
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4692
Research Article(ISSN: 2637-4692) 
Multifactorial Analysis of Implant Removal - A Retrospective Cohort Study of 19 year data Volume 5 - Issue 4
Anastasiya Petrovska, Sameer Bajaj, Sakshi Kapoor, Yvonne L Kapila and Yogalakshmi Rajendran*
- Department of Orofacial Sciences, University of California San Francisco, USA
Received: November 21, 2022; Published: November 30, 2022
Corresponding author: Yogalakshmi Rajendran, BDS, MS, Director of Predoctoral Periodontics, Division of Periodontology, Department of Orofacial Sciences, University of California San Francisco, CA, USA. Box 0762.
DOI: 10.32474/MADOHC.2022.05.000220
Summary
a. What Is known: Studies have indicated that risk factors for developing peri-implant disease include a history of periodontal disease, poor oral hygiene, smoking, and diabetes.
b. There are other risk factors yet to be identified, which may cause peri-implant disease and implant loss.
What this study adds
a. This retrospective cohort study explored factors and diseases present at time of implant failure and determined that in addition to having a history of periodontal disease and non-compliance with maintenance recalls, there are high levels of systemic conditions, including cardiovascular disease, arthritis, osteoporosis, emotional disorders, and other systemic diseases present at time of implant loss.
Abstract
Background: Although frequently employed, dental implants may exhibit immediate or delayed complications that could lead to implant failure.
Purpose: The aim of this study was to explore the factors coincidental with removal of failed implants at a university-based periodontology specialty clinic by reviewing electronic health records (EHR) for the last 19 years.
Materials and methods: EHR data from Axium were searched for the dental code D6100 (implant removal) from January 2001 through April 2019. Patient and surgical data were gathered from dental records and analyzed.
Results: Analysis was performed on 73 patients who had a total of 96 implants removed. Of these, 59% of patients had periodontal disease, 32% were smokers. Amongst the medical conditions reviewed, 32% of patients reported cardiovascular disease, 23% had a bone disorder, and 18% had emotional disorders. In terms of the implants, 41 implants were placed in grafted bone: 54% being allograft. Out of 96 implants removed, 58 were late failures and 33 early failures. Forty-five percent of cases that had a late failure did not comply with regular recall and maintenance protocols.
Conclusion: Implant failure was coincidental with a history of periodontal disease and other risk factors, such as cardiovascular disease and emotional disorders. A lack of consistent maintenance recalls was frequently found in cases with late implant failure. This study highlights the need for a thorough and systematic evaluation of patients planning to receive implants.
Background
Dental implants are a successful treatment option for replacing missing teeth. It is estimated that every year, five million dental implants are placed in the United States. Dental implants treat edentulous spaces without damaging the adjacent teeth and restore patients’ chewing ability and esthetics. Implants are a great option for most patients, and they have a high success rate for treating failed teeth and edentulous areas [1]. High survival and success rates are reported in the literature, all ranging in the high 90 percent [2,3]. If compared to other alternative treatments, Fugazzotto et al. reported 97 - 98.6 % success rate for implants in molar sites, with the lowest success rate being that of second molar sites (85%) in comparison to root resection. Fixed partial dentures have a success rate of 93.67% over 6-7 years compared to single crown implants, which have a long-term success rate of 97.5% [4].
A major reason for the high success rates of dental implants is the biocompatibility of titanium fixtures with human bone and the ability of dental implants to Osseo integrate. The concept of osseointegration was first coined by Brandmark et al. and was described as bone-to-implant contact at the light microscopic level [5]. Albrektsson and Sennerby then defined osseointegration as “a direct functional and structural connection between living bone and the surface of a load carrying implant [6].” A histological connection between the new bone and the implant surface is established as early as 6 weeks and is 60% mature at three months [7]. If such healing is not successful, early implant failure occurs, even prior to an implant being restored and loaded. Similar to periodontal health, dental implant success relies on bone and soft tissue health. Peri-implant tissues are those that support the Osseo integrated implant-soft and hard tissue [8]. The American Academy of Periodontology defines two diseases that could affect implants, peri-implant mucositis and per-implantitis [9]. Peri-implant mucositis includes inflammation of the soft tissues surrounding a dental implant without additional bone loss after the initial bone remodeling. This disease is considered reversible with proper treatment [10,11]. Peri-implantitis is characterized by inflammation in the peri‐implant mucosa and subsequent progressive loss of supporting bone. This disease process could lead to implant failure and the need for implant removal. The increasing prevalence of peri-implantitis underscores the need to explore the risk factors associated with implant failure. Studies have reported several risk indicators for developing peri-implant disease: the most prevalent being a history of periodontal disease, poor oral hygiene, and smoking and diabetes [12]. The purpose of this retrospective study was to explore the factors coincidental with implant removal at the University of California San Francisco (UCSF) postgraduate periodontology clinic by reviewing the electronic health records (EHR) for the last 19 years.
Methods
This study was reviewed and approved by the UCSF Institutional Review Board (Approval # ID- 17-22729). The study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013. Electronic health records from the school’s dental database (Axium software, Dentrix) were accessed for current dental terminology (CDT) codes D6100 (implant removal) and D7140 (simple tooth extraction) from January 2001 to April 2019. Data were collected from patients who had one or more implant removed in the post-graduate and faculty periodontal clinics, regardless of whether or not the implant was originally placed at UCSF. Exclusion criteria included incomplete or non-accessible data. Data, including age at the time of removal, gender, and all available medical, dental, and social history were collected from patients’ records. The history of periodontal disease was determined based on previous non-surgical and surgical periodontal treatment. In addition, surgery and implant details, follow-up, and maintenance schedules were obtained from the electronic dental records where available. Basic statistical analyses were performed on the collected data. Specifically descriptive statistics, such as frequencies and percentages were used to describe the findings. This study complied with the STROBE checklist for Cohort studies. The data used to support the findings of this study are restricted to protect PATIENT PRIVACY. Data are available upon request from UCSF IRB – irb@ucsf.edu for researchers who meet the criteria for access to confidential data.
