Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4692
Research Article(ISSN: 2637-4692) 
The Associations between Childhood Dental Caries and Socio-Demographic Factors and the Impact of a Brief Dental Intervention on Improving Parental Knowledge Volume 5 - Issue 5
Amamilo Ifeyinwa B1*, Vikram Palit1, Sagar Vishwakarma22, Al Jaddir Ghaida2, Bedford Helen1 and Winyard Paul1
- 1Institute of Child Health, University College London, UK
- 2Chelsea and Westminster Hospital NHS Foundation, UK
Received: November 17, 2022; Published: December 5, 2022
Corresponding author: Amamilo Ifeyinwa B, Great Ormond Street Institute of Child Health, University College London, 30 Guilford St, London WC1N 1EH, UK
DOI: 10.32474/MADOHC.2022.05.000221
Abstract
Objective: Dental caries is the most common chronic disease of childhood and largely preventable with good oral hygiene practices. Identifying the multiple, contextual risk factors that contribute to decay is important to inform public health interventions. This study aimed to investigate associations between developing childhood caries and socio-demographic and parental factors. It also evaluated the suitability and impact of a dental public health intervention on improving parental oral health knowledge.
Methods: This was a pre/post single cohort interventional study (assessing the brief dental intervention (BDI) and its effect on knowledge) carried out over 12 months. Parents of children under ten years referred to as pediatric dental outpatients were recruited. Questionnaires (pre- & post-intervention) were administered to assess caregiver’s oral health knowledge/practice; after a subset of study participants received a BDI. Data were analyzed using SPSS, p-value and confidence interval were set at <0.05 and 95% respectively.
Result: The onset of tooth-brushing after one year of age increased odds of caries by 3.07 (95%CI 1.46-6.49). First dental appointment after age two, increased caries by four times (95%CI 2.06-7.81). Low maternal education increased the risk for caries [p=0.004]. The BDI led to a significant observed difference in pre- and post-intervention parental oral health knowledge [p<0.0001 across all variables].
Conclusion: Multiple socio-demographic factors are associated with developing caries including ethnicity, level of maternal education, timing of onset of tooth-brushing and first dental visit. Brief dental interventions show significant potential to improve parental knowledge of oral health.
Keywords: Dental caries; decay; oral health; childhood; pediatric; dental brief intervention, parental dental knowledge
Introduction
Dental caries in childhood (DCC) though preventable, constitutes one of the leading childhood diseases worldwide with significant, long-lasting impact on the child, family and community. Dental decay is the leading cause for hospital admission of children aged 5-9 years, and almost a quarter of under 5-year-olds in England suffer from some form of dental decay [1]. Contemporary perspectives in pediatric dental health describe an increasing awareness of the complex interplay of genetic, social and economic factors in the causal pathway of DCC [2]. Parental supervision of dental hygiene is instrumental in supporting good, early oral habits in children. Several factors including parental attitudes, belief and knowledge influence their capacity to support appropriate childhood dental practices. Dental visits, school education programs, health visiting and primary and secondary care services all present multiple opportunities for oral health promotion messages to be delivered during early childhood years. However, inconsistency, suboptimal and poor delivery of public health messages can lead to poor parental oral health knowledge, and this has shown to be strongly associated with DCC in England [3,4]. Brief interventions, involving structured, evidence-based dialogue between healthcare providers and patients, has been employed in multiple public health settings to motivate positive behavioral change [5]. However, their impact on oral child health has not been fully established and this has contributed to inconsistencies in the use of brief dental interventions (BDI) and their delivery in pediatric dental health [6,7]. To date, a number of oral health interventions involving parental education have been performed in the United Kingdom with varying results on parental oral health knowledge and dental practices [8-10]. This observational study sought to investigate the risk factors that contribute to DCC and the impact of a brief dental intervention to improve parental oral heath knowledge. Brief public health interventions that reinforce good oral health practices over multiple episodes of care may be an effective strategy to address the preventable risk factors that contribute to dental decay in childhood.
Methodology
Study area and population
This pilot observational study was undertaken at Chelsea and Westminster Hospital, a large teaching hospital in North West London, United Kingdom. It was an observational cross-sectional (assessing risk factors), and a pre/post single cohort interventional study (assessing the BDI and its effect on knowledge). Parents of children aged under 10 years who were referred to the pediatric dental outpatients were invited to participate in the study.
