Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2638-5910
Case Report(ISSN: 2638-5910) 
A Rare Case of Infective Endocarditis Complicated with a Cardiac Abscess Causing Heart Block Volume 3 - Issue 4
Veshesh Patel*
- College of Osteopathic Medicine, Nova Southeastern University, USA
Received:July 31, 2021; Published:August 12, 2021
Corresponding author: Veshesh Patel, Dr. Kiran C. Patel College of Osteopathic Medicine, Nova Southeastern University, USA
DOI: 10.32474/ADO.2021.03.000170
Abstract
Individuals that have underwent cardiac surgery or heart valve replacement are at increased risk for developing infective endocarditis (IE). IE has numerous signs and symptoms as well as complications. However, an interesting and unique presentation of IE can be in an individual showing a complete heart block on EKG. A heart block from an IE will typically present with a cardiac abscess on transesophageal echocardiogram (TEE) and coronary computed tomography angiography (CTA). This individual, with a past medical history of transcatheter aortic valve replacement in 2011, was found to have Enterococcus faecalis bacteremia and endocarditis. Soon after discovery of the infection, CTA of the coronaries showed a 7.6 x 4.6 x 2.5 cm loculated pericardial collection consistent of a cardiac abscess. Despite the initiation of antibiotic therapy, this gentleman with bacterial endocarditis had an increased risk of immediate mortality, due to the complete heart block and additional complications. High clinical suspicion and early intervention are warranted for cases of infective endocarditis.
Introduction
Infective endocarditis (IE) is a deadly condition involving inflammation of the inner lining of heart chambers and valves due to infection, commonly bacterial or fungal. Individuals with heart conditions, specifically heart valve replacement or artificial heart valves, are at a greater risk of IE. [1,2]. It has a strong link to the development of a range of deleterious pregnancy outcomes, contributing considerably to maternal, perinatal morbidity and death, and can have long-term effects for both mother and offspring’s health [3]. Complications for mothers include the risk of impaired glucose tolerance (IGT) and type 2 diabetes in the years after delivery, as well as obesity and the development of IGT and diabetes in early adulthood for kids [4]. Nearly 90% of all DM-complicated pregnancies are caused by GDM [5]. GDM is becoming more common around the world, posing a major public health threat [6,7]. This rate varies by setting and population, with a prevalence ranging from 1–14 % depending on the population studied and the diagnostic tests used [8]. The frequency of GDM in Africa varies greatly, from a low %age in Tanzania to 13.9 % in Nigeria. However, according to a recent comprehensive assessment of GDM in Sub-Saharan Africa, data on the burden of GDM in various African nations, including Sudan, is lacking [9]. GDM has been linked to a number of characteristics, including age, parity, education, a family history of diabetes, and obesity [10]. In Sudan, no data on GDM has been released. For practicing doctors, caregivers, and health planners, as well as academics, determining the prevalence and risk factors for GDM is critical. The purpose of this study was to look at the prevalence and risk factors for GDM in Sudan.
