
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4692
Research Article(ISSN: 2637-4692) 
Effect of Saline Mouthwash on the Oral Flora Volume 5 - Issue 2
Nokam Kamdem* Gimel Stephane Junior, Zilefac Brian Ngokwe, Ntep Ntep David Bienvenue, Kwedi Karl Guy Gregoire, Kouamo Tchiekou Audrey Mariette, Elage Epie Macbrain, Toukam Michel
- Department of Dentistry, University of Yaounde, Cameroon
Received: January 20, 2022 Published: January 28, 2022
Corresponding author: Nokam Kamdem, Department of Dentistry, University of Yaounde, Cameroon
DOI: 10.32474/MADOHC.2022.05.000207
Summary
Mouthwash is the process of soaking the teeth, gums and mucosa of the mouth with a solution. Its purpose is to improve oral
hygiene and to treat certain oral pathologies. The aim of this work is to evaluate the in vitro effect of salt water mouthwashes on
oral flora. We conducted a cross-over clinical trial in the Bacteriology Department of the Central Laboratory of the Yaounde General
Hospital. This study lasted 6 months, from November 2019 to April 2020. During the course of this work, we carried out convenience
sampling. Each participant in our study received the same intervention (mouthwash) at a specific time and the effect was observed
at regular intervals (H1 - H5). A period of 3 days (wash-out period) was observed between the interventions (mouthwashes with
different saline solutions: 0.9%; 2%; 5.8% and 23%) in order to avoid carry-over effects. Gram staining was performed before the
mouthwashes and 7 hours after the mouthwashes to determine the bacterial species affected by the mouthwashes.
We recruited 10 participants from whom we took 240 saliva samples. The sex ratio was 1:1. Our results showed that 2 minutes
after mouthwash all solutions decreased the oral flora (e.g., 5.8% saline reduced the initial flora by half). The activity of the 0.9%
saline was limited to this interval, while the homemade saline (2%) had an antibacterial effect on the oral flora that lasted for 3
hours. However, as the sampling continued only the 5.8% and 23% concentrations reduced the oral flora significantly. The 5.8%
salt concentration had an antibacterial action of 5 hours while the 23% salt concentration had an action of 7 hours. Furthermore,
we noted a more marked activity on gram positive bacteria. The 5.8% saline has a long-lasting efficacy and is better tolerated by
the participants. The homemade saline can be prescribed for short term indications as it has an antibacterial action that lasts for 3
hours. The 23% saline should be avoided because of its pungent and irritating taste.
Keywords: Mouthwash; Saline Solution; In Vitro Study; Oral Flora
Introduction
Mouthwash is the process of soaking the teeth, gums and mucous membranes of the mouth with a solution. The purpose of this procedure is to improve oral hygiene and to treat certain oral pathologies [1]. Salt water, various herbal infusions and an alkaline solution of sodium bicarbonate have long been used in oral hygiene. But, due to the antiseptic properties of new solutions such as Chlorhexidine, Povidone Iodine, etc., these natural solutions are used less frequently.[1] However, due to the side effects of these solutions, natural solutions such as saline mouthwash would seem to be more advantageous. Indeed, Kim et al. demonstrated that salt water mouthwash (at specific concentrations) could improve oral hygiene. He also showed that a salt water mouthwash would decrease xerostomia, halitosis and significantly decrease the bacterial mass of the oral cavity [2]. We conducted this study with the aim of comparing the in vitro effect of different concentrations of saline solution to that of 0.9% saline on the oral flora; ultimately, we want to find the best alternative with less risk in oral care.
Methodology
We conducted a cross-over clinical trial over a period of 6
months from November 2019 to April 2020. This study took
place in the bacteriology department of the central laboratory of
the Yaoundé General Hospital. We selected 10 participants from
among the Dental medicine students of the Faculty of Medicine and
Biomedical Sciences of the University of Yaoundé 1. Participants
had to meet 6 criteria: be aged 20-25 years in apparent good health;
have good oral health; not have taken any medication that could
modify the oral flora; not wear dentures; not perform any oral
hygiene act 12 hours before the start of the clinical trial and have
had a scaling within the last 6 months. We excluded any participant
who was suffering from a disease that could affect the oral flora,
neglecting oral hygiene, unavailable during the study period; Also
excluded were those who took medication that could affect the
flora; who ate less than 1 hour before the start of the sampling; who
ate during the sampling period. We then obtained ethical clearance
from the institutional ethics and research committee of the Faculty of Medicine and Biomedical Sciences of the University of Yaoundé 1
and research authorization from the Yaoundé General Hospital. The
information leaflet was explained and the informed consent form
given to the participants. Mouthwashes were free of charge and the
results of our clinical trial were given and explained to participants.