Study protocol
Study investigators who were either medical or dental professionals and had completed additionally two-day online training on primary dental care, developed the ‘Big Bites and Pearly Whites’ (BBPW) protocol, made up of pre- and post-intervention questionnaires assessing parental dental health knowledge and a 10-15-minute BDI that provided parents/caregivers with evidencebased verbal and written information about caring for children’s teeth. Ethics approval was granted by the Chelsea and Westminster local research committee, and the NHS Health Research Authority. From February 2018 to February 2019, the parents/caregivers of children under 10 years who presented to the pediatric dental out-patients department were consecutively approached by the researchers, during the clinic appointments. The study objectives, procedures, risks and benefits (tertiary prevention of caries in index child and/or possible prevention in younger siblings) were discussed with them after which written consent, were obtained from those who voluntarily accepted to be part of the study. They subsequently completed a 40-point pre-intervention questionnaire which collected anonymous demographic data and assessed each caregiver’s oral health literacy. Subsequently, a cohort of participants (178) chosen via systematic sampling (every 3rd parent of child referred to the Paediatric dental outpatient) was allocated to receive the BDI from one of the study investigators. The BBPW intervention advised caregivers on three key aspects of childhood dental health including the importance of early and regular visits to the dentist, twice daily tooth-brushing with fluoride toothpaste, and dietary recommendations to reduce total sugar intake. Participants that had received the BDI were asked to complete a post-intervention questionnaire assessing their retained oral health knowledge and overall experience and suitability of the intervention in practice.
Data analysis
The data collected was characterised using descriptive statistics. While categorical variables were summarized using frequencies/proportions, means and standard deviation were used for the numerical variables. The Fisher’s exact and Chi-square tests were used to evaluate relationships between caries and sociodemographic risk factors, parental oral health knowledge and practice. Significance testing involving paired categorical variables was done using Mc-Nemar’s test. Logistic regression was used to estimate the odds ratio (OR), 95% confidence intervals and p-values.
Result
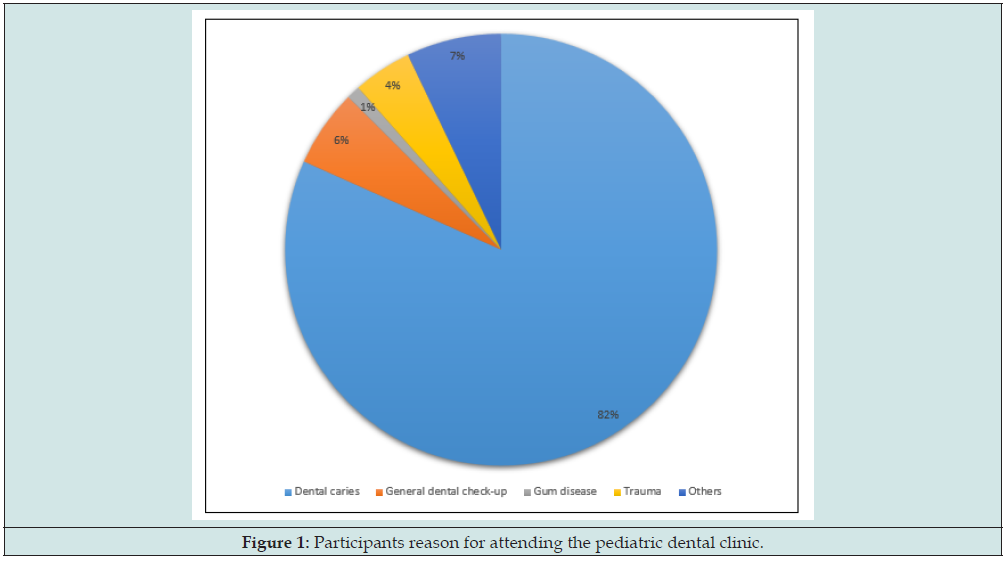
In total, 295 parents and caregivers of children referred to the pediatric dental outpatients were recruited to this study. Of them, 241 or 82% of study participants had children who were referred for dental caries, with the remaining reasons for referral shown in Figure 1. The mean age of the child was 5.86 years, with a male to female ratio of 1.3:1. Table 1 shows the sociodemographic distribution of the participants. Two hundred (68%) of the caregivers were employed, while 49.8% (n=147) of the children seen had mothers achieving tertiary level education. Among the participants, 55 (40.3%) and 100 (22.3%) of their children had siblings with previous history of caries and tooth extractions respectively. Most mothers [n=211 (71.5%)] self-reported to have dental caries.