Results
Patient demographics and implant failures
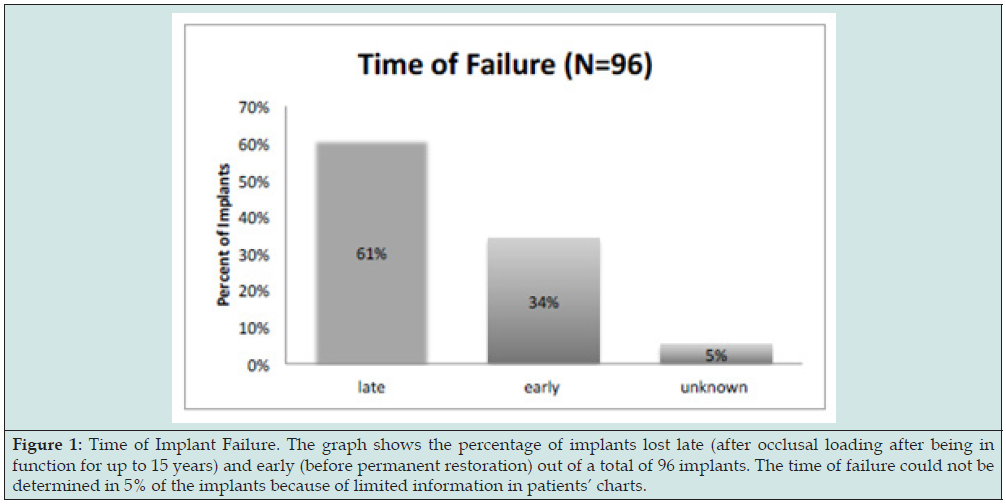
The search and review of the records resulted in the selection of 87 patients who had a total of 114 implants removed. In addition, 15 patients were excluded based on incomplete data. Also, two implants were incorrectly classified as simple tooth extractions in one patient. Therefore, the statistical analysis was performed on data from 73 patients and 96 implants. The youngest patient who had an implant removed was 28 and the oldest 88 years old, with an average age of 62 years old at the time of implant removal. Thirtyeight male patients, 34 female patients, and one transgender patient were included in the analysis (Table 1). Sixteen patients experienced multiple implant failures; the highest number of implants removed was five in one patient, but two of the implants were repeat failures in the same sites. Fifty-seven patients had one implant removed during the investigation time frame. Fifty patients had implants placed at UCSF, and 46 were placed in outside clinics. Out of 96 implants, 58 (61%) were restored and had one to fifteen years of service before failure. 33 (34%) exhibited early failure (Figure 1). For 5 (5%) implants it was unclear whether they were restored at the time of failure. Four early-failure implants developed a buccal fistula and radiolucency a few weeks following placement, two of which report previous endodontic infection on the site (Table 2). The rest of the implants had inadequate osseointegration prior to or at second-stage surgery. Late failures were primarily associated with advanced peri-implant disease (54/58), implant fracture (2/58), periapical abscess and pain (2/58).
Figure 1: Time of Implant Failure. The graph shows the percentage of implants lost late (after occlusal loading after being in function for up to 15 years) and early (before permanent restoration) out of a total of 96 implants. The time of failure could not be determined in 5% of the implants because of limited information in patients’ charts.
Medical and social history
Amongst the medical conditions reviewed, the most prominent was a history of cardiovascular disease at 32%. Bone disease was reported in 23% of patients; one patient reported taking an oral bisphosphonate for osteoporosis (Figure 2a). Eighteen percent of patients were presented with emotional disorders, such as depression, anxiety, and post-traumatic stress disorder. Sixteen percent of patients reported having acid reflux or gastroesophageal reflux disease (GERD), and 15% had a respiratory condition, such as asthma, chronic obstructive pulmonary disease (COPD), or emphysema. Eight patients had a history of cancer and 7 patients reported a viral infectious disease (human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) or hepatitis B).
Figure 2A: Presence of Systemic Disease. The graph shows the percentage of patients with Cardiovascular disease, Arthritis + Osteoporosis, Emotional disorder, Respiratory disease, Diabetes, History of Cancer and Infectious disease. Medical history could not be determined for 18% of the patients because of limited information in patients’ charts.
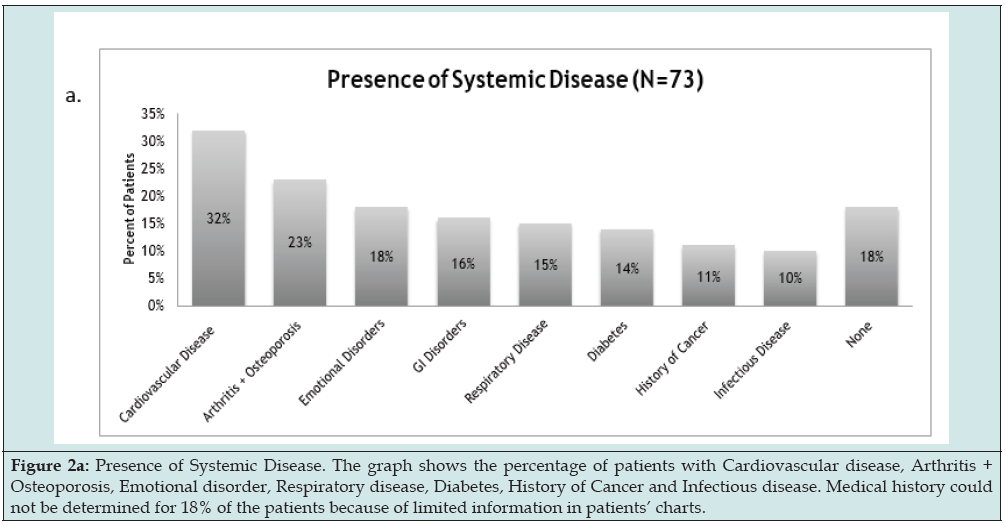
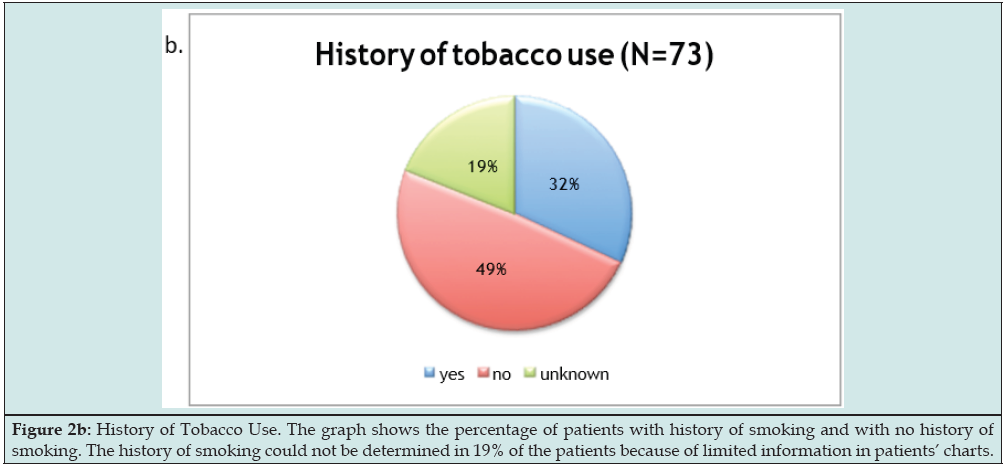
Fourteen percent of patients were presented with a diagnosis of diabetes. One patient had Type 1 diabetes and the remaining patients had Type 2. Patients reported taking medications for their diabetes and were determined to have normal or stable HbA1c measurements as recorded in their electronic dental records. Thirty-two percent of patients reported using tobacco products currently or in the past (Figure 2b). However, it was not possible to determine the breakdown of products used. Thirteen patients had no significant medical or social history.
