Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4692
Mini Review(ISSN: 2637-4692) 
Covid Safe Orthodontics: A Review of Principles & Practices. Volume 4 - Issue 5
Gurkeerat Singh1, Akanksha Shukla2*, Gaurav Saluja3, Anu Rathi4, Varun Goyal5 and Raj Kumar Singh6
- 1MDS, M Orth, Professor and Head of the Department, Sudha Rustagi College of Dental Sciences and Research, India
- 2Post graduate student, Sudha Rustagi College of Dental Sciences and Research, India
- 3Post graduate student, Sudha Rustagi College of Dental Sciences and Research, India
- 4Post graduate student, Sudha Rustagi College of Dental Sciences and Research, India
- 5MDS, Professor, Sudha Rustagi College of Dental Sciences and Research, India
- 6MDS, Reader, Sudha Rustagi College of Dental Sciences and Research, India
Received: April 21, 2021 Published: May 05, 2021
Corresponding author: Akanksha Shukla, Post graduate student, Sudha Rustagi College of Dental Sciences and Research, Fraidabad, Haryana, India
DOI: 10.32474/MADOHC.2021.04.000198
Introduction
With more than 116 million positive cases and 2.5 million deaths across the world due to coronavirus outbreak, the COVID-19 has rapidly spread across various countries in the past one year [1]. Lockdowns, quarantines, and social distancing had become the norm across the globe leaving only essential services to work. Lower respiratory tract infections including fever, coughing, sneezing, fatigue are the primary symptoms of coronavirus disease [2]. These can vary from being asymptomatic to mild change in sense of smell and taste to acute respiratory distress that might be further complicated by sepsis and multi organ failure leading to death [3,4]. The virus has been reported to be highly contagious even during its latency period and the incubation period can be anywhere between 2 weeks to 3 weeks [5]. Dental departments including the orthodontists face a higher risk of disease transmission because of the nature of dental procedures, getting exposed to aerosols and droplets splashing from patient’s mouth. The transmission can be multifold in a dental clinic occurring from treating an asymptomatic patient to the operator, from operator to other healthcare workers in the facility, forwarding to other patients and from one patient to another [6]. We as dentists have extensively known the basic principles of personal protection to prevent acquisition and transmission of various biological infections possible during different dental procedures. It is, however, important to re-evaluate the infection control measure within our practice to prevent the cross-infection and contamination of this highly contagious infection (Figures 1 & 2). The aim of this article is to enlist what all procedures and precautions that can be taken by orthodontists at various levels to reduce and minimize the transmission of this virus.
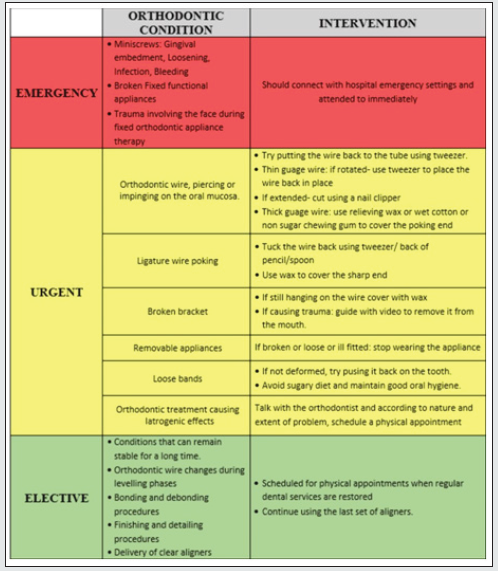
This article is divided into sections for protocols and safety measures according to different aspects of the practice: Triage, Operatory, Hygiene Protocols, Treatment procedures, Sterilization and Infection control. The very first step of any patient in the OPD demands careful screening and sterilization to avoid any unnecessary risk exposure. The dental procedures are divided into three categories. According to the urgency and associated risk of infection the treatment should be undertaken [7]. Keeping the doors opened at all times and using foot pedals wherever needed will reduce the transmission through these areas of contact. It is advisable to keep the exchange of currencies to bare minimum and make arrangements for online transactions of treatment charges. Similarly, all the treatment procedural updates can be made computerized or can be voice recorded.
