
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4692
Mini Review(ISSN: 2637-4692) 
Salivary Gland Imaging: Visualization of the Oral Lubricator Volume 1 - Issue 4
Yadav Karthik* and Pai Anuradha
- Department of oral medicine and radiology, The Oxford Dental College and Research Center, India
Received: March 09, 2018; Published: March 13, 2018
*Corresponding author: Karthik D Yadav, Department of Oral Medicine and Radiology, The Oxford Dental College and Research Center, India
DOI: 10.32474/MADOHC.2018.01.000118
Introduction
The oral cavity is often called the mirror of an individual's health. The maintenance of the oral cavity is mainly dependent on saliva and its importance is unspoken, unless and until these changes exhibit their importance by a decrease or increase in its levels. Saliva is a glandular secretion secreted by the salivary glands which are exocrine in nature. Saliva acts constantly by bathing the teeth and the oral cavity, providing the flush, lubricative and protective action, all of which are essential for the maintenance of healthy oral tissues and daily functions. There are 3 major glands -parotid, sub mandibular and sublingual glands and numerous minor glands scattered throughout the oral cavity [1,2]. A wide range of disease processes may affect the salivary glands which might be inflammatory, systemic, obstructive or neoplastic in nature. Imaging plays an imperative role in detection, diagnosis and differentiation of benign from malignant lesions [2,3].
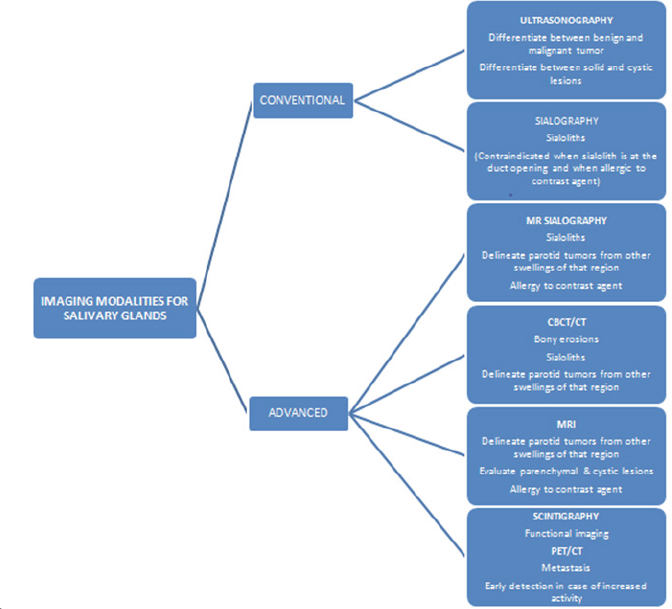
The imaging modalities include both conventional as well as advanced imaging modalities. The conventional modalities include plain radiography and sialography whereas ultrasound, contrast enhanced CT, MRI and MR sialography constitutes the modern imaging modalities [2,4]. Conventional plain film Radiography and Sialography were widely used formerly but are seldom used nowadays as they are of limited value. Plain film radiography is the most conventional and simplest mode of imaging. They can be used to detect the mineralized salivary calculi with a single or two radiographs with altered angulations to evade super imposition [5]. The availability of advanced imaging modalities has limited its use in this era [6].
Ultrasound
Ultrasound is the maiden noninvasive, economical investigative tool of choice due to its high spatial resolution, easy availability and not to forget its capability to guide.com in needle biopsy, using its high frequency probe in the 7-15MHz range [2,3]. It is the investigation of choice for major salivary gland disease for delineating benign and malignant lesions, especially superficial lesions [2]. However, the deep portion of the parotid gland is difficult to visualize because of the presence of bony ramus which lies over the deep lobe. US can also evaluate gland parenchyma and large ducts as well as reveal ductal dilatation. It can additionally be employed as imaging guidance for fine-needle aspiration (FNA) and core biopsy [7]. Ultrasound with Color Doppler has further enhanced the diagnostic significance of ultrasound. Ultrasound can detect around 95% of space occupying lesions of major salivary glands [8]. A sensitivity of 90%and 94% has been observed in detecting calculi of <3 and>3 mm in case of sialolithiasis [6].