Case Description
A 75-year-old gentleman, with a past medical history of hypertension (HTN), benign prostatic hyperplasia (BPH), hyperlipidemia (HLD), and transcatheter aortic valve replacement (TAVR) in 2011, presented to the emergency department (ED) accompanied by his wife reporting suicidal ideation. In the ED, the patient reported feeling depressed after his cardiologist told him a month ago that he would likely require a new aortic valve in two to five years. Patient also reported a 20 pounds (lbs) weight loss, loss of interest, and being anxious on the upcoming aortic valve replacement. He stated he has felt suicidal once before when he was originally diagnosed with aortic valve issues. Patient has been using a statin, coumadin, furosemide, metoprolol, tamsulosin, lisinopril, finasteride, and 81 mg of aspirin. On primary survey, the patients temperature was 98.3 degrees Fahrenheit with a heart rate of 67 beats per minute and blood pressure of 113/62 mmHg. The patient was alert and orientated to time, person, and place, but showed a depressed affect. On cardiovascular examination, there was regular rate and rhythm, normal heart sounds, and a systolic murmur. Electrocardiogram (EKG) showed a rate at 70 beats per minute, QRS axis -40 degrees, right bundle branch block, ST depression in the inferior and lateral leads, and T-wave inversions in lead III. Patient was found to have elevated INR at 7.69 and minimally elevated troponins at 0.2, therefore cardiology was consulted for further work up. Repeat EKG showed slightly worsening ST depressions in the lateral leads. On reevaluation, patient denied any chest pain, shortness of breath (SOB), or other cardiac related symptoms. It was recommended to discontinue coumadin at the time, trend the troponins, and order an echocardiogram as well as a stress test. Other lab abnormalities included decreased hemoglobin (Hgb) at 11.0 g/dL, elevated white blood cells (WBC) at 24.3 x 10^3/u, elevated blood urea nitrogen (BUN) at 37 mg/dL, and elevated creatinine at 1.40 mg/dL. Of note, patient was Baker acted for suicidal ideation.
Next morning, patient continued to deny any chest pain, edema, SOB, dyspnea, or pleuritic pain. The patient underwent a stress test and nuclear medicine (NM) study of the myocardium to rule out ischemia. Stress test was negative. Nuclear medicine study showed no evidence of reversible ischemia or myocardial infarct. Troponins were trending down possibly due to rehydration and correction of the acute kidney injury (AKI) caused by BPH. Echocardiogram was performed for the T wave inversions in the inferior leads and demonstrated increased left ventricular thickness, left ventricular ejection fraction (EF) at 50%, and moderate to severe aortic stenosis. Upon evaluation of the collective findings, it was found that the patient had complete heart block and was transferred to the cardiovascular intensive care unit (ICU) with bedside pacemaker with pads and atropine. In the ICU, the patient, noted to have heart block and supratherapeutic INR, showed a review of symptoms and physical examination within normal limits. However, the vitals were notable for a heart rate of 50 beats per minute and blood pressure at 94/51 mmHg with the patient afebrile. Blood cultures were performed for suspicious elevated WBCs, heart block, and patient’s history of TAVR. On both blood cultures, Enterococcus faecalis were identified. It was determined to withhold surgery for permanent pacemaker (PPM) placement for the patient due to positive bacteremia suspicious of endocarditis. Infectious disease was consulted, cardiology was notified, and a temporary pacemaker was in place.
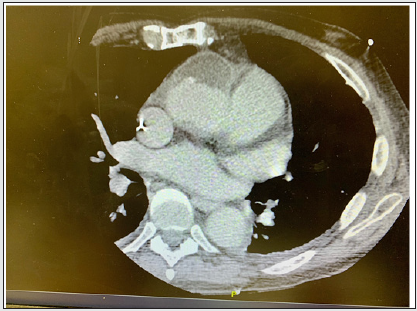
On the following day, PPM was on hold until the bacteremia is cleared, and atropine was on standby. Vancomycin and ceftriaxone were initiated. A transesophageal echocardiogram (TEE) was performed to determine to cause of the patient’s bacteremia. The results showed an aortic root abscess with severe aortic stenosis. After discussion of the possible bioprosthetic aortic abscess, cardiothoracic surgeons were consulted, and patient was scheduled for a coronary computed tomography angiography (CTA). CTA of the coronaries showed a 7.6 x 4.6 x 2.5 cm loculated precardial collection and confirmed the diagnosis (Figure 1). This illustration shows a computerized tomography (CT) scan of a rare complication of infective endocarditis causing a cardiac abscess. This image depicts a 7.6 x 4.6 x 2.5 centimeters (cm) loculated collection (yellow arrow) measuring in the precardial space. An infective abscess near the aortic valves can compress local structures and disrupt the atrioventricular (AV) conduction. As a result, IE can result in first-degree, second-degree, or complete heart blocks. Given the findings on CTA and active endocarditis, the patient was a high-risk surgical candidate with an elevated risk for mortality and poor outcome. Patient wished to be do-not-resuscitated (DNR) and do-not-intubate (DNI). Patient opted for hospice and all care was removed including temporary pacemaker. Patient was in hospice care for three days until he passed away.
