted for by diabetes mellitus in this study is significant. This might suggest a rising occult prevalence of the disease which might be due to overt change in our diet and lifestyle over the last 2-3 decades [10]. If unchecked, this rise will lead to untold morbidity and mortality of our popoulation as health facilities may be easily overwhelmed. The female preponderance in this study may be explained by factors such as sedentary lifestyle and obesity which are common in this gender as they approach middle-age. Another study also documented similar findings of 27.8% admission burden of diabetes mellitus, mainly females with type 2 diabetes [11]. In another study, the burden of admission was stated as 40.6% [12]. Studies done in our sub region revealed approximately 10% admission burden attributable to diabetes mellitus [13,14].
Many of our patients were empirically classified as type 2 diabetes mellitus based on clinical features such as age, body mass index and response to oral antidiabetics. Objectively, these patients should have their C-peptide levels checked or be screened for antibodies against insulin or islet cells. Unfortunately, these facilities are not readily available in the country. Despite this limitations, studies done elsewhere also demonstrated a type 2 diabetes predominance of >90% among admitted patients [15,16]. The commonest reasons for admission of patients with diabetes mellitus were sepsis and poor glycaemic control. The rising burden of antimicrobial resistance in our setting further compounds the treatment of infections in diabetics and such infections are usually severe. The lack of enhanced microbiological laboratory facilities in the country also aggravates the problem. Many of our patients are not compliant with their prescribed medications, making glycaemic control a serious problem in our environment. Issues relating to affordability and alternative medicine may be contributory. Diabetes mellitus potentiates the occurrence of cardiovascular events and infections, and this has been attributed to poorly controlled hyperglycaemia, increased prevalence of cardiovascular risk factors, decreased immunity and chronic complications of diabetes mellitus [17,18]. The reasons stated for admission of diabetics included acute coronary syndrome, heart failure, pneumonia, chronic obstructive pulmonary disease and stroke [12]. In another study, hyperglycaemic emergencies were the commonest reason for admission [13]. The most common comorbidity is systemic hypertension. Both conditions are related to damage to the vascular endothelium. A study done in Canada also supported this fact [19].
Studies have shown that the burden of hospital admissions attibutable to diabetes mellitus can be reduced by early diagnosis, public education, yearly screening for complications and vaccination against common infections [20-23]. The need for public sensitization, prevention programmes and achieving glycaemic treatment targets were also emphasized in another study done in Sierra Leone [10].
Recommendation -In addition to the above, there is need for enhanced manpower development, availability of facilities needed to manage diabetes mellitus and its complications and availability of specialized drugs needed to treat diabetes mellitus.
Limitations of the Study
The study was a single center study and findings may not reflect that from other hospitals. Due to the retrospective nature of the study, some data may be missing. The study was done in the medical wards without data from surgical wards. The lack of facilities to test for antibodies to islet cells or insulin or testing for C peptide makes it difficult to precisely classify patients as type1 or type 2 diabetes mellitus or other forms of diabetes mellitus.
Conclusion
There is a significant admission burden of diabetes mellitus, mainly in females with type 2 diabetes mellitus. The main reasons for admission were sepsis and poor glycaemic control. There is a need to enhance public education, screening and prevention programs and manpower development in the management of diabetes mellitus.
References
- Guariguata L, Whiting DR, Hambleton I, J Beagley, U Linnenkamp, et al. (2014) Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 103(2): 137-149.
- Australian Institute of Health and Welfare (2009) Diabetes prevalence in Australia. An assessment of national data sources. Canberra, AIHW.
- Yang JJ, Danxia Yu, Wanqing Wen, Eiko Saito, Shafiur Rahman, et al. (2019) Association of diabetes with all-cause and cause-specifc mortality in Asia. JAMA Netw. Open 2(4): 192696.
- Bragg F, Michael V Holmes, Andri Iona, Yu Guo, Huaidong Du, et al. (2017) Association between diabetes and cause-specifc mortality in rural and urban areas of China. JAMA 317: 280-289.