Figure 2B: History of Tobacco Use. The graph shows the percentage of patients with history of smoking and with no history of smoking. The history of smoking could not be determined in 19% of the patients because of limited information in patients’ charts.
Dental history
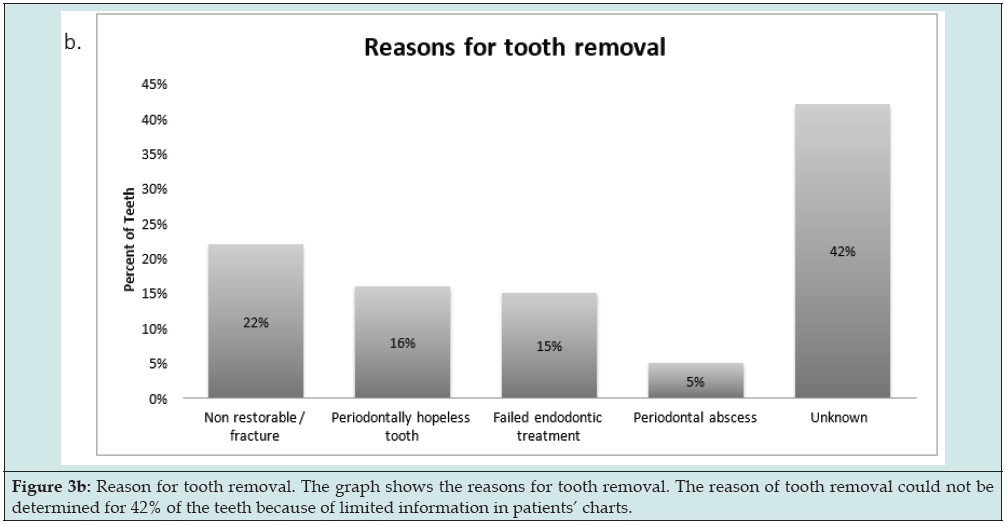
A history of periodontal disease was present in 59% of patients based on a recorded history of surgical or non-surgical periodontal treatment (Figure 3a). Oral habits and occlusal schemes were not clearly reported in the electronic dental records. Examination of the reason for tooth removal at sites where implants failed revealed that 5 (15%) teeth had endodontic treatment and 3 out of these 5 (5%) had periapical abscesses (Figure 3b). Also, teeth were removed due to severe periodontal disease and unrestorable conditions.
Figure 3A: History of Periodontal Disease. The graph shows the percentage of patients with history of periodontal disease and with no history of periodontal disease. The history of periodontal disease could not be determined in 16% of the patients because of limited information in patients’ charts.
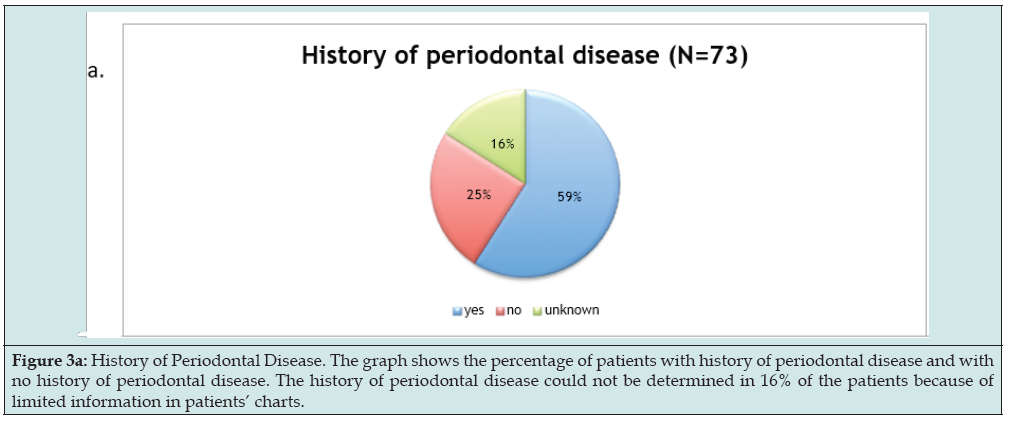
Figure 3B: Reason for tooth removal. The graph shows the reasons for tooth removal. The reason of tooth removal could not be determined for 42% of the teeth because of limited information in patients’ charts.
Surgery and maintenance
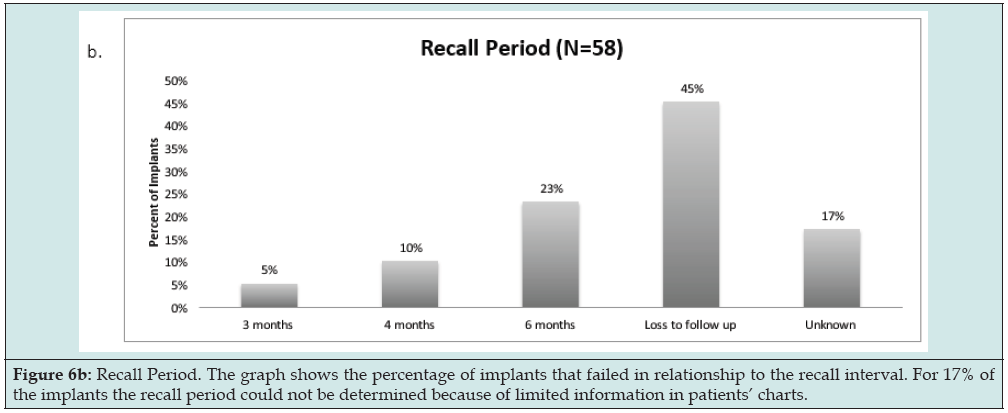
It was determined that 41 (43%) failed implants were placed in grafted bone and underwent either ridge preservation, guided tissue regeneration, sinus augmentation, simultaneous augmentation or a combination thereof (Figure 4a). The majority of cases (54%) used particulate allograft for bone augmentation (Figure 4b). Other cases used a mixture of allograft and autogenous graft, or allograft and xenograft, 12% and 10% respectively. Other materials were used to a lesser extent. Various implant systems were represented in the failed implants. The highest number of failed implants were Nobel BioCare (31%) followed by unknown types (30%) (Figure 5). Unfortunately, occlusion, types of restorations, and parafunctional habits were not sufficiently discussed in patients’ records for analysis. Periodontal maintenance was reported for 38% patients, whereas 45% documented no regular maintenance (Figure 6a). Seventeen percent of patients’ charts did not report if maintenance was performed. Of those in maintenance, 23% were on a 6 month recall, 10% on a 4 month recall, and 5% on a 3 month recall (Figure 6b).