In the procedure, each participant in our study performed
a mouthwash between 9:00 - 9:30am with 10ml of solution for
30seconds. Effects were observed at regular intervals during the
day including 2 minutes, 1 hour, 3 hours, 5 hours and 7 hours
after mouthwash. A period of 3 days was observed between each
mouthwash in order to ensure that the flora was reconstituted ad
integrum. On the saliva samples, gram staining was performed
before the mouthwash and 7 hours after the mouthwash in order to
determine any changes in the bacterial flora. Saliva samples were
analyzed for bacterial colony count (viable plate count method) [3].
Saliva samples consisted of 1ml of unstimulated saliva collected
in a dry sterile tube. We used 4 different concentrations of saline
for our study (these concentrations were chosen according to the
classification of bacterial halotolerance) [4]. These were 0.9%
saline (0.16M); 2% saline (home-made preparation: 5mg of salt in
250ml of water) (0.34M) [5]; 5.8% hypertonic saline (1M); 23%
hypertonic saline (4M). The preparation of our solutions was carried
out with conventional table salt and sterile distilled water. The salt
used had the following concentration: Sodium chloride: 97% min;
Iodine: 100ppm; Anti-caking agent E-536: 10ppm; Calcium: 25mg/
kg max; Magnesium: 150mg/kg max; Sulphate: 400mg/kg max;
Insoluble: 0.01% max; Moisture: 0.1% max. We determined the
molar concentration of each solution before use using the following
formulae: molar concentration = number of moles (mol)/volume
(l) and mole = mass (g)/molar mass (mol/g).
Data analysis
The data were recorded with Microsoft Excel. Differences between groups were determined by Student’s paired-sample t-test; the repeated measures analysis of variance allowed us to compare the means obtained by paired samples. Probability values of P < 0.05 were considered statistically significant. However, the adjustment of the p-value with the Bonferoni correction was used due to the multiple statistics that were performed. We used SPSS 26.0 software to perform these different statistical tests.
Results
In this study we had 10 patients from whom we took a total of 240 saliva samples (24 samples per patient). The age of the patients ranged from 22 to 25 years, with an average of 23.6 years±0.96 in girls and 22.6 years±0.80 in boys. The bacterial load of our patients before mouthwash (H0) was different from each other as revealed in Table 1. Furthermore, this table shows the effect of the different mouthwashes on the oral flora at all different intervals H1 - H5. The action of the solutions is different but the differences are not statistically significant. The results of Gram-stained smears (Table 2) show a flora composition of 60-70% gram positive bacteria and 30-40% gram negative bacteria at H0. On analysis of the smears at H5 we observed a much greater reduction of gram-positive bacteria after mouthwash with the following solutions: saline 5.8% and saline 23%. During our clinical trial we collected the subjective assessments of the participants towards the different mouthwashes. This shows that:
Table 1: Effects of different saline mouthwashes on oral flora with time
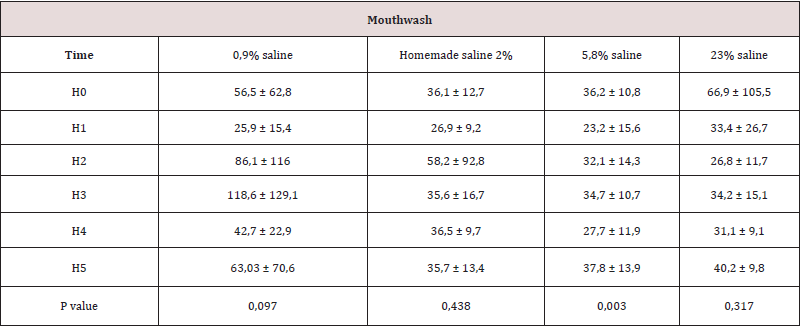
All values above are multiplied by 10^7 and expressed in CFU/ml
H0: sampling before mouthwash; H1: sampling 2 minutes after mouthwash; H2: sampling 1 hour after mouthwash; H3: sampling 3
hours after mouthwash; H4: sampling 5 hours after mouthwash; H5: 7 hours after mouthwash
Table 2: Results of Gram-stained smears at H0 and H5
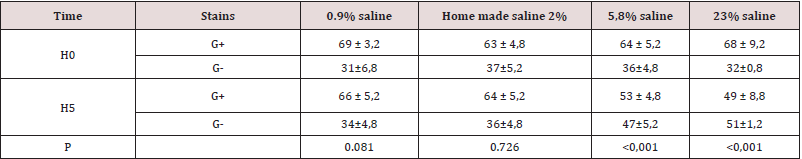
In black: gram positive bacteria; in blue: gram negative bacteria. (Result in %)
H0: sampling before mouthwash; H5: 7 hours after mouthwash
a) All participants experienced a salty taste after the 0.9% saline
and homemade saline mouthwashes. They described this taste
as normal and usual.
b) Half of the participants reported that the 5.8% saline was very
salty but still tolerable. While the rest of the participants found
its taste equivalent to the solutions mentioned above.
c) The 23% saline was not tolerated by any of the participants
during our clinical trial. All noted its pungent, aggressive and
irritating taste which took time to subside.