Oral health knowledge and practice of parents/ caregivers
282 (95.6%) participants knew children’s teeth should be brushed twice daily, 164 (55.5%) reported that the duration of tooth-brushing should be two minutes. 232 (78.6%) of study participants did not know the recommended fluoride content of their children’s toothpaste (Table 2). Regarding parental dental practices (Table 3), only 38.6% (n= 114) started to brush their children’s teeth before the child’s first year and 30.5% (n=90).
n a =293; n b =294; n c = 295; n d = 247; n e =248, SD- standard deviation
Association between caries and socio-demographic factors
There was significant association between caries and ethnicity, being Asian/Asian British (AAB) increased the odds of having caries by approximately four times [OR (95%CI) = 3.50 (1.45-8.43)] compared to their WWB counterparts. Likewise, low maternal education, not having caries and tooth extractions in other children significantly increased developing caries [p-value = 0.004; 0.002; and 0.008 respectively] (Table 4).
(*)- significant result, OR- Odds ratio, CI- Confidence interval
Association between caries and parental oral health knowledge and practices
(***)- significant result, OR- Odds ratio, CI - Confidence interval
Significant associations were found between caries and age at onset of tooth-brushing and age at the first dental visit (p<0.001) (Table 5). Starting to brush children’s teeth after one-year increase the odds of having caries by three times, which was doubled when tooth-brushing was commenced after two-years [OR (95% CI) = 3.07 (1.46-6.49), OR (95% CI) = 6.04 (2.24-16.27)]. Equally, those who had their first dental visit after two-years were 4-times more likely to have caries {OR (95% CI) = 4.02 (2.06-7.81), OR (95% CI) = 5.13 (1.13-23.22)}.
Impact of BDI
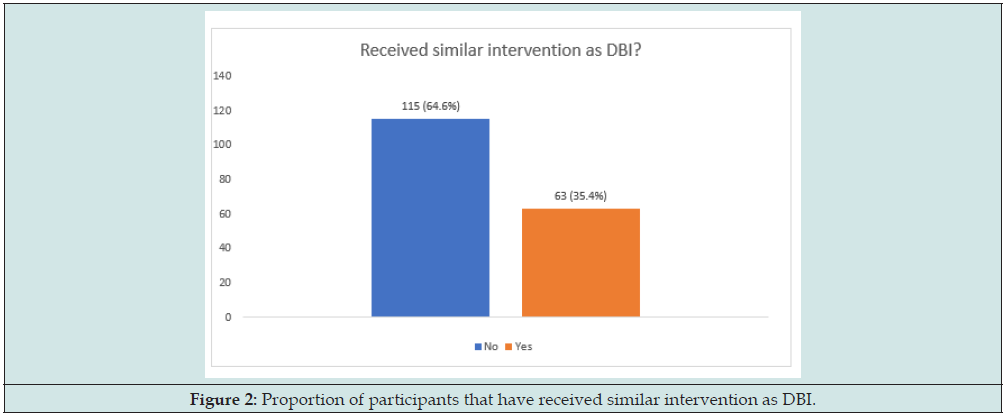
Following BDI, 115 (64.6%) of the participants reported they had not received similar advice before (Figure 2), and a significant increase in oral health knowledge among parents/caregivers was observed (p<0.0001 for all the categories) (Table 6). Caregivers’ knowledge regarding the duration and frequency of daily toothbrushing increased by 47.2% and 23.6% respectively; while their knowledge of the recommended frequency that toothbrushes should be changed (3 months) showed a 38.8% improvement.
†n= 178, (***)- statistically significant.
Discussion
In this study, an individual’s ethnicity was shown to have a significant association with developing childhood caries. The finding that AAB and BAC children were more likely to have caries compared to WWB children is consistent with the 2015 Public Health England (PHE) survey that showed that Chinese followed by the East-European populations had a three times higher proportion of dental caries compared to other ethnic groups [11]. However, a more recent PHE survey in 2018 reported more caries in the East-European children followed by the Chinese [12]. It is possible that the prevailing social deprivation among minority and immigrant populations may be responsible for this finding and reflect the impact of social inequalities which need to be addressed. Nevertheless, some authors linked it to culturally related oral health beliefs, child-rearing and infant feeding practices [13,14]. The finding that low-level maternal education increases caries agrees with many studies [15,16]. In this study, the reason for greater odds observed for mothers who had secondary education is not apparent but may be explained by the greater number of participants having secondary education compared to primary education. [17] Kinirons and McCabe reported a 40% prevalence of caries among preschoolers whose mothers had low levels of education as opposed to 10% in those whose mothers had high levels of education. Similarly, [18] Wei and colleagues in Hong Kong observed that mothers who had high level of education took their children for first dental visits earlier than the others and, this affected dental outcomes. Caregiver’s education is suggested to influence family income, oral health literacy, feeding habits, lifestyle choices and ultimately oral practices [19], therefore, oral health messages should be simple and easy to understand with consideration of those with limited education.
