Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4692
Mini Review(ISSN: 2637-4692) 
Thyroglossal Duct Cyst in the Floor of Mouth: An Unusual Finding Volume 1 - Issue 5
Fuenmayor LG1*, Liceaga R2, Mosqueda A3 and Bustos LM4
- 1Oral Surgery Department, Autonomous University of Baja California, Mexico
- 2Oral and Maxillofacial Surgery Department, General Hospital of Campeche, Mexico
- 3Oral and Maxillofacial Pathology Department, Autonomous Metropolitan University, Mexico
- 4Oral and Maxillofacial Surgery Department, Autonomous University of Aguascalientes, Mexico
Received: March 21, 2018; Published: March 26, 2018
Corresponding author: Fuenmayor LG, Dentistry Coordinator, School of Health Science Valle de las Palmas, Autonomous University of Baja California. Boulevard Universitario numero 1000, Baja California, Mexico, P.C 22260
DOI: 10.32474/MADOHC.2018.01.000122
Abstract
The cyst of the thyroglossal duct is a benign congenital malformation, in which the thyroglossal conductor fails to obliterate, before descending towards the thyroid gland. (TDC) is one of the most frequent pathologies found in the midline of the neck. Approximately 7% of the population has thyroglossal remnants, which represents 70% of the head and neck pathologies. We Present a case of a 45-year-old male patient attended consultation with Maxillofacial Surgery referring to difficulty in swallowing and episodes of sleep apnea. Under General anesthesia, and nasotracheal intubation the lesion was removed with no further recurrence or the lesion.
Introduction
The thyroglossal duct cyst (TDC) is one of the most frequent pathologies found in the midline of the neck. Approximately 7% of the population has thyroglossal remnants, which represents 70% of the head and neck pathologies [1]. It is important to point out that, although the thyroglossal duct cyst occurs mainly in children; It can also occur in adults. Most of these are near the hyoid bone, however, they can be located anywhere on the descending path to the thyroid cartilage [2]. 85% of the cases are below the hyoid bone [3]. The understanding and knowledge of both embryology and the anatomy of the tongue are necessary for successful treatment [4,5].
Case Report
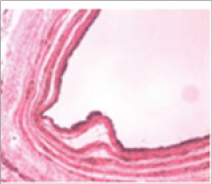
A 45-year-old male patient attended consultation with Maxillofacial Surgery referring to difficulty in swallowing and episodes of sleep apnea; as well as changes in the tone of the voice. Clinically, there is an increase in volume in the floor of the mouth, which protrudes the tongue and causes dysphonia (Figure 1). The patient had been treated by Otorhinolaryngology for the difficulty in breathing and at the time of the consultation came with a Waters X-ray only. He is later indicated computed tomography; where hypodense image can be observed for soft tissues of approximately 10mm x 5mm x 8mm, located on the floor of the mouth above the mylohyoid muscle (Figure 2). An aspiration puncture was made, in which whitish liquid without odor was observed. It was decided to plan the surgical excision under general anesthesia. Within the differential diagnoses that we had contemplated were; Dermoid cyst, epidermoid cyst, cystic hygroma, plunging ranula. Under General anesthesia, and nasotracheal intubation. An incision is made on the floor of the mouth horizontally, above the sublingual caruncle; (Figure 3) by blunt dissection the lesion is completely dissected (Figure 4) until its complete excision in a single piece (Figure 5). The Piece is sent to histopathological study where it is diagnosed as Thyroglossal Duct Cyst. The main histological findings were. A cystic wall of loose fibrous tissue, well vascularized, surrounded by bundles of striated muscle and adipose tissue of normal characteristics. The cavity is lined by a pseudostratified ciliated cylindrical epithelium, without findings of malignancy (Figures 6 & 7). Due to the unusual location of this entity in the sublingual region, in the floor of mouth, as well as the few reports of the literature we saw ourselves in the task of making the report of this case.
Figure 1: Clinical view of the lesion, we observed the elevation of the floor mouth and tongue.

Figure 2: CT image coronal view. Size of the pathology can be determinate.

Figure 3: Horizontal incision over the floor of mouth prior to resection.

Figure 4: Complete dissection and resection of the lesion.