Figure 4A: Implants placed in grafted bone. The graph shows the percentage of failed implants placed in grafted bone versus native bone. In 48% of the patients if bone grafting was done prior to implant placement could not be determined because of limited information in patients’ charts.
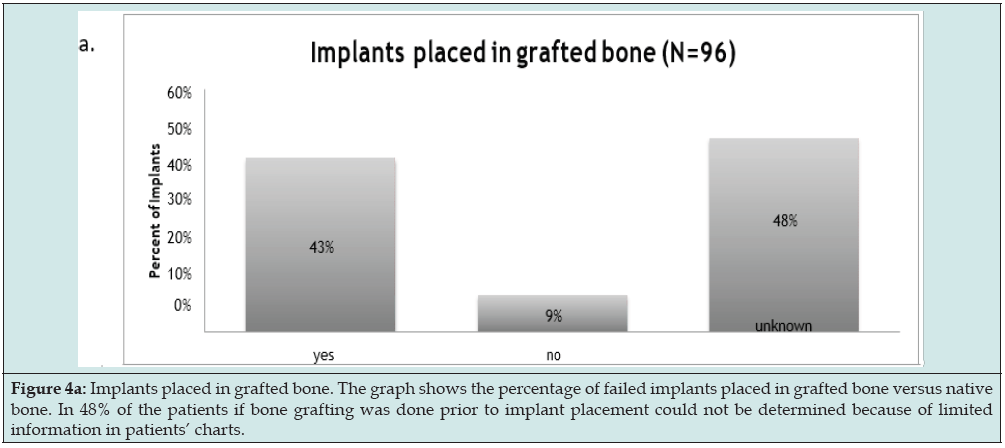
Figure 4B: Bone Graft Material. The graph shows the percentage of failed implants in relation to the different bone graft materials. In 12% of the implants the graft material used could not be determined because of limited information in patients’ charts.
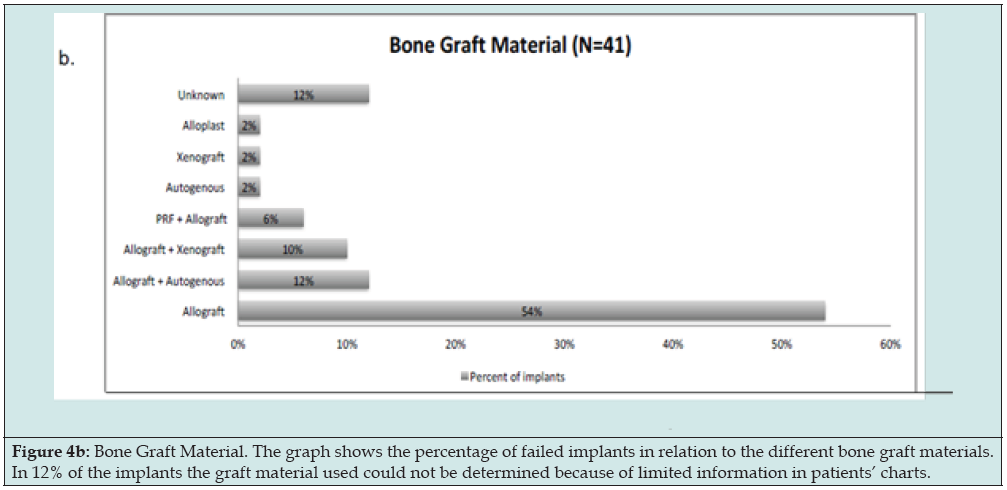
Figure 5: Implant Company. The graph shows the percentage of implants failed in relationship to the type of implant. For 30% of the implants, the implant type could not be determined because of limited information in patients’ charts.
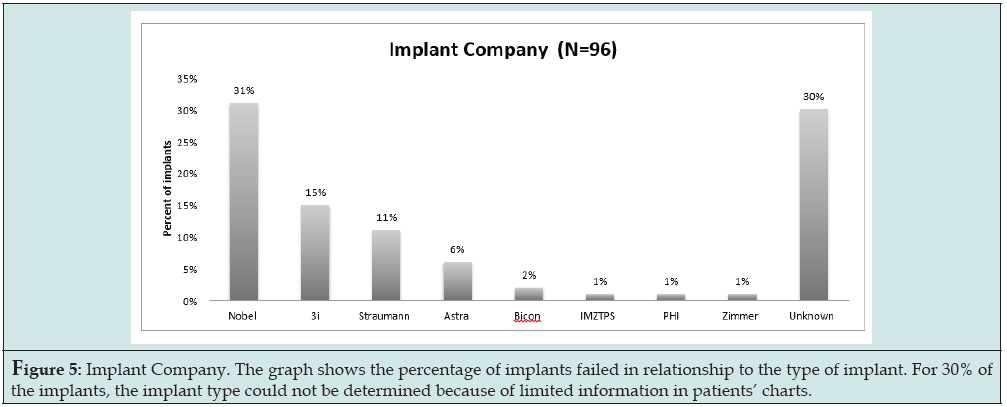
Figure 6A: Implant Maintenance for late failures. The graph shows the percentage of implants removed due to late failure in relationship to implant maintenance. The implant maintenance could not be determined for 17% of the implants because of limited information in patients’ charts.
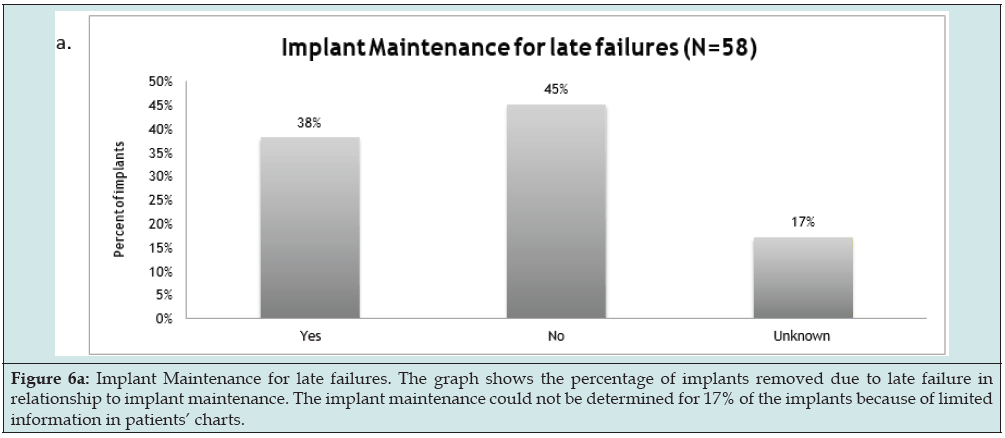
Figure 6B: Recall Period. The graph shows the percentage of implants that failed in relationship to the recall interval. For 17% of the implants the recall period could not be determined because of limited information in patients’ charts.