Interestingly, this study found that not having caries and/or tooth extractions in siblings increased the odds of having caries. Not having a child with oral problems may result in reduction in acquiring oral health knowledge and give caregivers a sense of ‘false security’ regarding adequate dental practices. [20] Dobloug corroborated this in their study that found that having caries and/ or tooth extractions in siblings reduced the odds of subsequent children having caries. They suggested that previous caries experience in a sibling creates a positive oral health environment, possibly from improved knowledge and practice resulting from frequent interactions with dental personnel. On the contrary, [21] Folayan reported an increased odd of caries in children whose siblings had caries. They argued that this could be resulting from similar socioeconomic factors impacting the children, strengthening the multifactorial aetiology of DCC. Participants in this study showed poor knowledge of the recommended content of fluoride in toothpaste and duration of brushing. This is consistent with the findings of several authors around the world [22-24]. [2] Olley attributed this poor knowledge to a deficiency in the delivery and content of preventive oral health messages by dental practitioners in the UK, also highlighting the quality and impact of the existing community and school-based oral health programs. Also, substantiating the need for the evaluation of these programs to improve their effectiveness across the UK. In this study, caries was found to be significantly associated with the onset of toothbrushing after the first year- and first dental visit after the second year-of-life. These findings corroborate with recommendations of PHE concerning age at onset of tooth-brushing and early dental visits [1]. The findings also agree with many reviews showing that early onset of tooth-brushing and dental visits can influence habitforming and go on to influence dental outcomes [24-27]. Across all the parameters assessed post-intervention, there was significant increase in caregivers’ oral health knowledge showing promising evidence on use of BDI. Though this finding is encouraging, it did not indicate better dental outcomes amongst participants, since only short-term memory was tested. However, these outcomes are expected to be assessed at the end of the three-year project, nevertheless, earlier evidence indicate that BDI has the ability to improve use of preventive dental care and to reduce dental disease rates [28].
Conclusion and recommendations for future research
This study identified that sociodemographic factors including ethnicity, maternal education, previous history of caries and/or tooth extractions in other children, age at onset of tooth-brushing and first dental visit significantly influenced DCC among the study participants. It also highlights oral health knowledge and poor practice gap caregivers/parents that may be contributory to the increasing rates of DCC among their children. Consequently, Health professionals need to coordinate and maximize their efforts to deliver clear preventive advice to enhance and increase parents’ knowledge towards their children’s oral health. Given the high acceptability and promising impact of BDI to address these knowledge-practice deficiencies of caregivers, it is hoped to contribute to the development of oral health preventive strategies in NWL and beyond.
Conflict of Interest:
Nil
Acknowledgement
We would like to thank the staff of the pediatric, dental and general outpatient clinics at Chelsea and Westminster NHS Foundation Trust for their support and help with recruitment.
References
- (2015)Public Health England. Rapid Review to Update Evidence for the Healthy Child Programme 0-5 United Kingdom.
- Fisher-Owens SA, Gansky SA, Platt LJ, Weintraub JA, Soobader MJ, et al. (2007) Influences on Children’s Oral Health: A Conceptual Model. Pediatrics 120(3): e510-e520.
- Olley R, Hosey M, Renton T, Gallagher J (2011) Why are children still having preventable extractions under general anesthetic? A service evaluation of the views of parents of a high caries risk group of children. British dental journal 210(8): E13.
- Tickle M, Milsom K, King D, Blinkhorn A (2003) The influences on preventive care provided to children who frequently attend the UK General Dental Service. British dental journal 194(6): 329-332.
- Henry-Edwards S, Humeniuk R, Ali R, Monteiro M, Poznyak V (2003) Brief intervention for substance use: A manual for use in primary care. World Health Organization, Geneva.