Discussion
Mouthwashes are frequently prescribed by dentists. Some socalled ‘comfort mouthwashes’ are even available in supermarkets. All these commercial or medical solutions have progressively replaced an old solution that had excellent results, namely the saline mouthwash [2,6,7]. Indeed, the use of salt water mouthwash is mainly based on empirical considerations, which are based on the fact that a solution with a high salt content can have antibacterial properties. Often referred to as a “grandmother’s solution”, it is simple to make and its constituents are affordable, namely drinking water and table salt. The price of a kilogram of table salt is much cheaper than the price of a bottle of chlorhexidine, hydrogen peroxide or povidone iodine. In addition to its low toxicity, it would be advisable to return to this solution, which has been proven in the past [1,6]. In view of the scarcity of scientific data on this subject, we undertook this study to investigate the antibacterial effect of different concentrations of salt water on the oral flora. For this analysis we used different saline solutions: 0.9%, homemade saline (2%), 5.8% and 23%. These solutions were chosen according to the halotolerance classification of bacteria described by Vreeland [8]. Each solution corresponded to a class of bacteria in the halotolerance classification. The effect of these different solutions was compared to the effect of 0.9% saline.
General Characteristics of the Population
Our population consisted of young oral health students with little age difference due to their ease of understanding the study procedure, accessibility and similarity of oral flora [9,10]. The differences in flora between individuals are comparable to the results obtained in the work of Addy and Smith who worked at the University of Cambridge on students and administrative staff and the work of Shapiro et al who worked at the University of Bergen on administrative staff [9-11].
Effects of Mouthwash on Oral Flora
The results of our study showed that 2 minutes after mouthwash
all solutions reduced the oral flora (e.g., 5.8% saline reduced the
initial flora by half). Two reasons could explain this reduction: the
first would be related to the physiological hyper-salivation that
follows the mouthwash. This serous saliva, mainly from the parotid
region, would dilute the oral flora and thus reduce the number of
bacteria counted. The second explanation would be the immediate
antiseptic effect of mouthwash on bacteria: saline solutions can
cause cells to dry up and then fatally lose their cell structure and
function. This bacterial cell depletion is especially observable in
light halophiles, as they have very little capacity to adapt to a saline
environment.
The 0.9% saline solution has a limited action in this range
because it is isotonic for mucous membranes and bacteria. This
result is similar to the work of Shapiro and Smith [10,11]. However,
as sampling continued only two substances reduced oral flora
significantly (saline 5.8%, and saline 23%). The first: the 5.8%
saline reduced oral flora for 5 hours while the effect of the 23%
saline was 7 hours. The effect of the 2% saline solution was 3
hours. These results suggest that these mouthwashes have a longlasting
effect on the oral flora. This is probably due to: The longtime
taken by the salivary hypersecretion to dilute these high salt
concentrations. Thus, the strong osmotic pressure exerted by a
high Na Cl level is maintained. This will have a lasting effect on the
growth and survival of the bacteria.
The long-lasting action of 5.8% and 23% saline could be due to
their adhesion to the dental plaque. Indeed, the patients included
in our study had not performed any oral hygiene act 12 hours
before the beginning of the mouthwashes. This is sufficient time
for plaque to form (30 minutes) [12]. It is likely that the 5.8% and
23% salts adhere to the glycoprotein matrix (exogenous acquired
film) and thus destroy the plaque bacteria. It is also likely that
the non-removal of salt-rich bacterial cell debris perpetuates the
action of salt on plaque. Given that the concentration of Na+ in
saliva increases with salivary flow to the point of reaching plasma levels, it is likely that this concentration of Na+ combined with that
obtained after salt water mouthwash increases the alkalinity of the
medium and thus inhibits bacterial growth [13]. When comparing
the action of these saline solutions with that of other mouthwashes
described in the literature, it can be seen that these mouthwashes
have a greater or equal effect (for example : Povidone iodine has
an effect that lasts 1 hour according to Addy et al[9]; Triclosan and
Hexeditin have an antibacterial effect that lasts 3 hours according
to Jenkins et al, Shapiro et al and Tartaglia et al[11,14,15]; Acidified
sodium chlorite and sodium lauryl sulphate have an effect that lasts
7 hours according to Yates et al and Jenkins et al[15,16] etc.) .)