Discussion
Implant failure could be the result of biological or mechanical complications and lead to removal of the fixtures, often leaving the patient in a more compromised position for reconstruction than when they started. The clinician needs to systematically evaluate the patient for the risk of developing such complications and inform the patient of all the risks associated with implant treatment. Therefore, this retrospective study attempted to identify comorbidities in patients that lost implants due to such complications. Patient charts and radiographs were examined for the etiology of the failure. Most cases are presented with signs of biological complications- bleeding on probing, erythema, deep pocketing, and radiographic bone loss. Peri-implantitis is characterized by inflammation in peri- implant connective tissue and progressive loss of supporting bone [13]. In this study, peri-implantitis was the presumed leading cause of implant removal and, therefore, was used as a surrogate for implant removal in our study for discussion purposes where applicable.
Demographics
The patients included in this study were patients of record at the UCSF Dental Center who had one or more implants removed due to various reasons. Thirty- eight patients were males, 34 were females and 1 transgender (patient on hormonal therapy). Sixteen patients had multiple implants removed, 68% of which were male patients. This compares to a retrospective study in which male gender had a higher association with peri - implant disease [14]. However, another study showed no significant association between age, gender, and peri - implant disease [15]. The same study showed that older patients also had more systemic diseases, polypharmacy, and a higher prevalence of periodontal disease, which could contribute to a higher failure of dental implants. In our study, the majority of the patients who had to undergo explanation were over 50 years of age. This agrees with a report showing a higher prevalence of implant failures in older populations; especially late implant failure in men [16]. Nevertheless, implant failure is a multifactorial disease, and various contributing factors should be considered besides gender.
Medical Conditions
Cardiovascular disease
In the population examined in this study, 32% of patients had cardiovascular disease, including ischemic heart disease, stroke, and hypertensive heart disease. According to the WHO, cardiovascular disease is one of the most common chronic conditions in the aging population [17], therefore our patient population is consistent with this report on world norms. A retrospective study by Revert showed an association of cardiovascular disease with peri - implantitis, reporting the highest odds ratio (11.9) between diagnosis of peri – implantitis and a history of cardiovascular disease.15 However, a cohort study by Wu found a decreased failure rate of dental implants in patients who used antihypertensive drugs (0.6%) compared to 4.1% of nonusers [18]. They concluded that various classes of antihypertensive drugs have positive effects on bone remodeling and formation. More studies are needed to evaluate the effect of cardiovascular disease on the rate of implant failure.
Bone disorders
Bone related ailments, such as osteoarthritis, osteoporosis and osteopenia were reported in 23% of patients in this study. In a cross-sectional study, Dvorak et al., did not find a statistically significant association between peri - implantitis or implant loss and diagnosis of osteoporosis or osteopenia [19]. However, in a retrospective study, Alsaadi et al. found an association between osteoporosis and early implant failure (up to abutment connection) [20]. A consensus report that used a meta-analysis to evaluate the effect of systemic disease on implant survival post loading, found that patients that received low- dose antiresorptive therapy for osteoporosis and osteoarthritis had comparatively high implant survival rates [21]. However, patients that received high dose anti-antiresorptive therapy for metastatic cancer treatment and osteoporosis had increased rates of complications. Bisphosphonates that were administered intravenously for metastatic cancer patients, increased the risk of osteonecrosis of the jaw due to their long-lasting inhibitory effects on osteoclast activity [22].
Cancer
In its various forms, cancer was reported in 11% of our patient population. Records were not sufficient to determine the exact timing of cancer diagnosis and treatment in relation to dental implant procedures. Nevertheless, patients reported chemotherapy and/or radiation therapy as part of their cancer treatment. There is strong evidence showing that head and neck radiation negatively impacts dental implant treatment [23]. Radiation decreases bone remodeling potential and decreases the blood supply to the remodeling bone; both of which can lead to complications if dental surgery is performed [24]. Due to the increased risk of implant failure and osteonecrosis of the jaw, dental implants are contraindicated for such patients. However, with improvements in cancer treatment, the dosage and scatter of radiation can be decreased, thereby having a more positive effect on post- radiation healing potential. A meta-analysis showed an 83% survival rate for implants placed in radiated bone [25].
Emotional Disorders
Eighteen percent of the studied population reported an emotional disorder, such as anxiety, depression, or post - traumatic stress disorder. The electronic dental records also indicated the use of medications to treat these conditions, such as selective serotonin reuptake inhibitors (SSRIs). In addition to their desired effects, SSRIs can also reduce bone remodeling and increase the risk of bone fractures by influencing signaling pathways in osteoblasts and osteoclasts [26]. In a cohort study of 490 patients, a higher risk of late implant failure was reported in SSRI users compared to nonusers [27]. A systematic review completed for the ITI Consensus Meeting reported a significantly higher implant failure rate for SSRI users and proton pump inhibitor (PPI) users [28]. Taken in aggregate, these data indicate that SSRIs and PPIs could be associated with medication - related implant failures.
Gastrointestinal acid related conditions
Conditions such as peptic ulcers, gastroesophageal reflux disease, or acid reflux were recorded in 16% of the patient population in the current study. A common class of medications for such conditions are PPIs, which, in addition to modulating gastric acidity, also influence bone metabolism. This class of medications inhibits the H/K ATPase pump, which is present both in the GI tract and bone osteoclasts. In bone osteoclasts, PPIs reduce osteoclast remodeling potential [29]. Implant survival depends on bone metabolism, so PPIs have been investigated as a risk indicator for peri - implant disease. In a cohort study of PPI users and non-users, Wu et al. followed 799 patients who had dental implants placed. Subjects using PPIs had higher failure rates (6.8%) compared to non-users (3.2%), primarily 10-20 months after implant placement [30]. Published data support that PPIs influence bone remodeling, and therefore, PPIs may have adverse effects on implant osseointegration [31].