Discussion
Initially, this gentleman presented to the ED for suicidal ideation and depression when he discovered that he would require a new aortic valve. After further workup, it was found that the patient developed bacteremia and complete heart block from the aortic root abscess. In one case report on infective endocarditis presenting as depression, it detailed how a stroke manifested into neurological and psychiatric symptoms, such as depression, after an embolization of a clot from an infective endocarditis [2]. Although this patient did not undergo a workup for stroke, there may be a correlation between the patient’s suicidal ideations and the infective endocarditis. This patient denied any chest pain or cardiac related symptoms. However, the patient had slightly elevated troponins and an abnormal EKG. It was necessary to workup myocardial infarction (MI) and ischemic causes. When the workups came back negative, the next step was to obtain an echocardiogram. The echocardiogram entailed features of longstanding aortic stenosis and decreased left ventricular function. Although the patient was afebrile and had an unusual presentation of endocarditis, blood cultures were ordered because the patient had elevated WBCs, a heart block, and a history of TAVR. The findings to the blood cultures were significant and identified as Enterococcus faecalis. Enterococcus faecalis is part of the normal gut flora, mostly genitourinary tract, and can seep into the systemic circulation to cause an infection. E. faecalis is the third leading cause of infective endocarditis, being responsible for 5% to 15% of cases [3]. The patient was unable to get a permanent pacemaker (PPM) placement because bacteremia is a contraindication for surgery.
In this case of IE, the patient had developed bioprosthetic aortic abscess evidenced by the findings of the TEE and CTA of the coronaries. A cardiac abscess is a collection of pus, which are dead neutrophils and its degradative enzymes. When there is a suppurative infection of the myocardium, endocardium, or prosthetic valve, it can result in a cardiac abscess [4]. There is a higher incidence at 30% to 40% for perivalvular abscess among patients with infective endocarditis. Additionally, there is greater predisposition with the aortic valve than the mitral valve. For this patient, the abscess caused a complete heart block which likely resulted from direct extension from the aortic root of the infectious process to the AV node or bundle of His [5]. A cardiac abscess can also cause abnormal communication between the cardiac chambers, pericardial disease, and myocardial ischemia. Patients with bacterial endocarditis have an increased risk of immediate mortality (30%), despite the initiation of antibiotic therapy, and if complicated with complete heart block, it will contribute to a poorer prognosis [5].
Conclusion
Infective endocarditis has many complications, but one notably rare consequence is developing an abscess. As demonstrated in this case, a cardiac abscess located at the aortic root can impinge the AV conduction pathways and result in complete heart block. Prompt treatment of the bacteremia and endocarditis-induced abscess is urgent after imaging workup. Treatment includes antibiotic therapy for the infection as well as a permanent pacemaker placement for the heart block. However, the prognosis is very poor and there is a high mortality rate. Therefore, IE warrants a very high clinical suspension to prevent further consequences.
References
- Jameson JL, Fauci AS, Kasper DL (2018) Infective endocarditis. Harrison's Principles of Internal Medicine (20th Edn) McGraw Hill, USA.
- Kallivayalil AM, Keerthy R, Silvin SP (2021) Infective endocarditis presenting as depression: A case report. Telangana Journal of Psychiatry.
- Khan Z, Siddiqui N, Saif MW (2018) Enterococcus Faecalis Infective Endocarditis and Colorectal Carcinoma: Case of New Association Gaining Ground. Gastroenterology Res 11:238-40.
- Fergie J Ramos Tuarez, Varun S Yelamanchili (2020) Mark A Law: Cardiac Abscess, NCBI.
- Wang K, Gobel F, Gleason DF, Edwards JE (1972) Complete heart block complicating bacterial endocarditis.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...