
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4692
Case Report(ISSN: 2637-4692) 
Management of Periodontal Health in Pediatrics Patients: Series of Cases Volume 4 - Issue 2
Sumit Munjal1* and Seema Munjal2
- 1Department of Periodontics, Institute of Dental Studies & Technologies, India
- 2Department of Prosthodontics and crown & bridge, Faces N Braces Dental Research Centre, India
Received:December 16, 2019; Published: January 07, 2020
Corresponding author:Sumit Munjal, Department of Periodontics, Institute of Dental Studies & Technologies, Uttar Pradesh, India
DOI: 10.32474/MADOHC.2020.04.000182
Abstract
The effects of periodontal disease observed in adults have their inception earlier in life and are often associated with systemic metabolic patterns, thus the diagnosis is significant. Moreover, surgical corrections are increasingly sought for since the parents are more concerned about aesthetics than ever before. This paper reviews the more common oral conditions involving periodontal health in children and adolescents and discusses the roles of paediatric dentistry and periodontology in the management of these conditions with the goal of children entering adulthood with healthy dentitions.
Keywords: Periodontal; paediatric; aesthetic corrections; gingivoplasty
Introduction
Introduction
Epidemiologic studies indicate that gingivitis of varying severity is nearly universal in children and adolescent [1,2] which in turn, may progress to jeopardize the periodontium of the adult. Very recently, an association of a higher risk of dental caries and periodontal disease with overweight, obesity and prediabetic conditions has also been reported [3]. The cause of gingivitis is plaque and local conditions such as material alba and poor hygiene, favor its accumulation. However, plaque appears rapidly in the age of 8 to 12 years and is less in preschool children [4]. The underlying systemic disturbances and genetic predisposition contribute to common occurrences like primary herpetic gingivostomatitis, candidiasis and necrotizing ulcerative gingivitis [5]. The unique appearance of polypoid granulation tissue in deciduous molars and permanent first molar is a dental polyp, characterized by lymphocytes, neutrophils and plasma cells. Some other conditions like fibromas are easily diagnosed by histopathology [6]. In the normal oral cavity, the gum tissue recedes as the tooth continues to erupt and moves into its proper position. But a sudden onset of pain and inflammation of the operculum, or the flap of gum that partially covers erupting wisdom teeth leads to pericoronitis. Depending on the severity of infection, there is abscess, cellulitis and involvement of lymph nodes [7]. The surgical excision of the tissue is often the treatment of choice. Aesthetic corrections have led to an increasing importance in seeking treatment, especially the removal of aberrant frenum [8] and gum sculpting for artificial crown fabrication. Gingivoplasty and osseous surgery is performed to recapture a good physiologic form for ideal gingival architecture [9].
Clinical Cases
Case 1
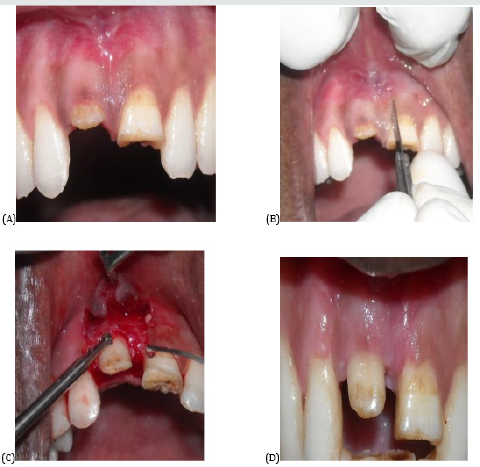
An 11-year-old patient reported to FACES N BRACES Research Centre for fever and severe pain in back tooth. Oral examination revealed carious 16 with polyp growth (Figure 1A-1D). The vitality tests showed negative response and endodontic therapy along with excision was decided on radiographs. On obtaining a written informed consent, 2% Xylocaine hydrochloride with adrenaline (1;80000) was administered. The complete removal was done with electrosurgery followed by thorough saline irrigation. Ibuprofen400mg twice a day for 3 days was prescribed during healing period.