- Riedy CA, Weinstein, P, Mancl L, Garson G, Huebner CE, et al. (2015) Dental attendance among low-income women and their children following a brief motivational counselling intervention: a community randomized trial. Social Science & Medicine 144: 9-18.
- Finlayson TL (2017) Limited Evidence Shows That a Motivational Interviewing Approach May be the Most Effective Behavioral Intervention for Reducing Dental Caries in Children. Journal of Evidence Based Dental Practice 17(2): 129-131.
- Blinkhorn AS, Gratrix D, Holloway PJ, Wainwright‐Stringer YM, Ward SJ, et al. (2003) A cluster randomized, controlled trial of the value of dental health educators in general dental practice. British Dental Journal 195(7): 395-400.
- Clarkson JE, Young L, Ramsay CR, Bonner BC, Bonneti D (2009) How to influence patient oral hygiene behavior effectively. Journal of Dental Research 88(10): 933-937.
- Ley-Barber I, Hann G, Singh G, Palit V, Al-Jaddir G (2019) The associations between social factors and suboptimal use of pediatric dental services (Tiny Teeth): a mixed method study. Meeting abstracts, The Lancet 394: 66.
- (2016) Public Health England. National Dental Epidemiology Programme for England: oral health survey of five-year-old children 2015: A report on the prevalence and severity of dental decay.
- (2018) Public Health England. National Dental Epidemiology Programme for England: oral health survey of five-year-old children 2017: A report on the inequalities found in prevalence and severity of dental decay.
- Holt R, Winter G, Downer M, Bellis W, Hay I (1996) Caries in pre-school children in Camden 1993/94. British dental journal 181(11-12): 405.
- Prendergast MJ, Beal JF, Williams SA (1997) The relationship between deprivation, ethnicity and dental health in 5-year-old children in Leeds, UK. Community dental health 14(1): 18-21.
- Sanders LM, Federico S, Klass P, Abrams MA, Dreyer B (2009) Literacy and child health: a systematic review. Archives of Pediatrics & Adolescent Medicine 163(2): 131-140.
- Kim Seow W (2012) Environmental, maternal, and child factors which contribute to early childhood caries: a unifying conceptual model. International Journal of Paediatric Dentistry 22(3): 157-168.
- Kinirons M, Mccabe M (1995) Familial and maternal factors affecting the dental health and dental attendance of preschool children. Community dental health 12(4): 226-229.
- Wei S, Holm A, Tong L, Yuen S (1993) Dental caries prevalence and related factors in 5-year-old children in Hong Kong. Pediatric dentistry 15(2): 116-119.
- Dobloug A, Grytten J (2016) Correlation between siblings in caries in Norway. A quantitative study. Community dentistry and oral epidemiology 44(5): 416-425.
- Folayan MO, Owotade F, Oziegbe EO, Fadeyibi R (2010) Effect of birth rank on the caries experience of children from a suburban population in Nigeria. Journal of Dentistry and Oral Hygiene 2:27-30.
- Rwakatema DS, Nganga PM (2009) Oral health knowledge, attitudes and practices of parents/guardians of pre-school children in Moshi, Tanzania. East Afr Med Journal86(11): 520-525.
- Blinkhorn A, Wainwright‐Stringer Y, Holloway P (2001) Dental health knowledge and attitudes of regularly attending mothers of high‐risk, pre‐school children. International dental journal 51(6): 435-438.
- Alyahya L (2016) Parental knowledge and practices regarding their children's oral health in Kuwait. European Journal of Paediatric Dentistry 17(4): 267-273.
- Hiba SA, Amal HA (2016) Knowledge and Practice of Mothers in Relation to Dental Health of Pre-School Children. Advancements in Genetic Engineering 5: 2
- Arora A, Manohar N, John JR (2017) Factors associated with dental caries in primary dentition in a non-fluoridated rural community of New South Wales, Australia. International Journal of Environmental Research and Public Health 14(2): 1444.
- Hallett K, Orourke P (2003) Social and behavioral determinants of early childhood caries. Australian dental journal 48(1): 27-33.
- Pine CM, Adair PM, Petersen PE, Douglass C, Burnside G, et al. (2004) Developing explanatory models of health inequalities in childhood dental caries. Community dental health 21: 86-95.
- Weinstein P, Harrison R, Benton T (2004) Motivating parents to prevent caries in their young children: one-year findings. The Journal of the American Dental Association 135(6): 731-738.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...