Diabetes
Ten out of 73 (14%) patients in this study had diabetes, which is higher than the global prevalence of 8.8% [32]. HbA1c values were not available for all patients; however, this is a critical value that can show the level of control of the disease. Monje et al. conducted a systematic review and meta-analysis aimed at investigating the association of hyperglycemia to peri - implant disease [33]. This meta- analysis of 7 studies revealed that the risk of peri - implantitis was 50% higher in patients with diabetes (of any severity and with hemoglobin HbA1c levels above 5.7%), compared to healthy controls. In patients with diabetes, the chronic inflammatory state and decreased repair and wound healing of periodontal tissues could adversely affect the health of peri - implant tissues. However, with good glycemic control, osseointegration of dental implants is possible, and implant treatment can have comparable success rates as that in healthy patients [34,35].
Smoking
Thirty-two percent of the patients in this study were smokers or had a history of using tobacco. The specific form, quantity, and duration of tobacco product usage was not analyzed in this study, due to limited information recorded in the patient records. Previous studies indicate a significant deleterious impact of smoking on implant health [36]. Smoking is believed to have a negative effect on new bone formation by reducing calcium absorption and impairing wound healing through direct toxic effects [37]. In a cross - sectional study of 119 subjects, a high association between implant loss and smoking was reported [38]. Although, a majority of current studies do not report strong evidence to classify smoking as a risk factor for peri - implantitis (9); additional long-term studies are needed to shed more light on this topic.
Periodontal disease
A history of periodontal disease is one of the main risk indicators for peri - implant disease and subsequent implant failure (9). Periodontitis occurs in roughly 50% of the adult population in the United States [39]. This number is in agreement with the results of the current study, wherein 59% of patients had a history of periodontal treatment and / or had active periodontal disease. A ten - year prospective cohort study by Karoussis et al showed that a history of periodontal disease is associated with lower survival rates for dental implants - 90.5% survival for periodontitis patients versus 96.5% for patients with no history of periodontal disease [40]. Periodontitis is a bacterial infection, and peri- implant disease shares a common etiology. Bacteria originating from teeth with periodontal disease can infect dental implants, which is important in partially edentulous patients that have remaining deep pockets [41]. Implants placed in patients with poorly controlled periodontal disease show higher odds for developing peri – implantitis; from an odds ratio of 5 [42] to an odds ratio of 6.14 Periodontal disease needs to be properly treated and stabilized in order to reduce the risk of peri-implant disease, which could lead to implant failure [43].
Infected recipient site
Our study found that 6 fixtures were removed from previously failed endodontic sites with noted periapical radiolucencies. A histopathologic study on 154 alveolar bone specimens discovered that bacteria could remain encapsulated in the edentulous alveolar ridge for 1 year or more after extraction and mucosal healing [44]. These encapsulated bacteria could trigger an infection around the apical portion of the implant [45]. Residual infection could present as retrograde peri - implantitis (RPI), described as a symptomatic periapical lesion with no bone loss or signs of inflammation around the coronal portion of the implant [46]. Placement of implants in previously infected sites could contribute to implant failure [47]. In contrast, there are several systematic reviews suggesting that immediate implants can be placed in sites having a prior history of periapical lesions with comparable results to those placed in healthy edentulous sites [48,49].
Bone augmentation
Bone augmentation and ridge regeneration are essential components of modern implant dentistry. In this study, out of 96 implants, at least 46 (42.7%) needed augmentation, prior to and/ or during implant placement. Various materials and combinations were used; the most common being allograft (54%). Mixtures of allograft with autogenous bone (12%) and with xenograft (10%) were also utilized. Literature strongly supports the benefits of and the necessity for grafting and shows comparable survival rates for implants placed in regenerated versus native bone [50,51]. A review article by Jensen et al. indicates high survival rates for implants placed at sites with horizontal ridge augmentation (97 - 100%), vertical ridge augmentation (95 -100%), and maxillary sinus floor elevation (61.2-100%) [52]. However, the follow-up period in this study was fairly short- 12 months after loading. Some studies suggest that bone augmentation lowers the risk of developing peri - implant disease because implants can be placed in a favorable position in ample amounts of bone [53,54]. On the other hand, there are reports that show a weak association between previous ridge augmentation and peri - implant disease after an 8-year follow (P=0.617).55 Long-term follow up studies on grafting outcomes would be beneficial.
Early vs late failures
Implant failure can be divided into two categories: early failure (before abutment connection), and late failure (after occlusal loading). In the current study, out of 96 implants, 34% implants failed prior to placement of the permanent restoration, and 61% failed after being in function for up to 15 years. The time of failure could not be determined in 5% of the implants because of limited information in patients’ charts. Previous studies also reported a greater percentage of late implant loss compared to early implant loss. In a systematic review, Berglundh, et al. determined that early implant loss comprised 0.76-7.47% of the cases and late implant loss comprised 2.1 - 11.3% of the cases [3]. Some of the proposed contributory factors in early implant failure include surgical technique, postoperative infection, and inadequate adjustment of prosthetic appliances that can lead to overloading of the fixture and prevention of proper healing [47]. Late failures are associated with peri - implant disease as demonstrated by radiographic bone loss, bleeding on probing, and deepening pocket depths.9 Mechanical failures are also noted, such as restoration or implant fracture [47].
Occlusion
Although occlusion and patient habits, such as bruxism, have been discussed in only a few cases, they are important factors to consider [55,56]. Manor et al’s review found that improper functional balance was the leading cause of late implant failure [16]. Stress concentrations from off axial loading also result in marginal bone loss.56 Multiple investigations showed that long cantilevers or parafunctional habits cause significant bone remodeling around dental implants [57]. Further, marginal bone loss can cause deepening of pockets around implants and increase the bacterial load, which can lead to significant peri- implant disease and eventual implant failure [58]. Advances in implant dentistry allow placement of tilted implants to avoid vital structures, for additional augmentation procedures, and to potentially increase anteriorposterior spread of the restoration. However, such implants are then loaded off axis, potentially concentrating the stress on the implant [59]. A meta-analysis on 7,568 implants failed to show a difference in survival rates and marginal bone loss between straight and tilted implants, but there were limitations in the studies, including a fairly short follow up of 3 years and a high bias was noted. Nevertheless, the review discussed the influence of the angle of the tilt on increasing marginal bone loss. A proper restorative design and loading should be accounted for when planning implant placement.
Maintenance
One of the main considerations in dental health is personal oral hygiene. Implant health is especially dependent on adherence to good oral health. Studies show that patients with poor oral hygiene are more prone to both periodontal and peri – implant disease and complications [60]. Peri- implant mucositis is more likely to progress to peri – implantitis in patients who do not practice proper preventative maintenance [61]. Peri- implantitis occurs less in patients who comply with maintenance therapy; odds ratio of 0.14 [62]. A cross sectional analysis by Schwarz et al found that high plaque levels were significantly correlated with peri-implantitis; odd radio 9.2 [13]. Therefore, regular self and professional maintenance is the key to success for peri- implant health [9].