Bacterial modification after mouthwash
After analysis of the results, we can observe that the solution that had the most effect on the oral flora was the 23% saline solution. This reduced the oral flora by half during the whole experiment (7 hours). However, the participants were bothered by its pungent, irritating and disgusting taste compared to homemade saline (2%) and saline 5.8%. This reaction can be explained by the hyperstimulation of the ionophores of the taste cells. Indeed, the Na+ cation is responsible for the salty taste; therefore, the mouthwash with 23% saline will cause an excessive stimulus discharge because sodium ion receptors are ubiquitous on the tongue [17]. These assessments, although subjective, lead to the conclusion that it would be advisable to turn to 5.8% saline, which is better tolerated and has a 5-hour antibacterial effect. However, for short term indications (3 hours), home-made saline can be used or prescribed. Examination of the Gram-stained smears showed us a flora composition of 60-70% gram positive bacteria and 30-40% gram negative bacteria at H0. On analysis of the smears at H7 we observed a much greater reduction of gram-positive bacteria after mouthwash of the following solutions: saline 5.8% and saline 23%. This observation would indicate that the 5.8% and 23% saline would be much more active on gram positive bacteria.
Conclusion
The 5.8% saline has a long-lasting efficacy and is better tolerated by the participants. The homemade saline can be prescribed for short-term indications as it has an antibacterial action that lasts for 3 hours. The 23% saline should be avoided because of its pungent and irritating taste.
References
- Bain de bouche (2020) Wikipedia [Internet].
- Kim JO, Kim NC (2014) Effects of 4% hypertonic saline solution mouthwash on oral health of elders in long term care facilities. J Korean Acad Nurs 44(1): 13-20.
- Larcher C, Larcher C Techniques de dénombrement p. 9-11.
- https://www.lachimie.fr/definitions/calcul-nombre-mole.php
- Hygiène de la bouche (2020) Société canadienne du cancer [Internet].
- Un gargarisme à l’eau salée - Remèdes naturels pour soulager une rage de dents - Doctissimo -10 remèdes naturels pour soulager une rage de dent.
- Critères de choix bactériologiques lors de la prescription de bains de bouche antiseptiques en odonto-stomatologie (1).
- Vreeland RH, Miller KJ (1987) Mechanisms of halotolerance in microorganisms. 14(4): 311-356.
- Addy M (1978) Comparison of the in vivo and in vitro antibacterial properties of povidone iodine and chlorhexidine gluconate mouthrinses. 5(3): 198-205.
- Smith RG, Moran J, Addy M, Doherty F, Newcombe RG (1995) Comparative staining in vitro and plaque inhibitory properties in vivo of 0.12% and 0.2% chlorhexidine mouthrinses. J Clin Periodontol John Wiley & Sons 22(8): 613-611.
- Shapiro S, Giertsen E, Guggenheim B, Guggenheim B (2002) An in vitro Oral Biofilm Model for Comparing the Efficacy of Antimicrobial Mouthrinses. Caries Res 36(2): 93-100.
- Robert MJ. Module- Bactériologie Informations.
- De A, Universite N-M, Poincare-Nancy H, De F, Dentaire C, et al. (2007) Etude Experimentale Du Test Salivaire Carlo Analyse Sur Des Patients Subissant Une Radiotherapie De La Shere Oro Faciale Présentée et soutenue publiquement le 28 Juin 2006 Examinateurs de la thèse.
- Tartaglia GM, Tadakamadla SK, Connelly ST, Sforza C, Martín C (2019) Adverse events associated with home use of mouthrinses: a systematic review. Ther. Adv. Drug Saf. SAGE Publications Ltd.
- Jenkins S, Addy M, Newcombe R (1991) Triclosan and sodium lauryl sulphate mouthwashes: (I). Effects on salivary bacterial counts. J Clin Periodontol 18(2):140-144.
- Yates R (1997) The comparative effect of acidified sodium chlorite and chlorhexidine mouthrinses on plaque regrowth and salivary bacterial counts. J Clin Periodontol [Internet]. Blackwell Munksgaard 24: 603-609.
- Caicedo A, Kim KN, Roper SD (2002) Individual mouse taste cells respond to multiple chemical stimuli. J Physiol, Wiley-Blackwell 544(2): 501-509.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