Figure 5: Clinical we of the lesion after the complete resection.
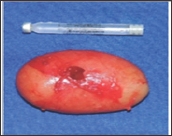
Figure 6: Histological findings, a cystic wall of loose fibrous tissue, well vascularized, surrounded by bundles of striated muscle and adipose tissue of normal characteristics.
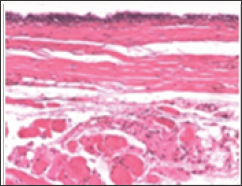
Figure 7: The cavity is lined by a pseudo stratified ciliated cylindrical epithelium, a Thyroglossal Duct Cyst was confirmed.
Discussion
The cyst of the thyroglossal duct is considered to be a benign congenital malformation, in which the thyroglossal conductor fails to obliterate, before descending towards the thyroid gland [6]. The QCT is the second most frequent neck pathology in pediatric patients, after lymphadenopathy [7]. It can present at any age, being more commonly observed during childhood, at approximately 5 years, however one third of these cysts are visible after [8]. There are 4 common locations. Intralingual (2.1%), suprahyoid, (24%) Tirohyoid (60.9%) and suprasternal [9]. (12.9%) Although, they have also been reported in up to 6 locations [6]. Our case is one of the least frequent locations reported. When the cyst appears in the neck and enucleation is performed; it is common to expect recurrence, so the recession of the hyoid has been suggested [10]. Promulgated by Changle in 1893 with a relapse of 20% and later by Sistrunk which eliminated the remaining tissue of the hyoid, reducing the recurrence by 3% [11]. However, when it is presented in the oral cavity and its enucleation is performed, no recurrence has been reported like the case presented. Factors that have been associated with the occurrence of these cysts in unusual locations include the presence of an ectopic foramen cecum, an abnormal route in the descent of the hyoid, and a lateral branch of the thyroglossal duct [12,13].
Histologically, the cystic wall is lined by a columnar epithelium; Thyroid tissue and mucus-producing cells which can also be isolated sometimes in the area [14]. In our case, a cystic capsule composed of a lax tissue epithelium was present and the epithelium was a columnar pseudostratified columnar type, although they were not isolated remnants of thyroid tissue in the lesion. Cysts of the Tiroglosal duct are rarely associated with ectopic thyroid tissue, although, occasionally associated with the lingual thyroid; which is presented as an increase in volume at the base of the tongue [15]. Only 1% of cases show malignancy data. Cases of incidental findings of primary thyroid papillary carcinomas in TDC have also been reported [16-18].
Conclusion
The thyroglossal duct cyst in the sub lingual region is one of the less frequent reported locations, unlike its usual presentation in the neck. The treatment of this lesion is surgical, a computed tomography its necessary to determine the approach and extension of the same one. It is also recommended to perform ultrasound and rule out the presence of lingual thyroid. Once the lesion was eliminated, the symptoms of dyspnea and dysphonia disappeared, as well as swallowing. Although in this case it was not mandatory to perform the classic Sistrunk technique, the patient evolved satisfactorily and without recurrence of the lesion.
References
- Ewing CA, Kornblut A, Greeley C, Manz H (1999) Presentations of thyroglossal duct Cysts in adults. Eur Arch Otorhinolaryngol 256(3): 136-138.
- Athow AC, Fagg NLK, Drake DP (1989) Management of thyro-glossal cysts in children. Br J Surg 76(8): 811-814.
- Boswell WC, Zoller M, Williams JS, Lord SA, Check W (1994) Thyroglossal duct carcinoma. Am Surg 60(9): 650e5.
- Nour YA, Hassan MH, Gaafar A, Eldaly A (2011) Deep neck infections of congenital causes. Otolaryngol Head Neck Surg 144(3): 365-371.
- Shion Saito, Kaoru Onidani, Shuji Yoshid, Isao Kamiyama, Aki Itoa, et al. (2016) A case of thyroglossal duct cyst on the oral floor of a neonate.Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology 28: 535-540.
- Sprinzl GM, Koebke J, Wimmers Klick J, Eckel HE, Thumfart WF (2000) Morphology of the human thyroglossal tract: a histologic and macroscopic study in infants and children. Ann Otol Rhinol Laryngol. 109(12): 1135-1139.
- Tracy TF, Muratore CS (2007) Management of common head and neck masses. Semin Pediatr Surg 16(1): 3-13.
- Sailesh Mukul, Amit Kumar, Ejaz Mokhtar (2016) Sublingual thyroglossal duct cyst (SLTGDC): An unusual location. Journal of Pediatric Surgery Case Reports 10: 3-6.
- Enepekides DJ (2001) Management of congenital anomalies of the neck. Facial Plast Surg Clin North Am 9(1): 131-145.
- Organ GM, Organ CH (2000) Thyroid gland and surgery of the thyroglossal duct: exercise in applied embryology. World J Surg 24(8): 886-890.
- Maran AGD (1997) Benign diseases of the neck. In: Kerr AG (Ed) Scott- Brown's otolaryngology, 6th Edn. Butterworth Heinemann, Oxford, pp 1-19.
- Sistrunk WE (1986) The surgical treatment of cysts of the thyroglossal tract. Ann Surg 7: 121-124.
- Bennett KG, Organ CH, Williams GR. Is the treatment for thyroglossal duct cysts too extensive? Am. J. Surg 152: 602-605.
- Takeda M, Noguchi M, Harada M, Yasunaga J, Nagai I, et al. (2001) A case ofthyroglossal duct cyst of the anterior part of the dorsum of the tongue. Jpn JOral Maxillofac Surg 47: 634-636.
- Soucy P, Penning J (1984) The clinical relevance of certain observations on the histology of the thyroglossal tract. J Pediatr Surg 19: 506-509.
- Welch KJ, Randolph JG, Ravitch MM, O'Neill JA, Rowe MI (1986) Pediatric surgery. 4th Edn. Chicago: Year Book Medical Publishers Inc.; p. 539-552.
- Sujatha Narayana Moorthy, Rekha Arcot (2011) Thyroglossal Duct Cyst- more than Just an embryological remnant. Indian J Surg 73(1): 28-31.
- Aggarwal H, Wadhera S, Raikwar RS, Shukla S, Mathur RK (2007) A rare case of incidentally diagnosed primary papillary carcinoma of thyroglossal duct cyst. Indian J Surg 69: 145-146.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...