Conclusion
Comprehensive individual risk assessments should be implemented and discussed with each patient planned for implant therapy. Implant failure is multifactorial and highly coincidental with the presence of periodontal disease and other factors, such as bone disorders and cardiovascular disease, and the use of specific medications. Occlusion is an important factor that needs to be considered in failing implants. This area needs to be further explored to determine a potential causal relationship. A holistic approach, which includes careful analysis of systemic conditions, emotional disorders, smoking, and endodontic history, should be practiced.
Acknowledgement
We acknowledge and thank Haripriya Padma, DDS and Mohammed Feizizad, DSS who helped with data extraction pertaining to implant explanation that were misclassified. This manuscript has already been submitted as a master’s thesis project [63].
References
- Pjetursson, Bjarni E, et al. (2004) A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years: I. Implant‐supported FPDs. Clinical oral implants research 15(6): 625-642.
- Moraschini V (2015) Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. International journal of oral and maxillofacial surgery 44(3): 377-388.
- Berglundh Tord, Leif Persson, Björn Klinge (2002) A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. Journal of clinical periodontology 29: 197-212.
- Fugazzotto Paul A (2001) A comparison of the success of root resected molars and molar position implants in function in a private practice: results of up to 15‐plus years. Journal of periodontology 72(8): 1113-1123.
- Brånemark PI (1969) Intra-osseous anchorage of dental prostheses: I. Experimental studies. Scandinavian journal of plastic and reconstructive surgery 3(2): 81-100.
- Albrektsson Tomas, Lars Sennerby (1991) State of the art in oral implants. Journal of clinical periodontology 18(6): 474-481.
- Berglundh Tord (2003) De novo alveolar bone formation adjacent to end osseous implants: a model study in the dog. Clinical oral implants research 14(3): 251-262.
- Karoussis Ioannis K, Sotirios Kotsovilis, Ioannis Fourmousis (2007) A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients. Clinical oral implants research 18(6): 669-679.
- Schwarz Frank (2018) Peri‐implantitis. Journal of clinical periodontology 45: S246-S266.
- Salvi Giovanni E (2012) Reversibility of experimental peri‐implant mucositis compared with experimental gingivitis in humans. Clinical oral implants research 23(2): 182-190.
- Meyer, Simon (2017) Experimental mucositis and experimental gingivitis in persons aged 70 or over. Clinical and biological responses. Clinical oral implants research 28(8): 1005-1012.
- Heitz‐Mayfield, Lisa JA (2008) Peri‐implant diseases: diagnosis and risk indicators. Journal of clinical periodontology 35: 292-304.
- Schwarz, Frank (2017) The prevalence of peri‐implant diseases for two‐piece implants with an internal tube‐in‐tube connection: a cross‐sectional analysis of 512 implants. Clinical oral implants research 28(1): 24-28.
- Koldsland, Odd Carsten, Anne Aamdal Scheie, Anne Merete Aass (2011) The association between selected risk indicators and severity of peri‐implantitis using mixed model analyses. Journal of clinical periodontology 38(3): 285-292.
- Renvert, Stefan (2014) Factors related to peri‐implantitis–a retrospective study. Clinical oral implants research 25(4): 522-529.
- Manor, Yifat (2009) Characteristics of early versus late implant failure: a retrospective study. Journal of Oral and Maxillofacial Surgery 67(12): 2649-2652.
- (2015) World Health Organization. World report on ageing and health.
- Wu, Xixi (2016) Antihypertensive medications and the survival rate of osseointegrated dental implants: a cohort study. Clinical implant dentistry and related research 18(6): 1171-1182.
- Dvorak, Gabriella (2011) Peri‐implantitis and late implant failures in postmenopausal women: a cross‐sectional study. Journal of clinical periodontology 38(10): 950-955.
- Alsaadi, Ghada (2007) Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection. Journal of clinical periodontology 34(7): 610-617.
- Schimmel, Martin (2018) Effect of advanced age and/or systemic medical conditions on dental implant survival: A systematic review and meta‐analysis. Clinical oral implants research 29: 311-330.
- Ruggiero, Salvatore L, (2009) American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws-2009 update. Journal of Oral and Maxillofacial Surgery 67(5): 2-12.
- Ihde, Stefan (2009) Effects of radiation therapy on craniofacial and dental implants: a review of the literature. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 107(1): 56-65.
- Tanaka, Takako Imai (2013) Updated clinical considerations for dental implant therapy in irradiated head and neck cancer patients. Journal of Prosthodontics 22(6): 432-438.
- Schiegnitz E (2014) Oral rehabilitation with dental implants in irradiated patients: a meta-analysis on implant survival. Clinical oral investigations 18(3): 687-698.
- Tsapakis EM, (2012) The adverse skeletal effects of selective serotonin reuptake inhibitors. European psychiatry 27(3): 156-169.
- Wu X (2014) Selective serotonin reuptake inhibitors and the risk of osseointegrated implant failure: a cohort study. Journal of dental research 93(11): 1054-1061.
- Jung Ronald E (2018) Group 1 ITI Consensus Report: The influence of implant length and design and medications on clinical and patient‐reported outcomes. Clinical oral implants research 29: 69-77.
- Ngamruengphong, Saowanee, (2011) Proton pump inhibitors and risk of fracture: a systematic review and meta-analysis of observational studies. American Journal of Gastroenterology106(7) 1209-1218.
- Wu, Xixi (2017) Proton pump inhibitors and the risk of osseointegrated dental implant failure: a cohort study. Clinical implant dentistry and related research 19(2): 222-232.
- Alexandru Mester, Dragos Apostu, Lidia Ciobanu, Andra Piciu, Ondine Lucaciu, et al. (2019) The impact of proton pump inhibitors on bone regeneration and implant osseointegration. Drug metabolism reviews 51(3): 330-339.
- K Ogurtsova, J D da Rocha Fernandes, Y Huang, U Linnenkamp, L Guariguata, et al. (2017) IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes research and clinical practice 128(1): 40-50.
- Monje Alberto, Andres Catena, Wenche S Borgnakke (2017) Association between diabetes mellitus/hyperglycaemia and peri‐implant diseases: Systematic review and meta‐analysis. Journal of clinical periodontology 44(6): 636-648.
- Javed Fawad, George E Romanos (2009) Impact of diabetes mellitus and glycemic control on the osseointegration of dental implants: a systematic literature review. Journal of periodontology 80(11): 1719-1730.