Case 2
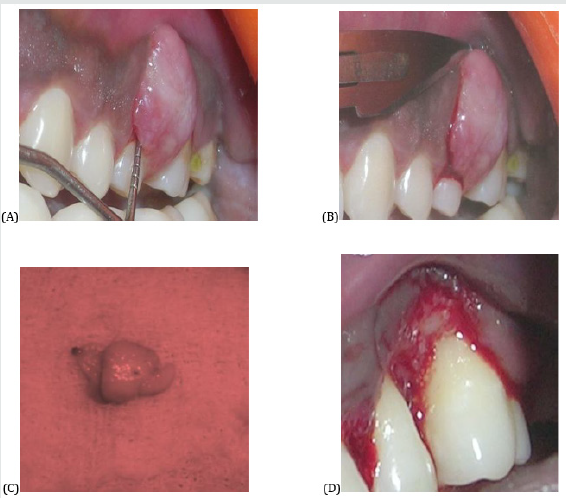
The patient presented with a growth on gums in relation to tooth which caused pain on mastication. Clinical inspection revealed a gingival overgrowth measuring 4x5mm with an absence of history of any prolonged medicine intake (Figure 2A). Under an appropriate anaesthesia, an incision was given using scalpel and the tissue was sent for biopsy (Figure 2B-2D). The patient was called the next day after prescribing the NSAIDS and antibiotics along with 0.2 % chlorhexidine gluconate mouth rinse. Bundles of well -formed collagen fibers with a scattering of fibrocytes and variable vascularity, characteristic of a fibroma was seen in histopathology.
Figure 1: A) Carious 16 with polyp, B) Electro surgical removal, C) Degranulation completed, D) Healing after 1 week.
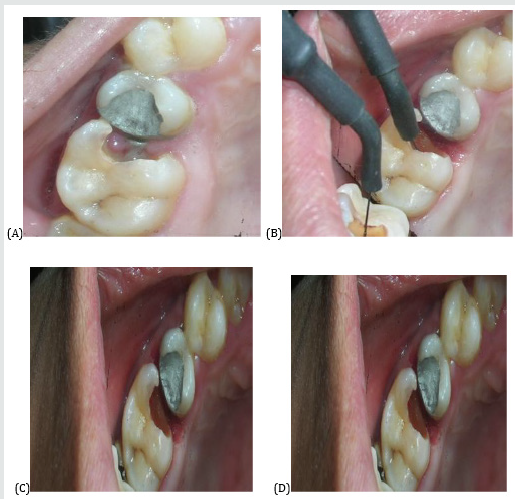
Figure 2: A) Fibroma in relation to 26, B) Incision with BP blade & scalpel, C) Biopsy specimen, D) Healing after 24hours.
Case 3
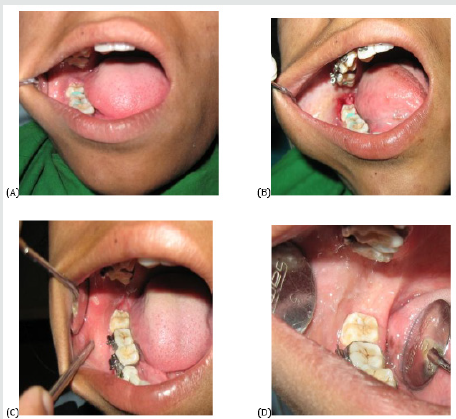
The patient complained of inability to chew from right side of face and fever for three days. A pericoronal flap circumscribing the tooth 48 was seen (Figure 3A) and extraction of 48 was not indicated. Thus, an ablation with Nd:Yag laser was done on the site upon a written informed consent from patient’s parents and patient recalled after one week for follow up (Figure 3B-3D).