Operatory
1. Alternate dental chairs should be made working in case chambers are not present in the department [8].
2. Artificial partitions or room dividing boards could be used to contain the aerosols generated.
3. The held able areas should be covered with plastic clingfilm and changed after every patient.
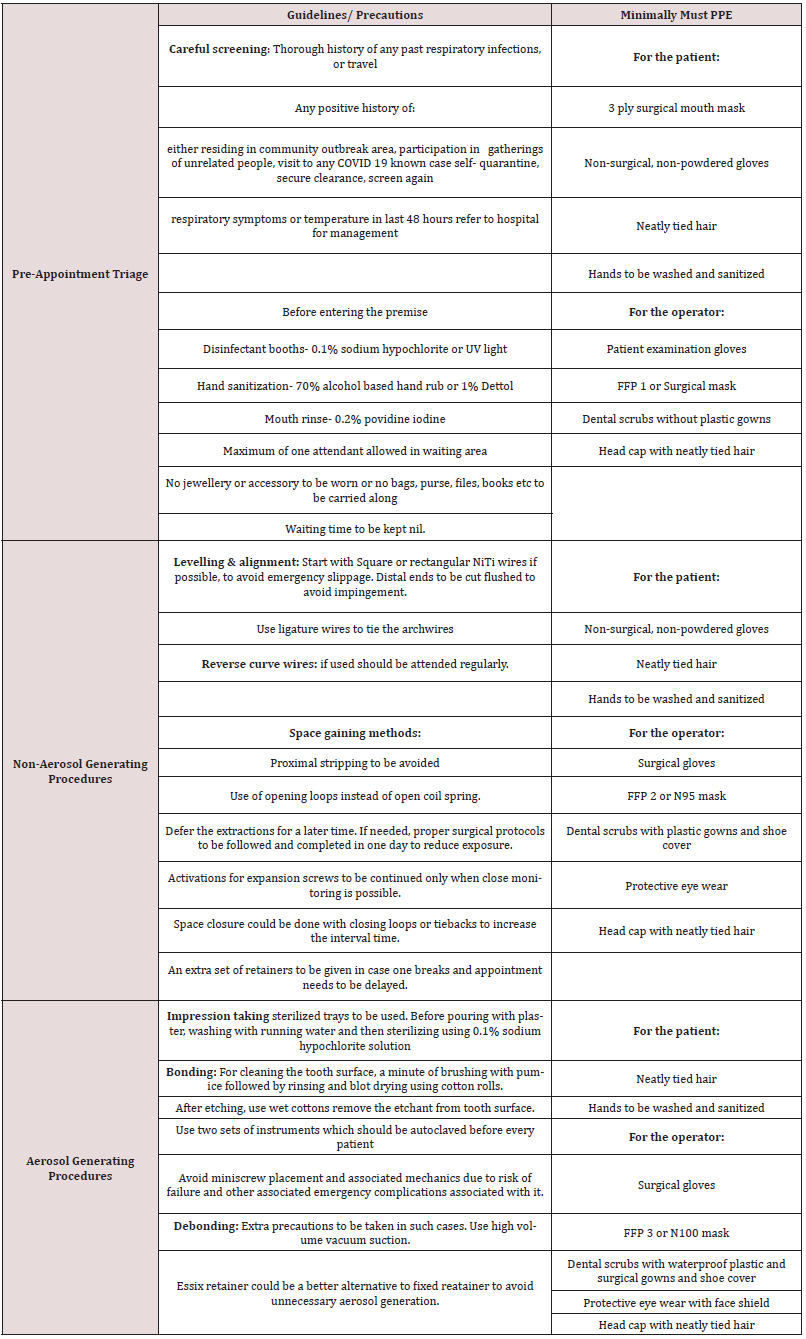
4. Before and after any procedure the dental chair should be disinfected with phenolics, iodophors or chlorine containing compounds (Table 1).