- Chrcanovic BR, Tomas Albrektsson, Ann Wennerberg (2014) Diabetes and oral implant failure: a systematic review. Journal of dental research 93(9): 859-867.
- Wallace Robert H (2000) The relationship between cigarette smoking and dental implant failure. The European journal of prosthodontics and restorative dentistry 8(3): 103-106.
- Riebel Gregory D, S D Boden, T E Whitesides, W C Hutton (1995) The effect of nicotine on incorporation of cancellous bone graft in an animal model. Spine 20(20): 2198-2202.
- Koldsland, Odd Carsten, Anne Aamdal Scheie, Anne Merete Aass (2009) Prevalence of implant loss and the influence of associated factors. Journal of periodontology 80(7): 1069-1075.
- Eke, Paul I, Bruce A Dye, Liang Wei, Gary D Slade, Gina O Thornton Evans, et al. (2015) Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. Journal of periodontology 86(5): 611-622.
- Karoussis Ioannis K, Giovanni E Salvi, Lisa J A Heitz Mayfield, Urs Brägger, Christoph H F Hämmerle, et al. (2003) Long‐term implant prognosis in patients with and without a history of chronic periodontitis: a 10‐year prospective cohort study of the ITI Dental Implant System. Clinical oral implants research 14(3): 329-339.
- Mombelli A, M A van Oosten, E Schurch Jr, N P Land (1987) The microbiota associated with successful or failing osseointegrated titanium implants. Oral microbiology and immunology 2(4): 145-151.
- Roos Jansåker Ann Marie, Christel Lindahl, Helena Renvert, Stefan Renvert (2006) Nine‐to fourteen‐year follow‐up of implant treatment. Part I: implant loss and associations to various factors. Journal of clinical periodontology 33(4): 283-289.
- Mombelli Andrea, Niklaus P Lang (1998) The diagnosis and treatment of peri‐implantitis. Periodontology 2000 17(1): 63-76.
- Kassolis James D, Mark Scheper, Bruno Jham, Mark A Reynolds (2010) Histopathologic findings in bone from edentulous alveolar ridges: a role in osteonecrosis of the jaws?. Bone 47(1): 127-130.
- McAllister BS, D Masters, RM Meffert (1992) Treatment of implants demonstrating periapical radiolucencies. Practical periodontics and aesthetic dentistry: PPAD 4(9): 37-41.
- Quirynen Marc, Frieda Gijbels, Reinhilde Jacobs (2003) An infected jawbone site compromising successful osseointegration. Periodontology 2000 33(1): 129-144.
- Esposito Marco, J M Hirsch, U Lekholm, P Thomsen (1998) Biological factors contributing to failures of osseointegrated oral implants. (II). Etiopathogenesis. European journal of oral sciences 106(3): 721-764.
- Crespi Roberto, Paolo Capparè, Enrico Gherlone (2010) A 4‐year evaluation of the peri‐implant parameters of immediately loaded implants placed in fresh extraction sockets. Journal of periodontology 81(11): 1629-1634.
- Chrcanovic Bruno Ramos, Maximiliano Delany Martins, Ann Wennerberg (2015) Immediate placement of implants into infected sites: a systematic review. Clinical implant dentistry and related research 17(Suppl 1): e1-e16.
- Hämmerle Christoph HF, Ronald E Jung, Andreas Feloutzis (2002) A systematic review of the survival of implants in bone sites augmented with barrier membranes (guided bone regeneration) in partially edentulous patients. Journal of clinical periodontology 29(Suppl 3): 226-231.
- Chiapasco, Matteo, Paolo Casentini, Marco Zaniboni (2009) Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implants 24(Suppl): 237-259.
- Jensen S Storgard, Hendrik Terheyden (2009) Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone-substitute materials. Int J Oral Maxillofac Implants 24(Suppl): 218-236.
- Konstantinidis Ioannis K, Georgios A Kotsakis, Sebastian Gerdes, Michael Horst Walter (2015) Cross-sectional study on the prevalence and risk indicators of peri-implant diseases. Eur J Oral Implantol 8(1): 75-88.
- Poli Pier Paolo, Mario Beretta, Giovanni Battista Grossi, Carlo Maiorana (2016) Risk indicators related to peri-implant disease: an observational retrospective cohort study. Journal of periodontal & implant science 46(4): 266-276.
- Busenlechner Dieter, Rudolf Fürhauser, Robert Haas, Georg Watzek, Georg Mailath, et al. (2014) Long-term implant success at the Academy for Oral Implantology: 8-year follow-up and risk factor analysis. Journal of periodontal & implant science 44(3): 102-108.
- Van Steenberghe Daniel, I Naert, R Jacobs, M Quirynen (1999) Influence of inflammatory reactions vs. occlusal loading on peri-implant marginal bone level. Advances in dental research 13(1): 130-135.
- Lindquist Lars W, Birger Rockler, Gunnar E Carlsson (1988) Bone resorption around fixtures in edentulous patients treated with mandibular fixed tissue-integrated prostheses. The Journal of prosthetic dentistry 59(1): 59-63.
- Kozlovsky Avital, Haim Tal, Ben Zion Laufer, Roy Leshem, Michael D Rohrer, et al. (2007) Impact of implant overloading on the peri‐implant bone in inflamed and non‐inflamed peri‐implant mucosa. Clinical oral implants research 18(5): 601-610.
- Lan Ting Hsun, Chin Yun Pan, Huey Er Lee, Heng Li Huang, Chau Hsiang Wang (2010) Bone stress analysis of various angulations of mesiodistal implants with splinted crowns in the posterior mandible: a three-dimensional finite element study. International Journal of Oral & Maxillofacial Implants 25(4): 763-770.
- Roccuzzo Mario, Nicola De Angelis, Luca Bonino, Marco Aglietta (2010) Ten‐year results of a three‐arm prospective cohort study on implants in periodontally compromised patients. Part 1: implant loss and radiographic bone loss. Clinical Oral Implants Research 21(5): 490-496.
- Costa Fernando Oliveira, Satoshi Takenaka Martinez, Luís Otávio Miranda Cota, Sergio Diniz Ferreira, Geraldo Lúcio Magalhães Silva, et al. (2012) Peri‐implant disease in subjects with and without preventive maintenance: a 5‐year follow‐up. Journal of clinical periodontology 39(2): 173-181.
- Monje Alberto, Hom Lay Wang, José Nart (2017) Association of preventive maintenance therapy compliance and peri‐implant diseases: a cross‐sectional study. Journal of periodontology 88(10): 1030-1041.
- Petrovska A (2020) Multifactorial Analysis of Implant Removal - A Retrospective Study of 19-year data. University of California San Francisco, United States.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...