Figure 3: A) Pericoronitis irt 48; B) Removal with Nd:Yag laser; C) Healing after 48 hours; D) Healing after one week.
Case 4
A 12-year-old patient was referred for the complaint of progressive spacing between the upper central incisors. Soft tissue examination confirmed a frenum pull in 11 & 21 region. The decision on frenectomy was accepted by patient’s parents. Resorbable sutures and Perio pack were given upon complete removal by scalpel (Figure 4A-4D)
Figure 4: A) Frenum Pull irt 11& 21, B) Frenectomy incision, C) Complete removal along with tissue tags, D) Healing after suture emoval.

Case 5
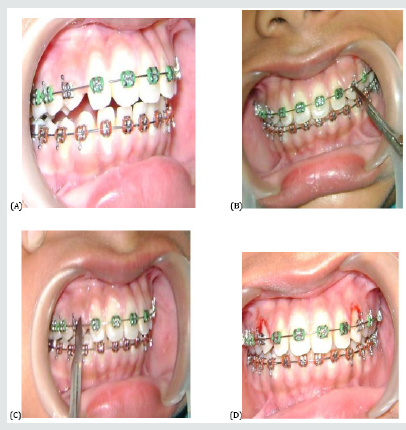
A compromise on hygiene compliance was noticed in a female undergoing malocclusion correction. It resulted in gingival proliferation in 13 & 23 region (Figure 5A). Gingivoplasty was performed 9 with scalpel and orthodontic straightening could be continued as planned (Figure 5B-5D).
Figure 5: A) Enlarged gingival irt 13 & 23; B) Gingivoplasty irt 23; C) Gingivoplasty irt 13; D) Restoration of gingival architecture.
Case 6
The patient had undergone an accident which caused a fracture of tooth 11. The reluctancy for extraction of permanent natural tooth and a desire for restoration of lost smile was expressed by him. After taking the X ray and pulp vitality testing, crown lengthening was done with osteotomy, followed by fixed ceramic crown (Figure 6A-6D).
Figure 6: A) Fractured 11; B) Incision placement; C) Flap and osteotomy with bur; D) Crown lengthening done.
Conclusion
Although there is a much lower prevalence of destructive periodontal diseases in young patients than in adults, children can develop severe forms of periodontitis [10]. Since early diagnosis ensures the greatest chance for successful treatment, it is important that children receive a periodontal examination as part of their routine dental visits.
References
- Ramfjord SP (1961) The periodontal status of boys 11 to 17years old in Bombay, India. J Periodontol32(3): 237-248.
- Durward CS, Wright FA (1989) The dental health of IndoChinese and Australian-born adolescents. Austr Dent J34(3):233-239.
- Drummond BK, Brosnan MG, Leichter JW (2017) Management of periodontal health in children: Pediatric dentistry and Periodontology interface. Periodontol 200074(1):158-167.
- Mattson L (1978) Development of gingivitis in preschool children and young adults. A comparative experimental study. J Clin Periodontol 5(1): 24-34.
- Pindborg JJ, Bhat M, Devanath KR, Narayana HR, Ramachandra S (1966) Occurrence of acute necrotizing gingivitis in South India children. J Periodontal 37(1):14-19.
- Schneider LC, Weisinger E (1978) The true gingival fibroma; an analysis of 129 fibrous gingival lesions. JPeriodontol 49(8):423-424.
- Perkins AE (1944) Acute infections around erupting mandibular third molar.Br Dent J 76: 199.
- Devishree, Gujjari SK, Shubhashini PV (2012) Frenectomy: A review with the reports of surgical techniques. J Clin Diagn Res6(9): 1587-1592.
- Prichard J (1961) Gingivioplasty, gingivectomy, and osseous surgery. J Periodontol32: 275-282.
- Löe H, Brown LJ (1991) Early onset periodontitis in the United States of America. J Periodontol62(10):608-616.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