Scintigraphy
In 1946 Schiff detected that iodine 131 can be concentrated in salivary glands and eliminated by saliva and later in 1950 Myant et al introduced this functional diagnostic and morphological technique termed as scintigraphy. Later Technetium 99 was found as a more suitable isotope [3]. It is used to assess the salivary gland function and to determine abnormalities in glandular uptake and excretion [2,3]. Scintigraphy is perhaps the only salivary imaging technique providing information on the functional capabilities of the glands [3]. Scintigraphy is indicated for the evaluation of patients when sialography is contraindicated or cannot be performed, such as in cases of acute gland infection or iodine allergy, or in cases where the major duct cannot be cannulated successfully.
It is a useful adjunct to aid in the diagnosis of salivary gland duct obstruction, salivary stones, glandular aplasia and Sjogren's syndrome [2,3]. There are several rating scales for evaluating the salivary scinti-scans, yet there is no standard rating method as of now. The prevailing approaches to functional assessment include visual interpretation, time-activity curve analysis, and numeric indices. Most radiologists read Tc 99m scans by using visual interpretation along with clinical judgment of the interpreter. Although a semi quantitative method exists in which Tc 99m uptake and secretion is calculated by computer analysis of a user-defined region of interest, these time-activity region of interest studies are quite time-consuming and mostly used for research purpose [3].
Positron Emission Tomography (PET)
A non invasive imaging modality that can be used to study pathological and physiological processes in the body, with further advantage of anatomical localization. PET scanning involves usage of radiotracers, which subsequently decay, with radiation of positively charged particles called positrons. The CT data is obtained during scanning and the PET data is combined with CT that helps in localization of this radiotracer. The main application of PET/CT is in the assessment of patients with salivary gland tumors using the glucose analogue 2-[18] fluoro- 2-deoxy-D-glucose (FDG) since the tumor cells have increased glucose utilization [2,3,9].
Computerised Tomography (CT) and Magnetic Resonance Imaging (MRI)
CT and MRI are used to assess the salivary gland pathologies, adjacent normal structures, and the juxtaposition of salivary lesions to some of the vital structures like facial nerve, retromandibular vein, carotid artery, lymph nodes etc [2,3,9]. Computed tomography (CT) images are produced in all the 3 planes viz. Coronal, Sagittal and Axial. A reconstructed image can then be formed by a computerized analysis of the variance of absorption produced in all the three planes. This 3 dimensional imaging modality has been used for screening for recurrence and metastases, check for possible radiation-induced salivary gland dysfunction by demonstrating altered (decreased) volume and increased attenuation [10]. Indicated in differentiating cysts from solid masses and lipomas from other tumors, technique of choice to look for bony erosion caused by malignant lesions [9,11]. The Contrast Enhanced CT is indicated in staging of salivary gland tumors prior to treatment, evaluating treatment response, to assess the intra and extraglandular location, local extension/invasion into the surrounding tissues, detect regional lymph node metastases and systemic involvement [6].
The reported sensitivity of CT in detecting salivary gland lesions approached 75-100% and when combined with clinical information and laboratory findings, the overall specificity was 90% [11]. Magnetic Resonance Imaging (MRI) uses the erratic water content of body tissues to make a distinction between them. When exposed to a strong electromagnetic field, tissues absorb and then re-emit electromagnetic energy. An analysis of the net magnetization by radiofrequency is then reconstructed on computer software either as T1- or T2-weighted images, depending upon the rate constant with which magnetic polarization or relaxation occurs [6,11]. MRI is the modality of choice to evaluate minor salivary gland disease; perineural spread orbase of the skull. Involvement of malignant tumor of any salivary gland and deep lobe of parotid lesions for surgical assessment due to its excellent soft tissue contrast and ability to assess deep structures Disadvantages are it is expensive, not always available, contraindicated in the presence of Pacemakers and implanted metals, claustrophobia and long acquisition time [6].