- Policardo L, Giuseppe Seghieri, Roberto Anichini, Alessandra De Bellis, Flavia Franconi, et al. (2015) Effect of diabetes on hospitalization for ischemic stroke and related in-hospital mortality: A study in Tuscany, Italy, over years 2004-2011. Diabetes. Metab Res Rev 31(3): 280-286.
- Lin X, Xu Y, Pan X, Xu J, et al. (2020) Global, regional and national burden and trend of diabetes in 195 countries and territories: An analysis from 1990 to 2025. Scientific reports 10(1): 14790.
- Cho NH, Show JE, Karuranga S, Huang Y, da Rocha Fernandes JD, et al. (2018) IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 138: 271-281.
- Michael Hirst (2003) Brussels: International Diabetes Federation (IDF), Diabetes atlas pp. 7-11.
- Ceesay MM, Morgan MW, Kamanda MO, Willoughby VR, Lisk DR (1997) Prevalence of diabetes in rural and urban populations in southern Sierra Leone: A preliminary survey. Tropical medicine and health 2(3): 272-277.
- Nabieu PF, Massaquoi TA, Massaquoi SD, Luseni G, Idriss B, et al. (2016) Lower limb amputation at the 34 Military Hospital in Freetown, Sierra Leone: Causes and Indications. Sierra Leone Journal of Biomedical research 8(2): 9-17
- Bilandzic A, Rosella L (2017) The cost of diabetes in Canada over 10 years: applying attributable health care costs to a diabetes incidence prediction model. Health Promot Chronic Dis Prev Can 37(2): 49-53
- Al-Adsani AMS, Abdulla KA (2015) Reasons for hospitalization in adults with diabetes in Kuwait. International journal of Diabetes Mellitus 3(1): 65-69
- Ojobi JE, Dunga J, Ogiator MO, Mbaave P, Bello RN (2017) Indications and outcome of admission of diabetic patients into the medical wards in a Nigerian Tertiary Hospital- A two year review. Jos Journal of Medicine 11(2): 53-58.
- Ogbera O (2007) Burden of diabetic illness in an urban hospital in Nigeria. TropDoct 37(3): 154-154.
- Choi J, Booth G, Jung HY, Lapointe-Shaw L, Tang T, et al. (2021) Association of diabetes with frequency and cost of hospital admissions: a retrospective cohort study. CMAJ Open 9(2): 406-412.
- Reutrakul S, Deerochanawong C (2016) Diabetes in Thailand: Status and Policy. Curr Diab Rep 16(3): 28.
- Haffner SM, Lehto S, Ronnemaa T, Pyorala L, Laakso M (1998) Mortality from coronary heart disease in subjects with type 2 diabetes and non-diabetic subjects with and without prior myocardial infarction. N Engl J Med 339(4): 229-234
- Ehrlich SF, Quesenberry Jr CP, Van Den Eeden SK, Shan J, Ferrara A (2010) Patients diagnosed with diabetes are at increased risk for asthma, chronic obstructive pulmonary disease, pulmonary fibrosis, and pneumonia but not lung cancer. Diabetes Care 33(1): 55-60.
- Wielgosz A, Dai S, Walsh P, Jennifer McCrea-Logie, Ece Celebican (2018) Comorbid conditions in Canadians hospitalized because of diabetes. Can J Diabetes 42(1): 106-111.
- Barker JM, Goehrig SH, Barriga K, Hoffman M, Slover R, et al. (2004) DAISY study. Clinical characteristics of children diagnosed with Type 1 diabetes through intensive screening and follow-up. Diabetes Care 27(6): 1399-404.
- Geiss L, Engelgau M, Pogach L, Acton K, Fleming B, et al. (2005) A national progress report on diabetes: successes and challenges. Diabetes Technol Ther 7(1): 198-203.
- Robbins JM, Thatcher GE, Webb DA, Valdmanis VG (2008) Nutritionist visits, diabetes classes, and hospitalization rates and charges: the urban diabetes study. Diabetes Care 31(4): 655-660.
- Heymann AD, Shapiro Y, Chodick G, Shalev V, Kokia E, et al. (2004) Reduced hospitalizations and death associated with influenza vaccination among patients with and without diabetes. Diabetes Care 27(11): 2581-2584.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...