CT scan and/ or MRI is useful for determining the outer extent of large tumors, any extra glandular extension, and the actual depth of such tumors. Additionally, they are helpful in distinguishing between 2 different tumors which are in close proximity to each another and for evaluation metastasis of cervical lymph nodes. CT-guided needle biopsy is useful to evaluate certain anatomically deep areas like the parapharyngeal space.
Gadolinium-enhanced dynamic MRI can be used to differentiate a benign tumor like pleomorphic adenoma from a malignant tumor by using peak time of enhancement. Similarly, heavy T2-weighted MRI scans can delineate Warthin tumor from pleomorphic adenoma based on signal strength.
MR Sialography
Advancements such as MR sialography, allows the visualization of the ductal system of the gland of interest without the injection of ductal/intravenous contrast agent with the help of highly fluidsensitive sequences, which is mostly performed in patients with acute sialadenitis. However, it has poor spatial resolution compared to the conventional sialography. The main hindrance to the usage of MR sialography is that it requires sufficient production of saliva and cannot be used otherwise [5].
CBCT
With further advancement of time, CBCT has replaced CT as the diagnostic modality of choice with advantages such as a relatively high spatial resolution of high-density structures such as bone, sialoliths with the added advantage of lower dose of radiation than conventional CT [6]. Though it useful in evaluating structures in and adjacent to salivary glands it cannot resolve differences in soft tissue densities. The mean effective dose in CT is 860 -1500|iSv and in CBCT is 68- 1073 |iSv, which clearly imparts the low radiation dose and also the cost effectiveness with better availability of CBCT imparts CBCT as a diagnostician's preferred choice of imaging modality [6,12]. Table 1 shows the various imaging modalities for salivary glands.
Conclusion
The realization and awareness of several imaging techniques has certainly evolved over time and the availability of these technologies helps in further increasing the understanding of the disease process and in drawing a conclusive diagnosis which is focused to draw a map towards the road leading to a successful treatment and a superior prognosis.
Table 1: Imaging Modalities for Salivary Glands.
References
- Taneja A, Sachdev IS, Sethi S, Garga UC (2015) Salivary gland imaging: A pictorial essay. Int J Med and Dent Sci 4(1): 692-700.
- Burket L, Greenberg M, Glick M, Ship J (2015) Burket's oral medicine 12th edn. Ont: BC Decker, Hamilton, USA, pp. 219-260.
- Dhameja M, Singla V, Dhameja K, Singla N (2016) Diagnostic imaging of the salivary glands- a review. International Journal of Contemporary Medicine Surgery and Radiology 1(1): 12-15.
- Karjodkar F (2013) Textbook of Dental and Maxillofacial Radiology, 2nd edn.
- Tassoker M, Ozcan S (2016) Contemporary Imaging of Salivary Glands. International Journal of Development Research 06(07): 8503-8507.
- Afzelius P, Nielsen MY, Ewertsen C, Klaus Poulsen Bloch (2014) Imaging of the major salivary glands. Clinical Physiology and Functional Imaging 36(1): 1-10.
- Thust SC, Smith RJP, Richards PS (2012) Salivary gland imaging. RAD Magazine 38(450): 37-38.
- Gritzmann N, Rettenbacher T, Hollerweger A, Macheiner P, Hubner E (2003) Sonography of the salivary glands. European radiology 13(5): 964-975.
- Taneja A, Sachdev IS, Sethi S, Garga UC (2015) Salivary gland imaging: A pictorial essay. Int J Med and Dent Sci 4(1): 692-700.
- Nabaa B, Takahashi K, Sasaki T, Okizaki A, Aburano T (2012) Assessment of salivary gland dysfunction after radioiodine therapy for thyroid carcinoma using non-contrast enhanced CT: the significance of changes of volume and attenuation of glands. AJNR Am J Neuroradiol 33(10): 1964-1970.
- Gopal S, Anusha V (2017) Salivary gland imaging- an overview. International Journal of Information Research and Review 04(09): 4481-4485.
- White SC, Pharoah MJ (2008) Oral Radiology, Principles and Interpretation. 6th edn.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...