Hygiene Protocols
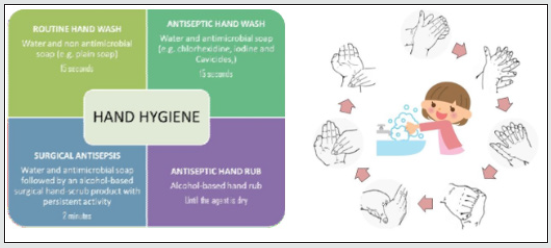
1. Hand hygiene is the most effective method of reducing the risk of the transmission of disease [9].
2. Hand Hygiene is MANDATORY before putting on and after removing gloves, and after inadvertent barehanded touching of contaminated surfaces or objects or after completing laboratory activities.
3. It is also RECOMMENDED after sneezing, coughing, blowing the nose or combing hair and after contact with your own face.
4. Hand wash should be done by patient and operators before entering and after leaving the operatory at all times.
Personal Protection Protocols
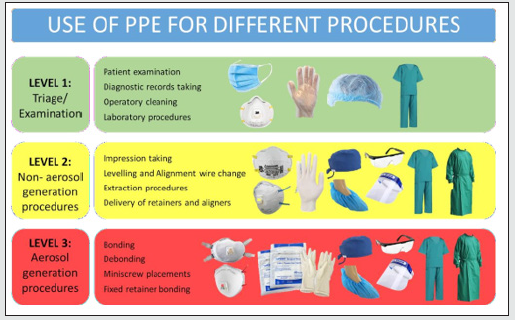
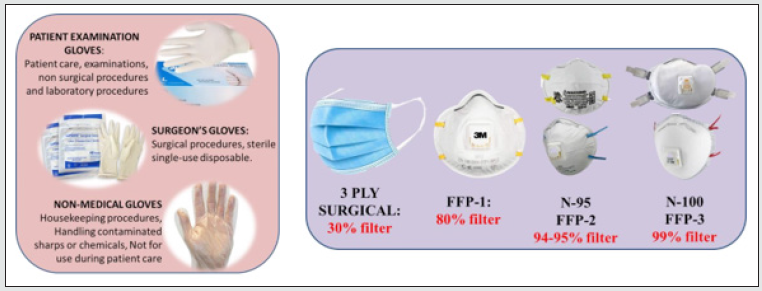
Personal Protection equipment should be in place for all the operators and dental auxiliaries including the helpers and cleaners. Since there is a cost associated with standard PPE kits, we can try to minimize the expenditure by following certain simple protocols. Mucosal surfaces of the eyes, mouth, and nose are vulnerable areas for contagious agents spread by patient saliva, aerosols and orthodontic supplies and instruments (Figures 3 & 4). Appropriate attire in the clinic protects the operator from contamination by aerosols and splatter which might get carried outside the clinical environment. Either protective eyewear or a chin-length plastic face shield must be worn during dental procedures. A face shield does not substitute for a surgical mask. Protective eyewear must possess side shields. Departmental scrubs should be made mandatory. It should be worn at all times in the department and sterilized on a daily basis. Gowns must be changed at least daily or more often if they are visibly soiled. Used gowns should never be stored with other personal clothing. Fluid resistant gowns must be worn for all patient treatment and clean-up [10].
Orthodontic Treatment Procedures
1. Most routine orthodontic procedures fall under Level 2 of treatment stages [11-13].
2. Following table lists stepwise precautions to be taken for every orthodontic procedure along with minimal requirement of PPE for the same.
Sterilization
1. A pre-procedural mouth rinse with an oxidizing mouthwash such as 1.5% H2O2, 1% povidine-iodine, or even HOCl acid may prove beneficial, since it has been suggested that the coronavirus could be vulnerable to oxidation.
2. Hypochlorous acid (HOCl) is a weak acid created when chlorine dissolves in water to form a hypochlorite. It can be mixed fresh and used within 90 minutes.
3. UV sterilizers, or autoclaves should be used for sterilizing orthodontic instruments after every patient.
4. 2% Gluteraldehyde can be used for sterilizing alginate impressions, burs, preformed bands, photographic retractors also.
Conclusion
These are the strenuous times of transition and adaptation to a new lifestyle, new form of human interactions, new way of working as responsible society and human beings is what we need the most. We need to be better equipped to deliver treatments with all the customary precautions as we become more aware of our actions and how our actions affect each other’s well being too.
References
- https://www.bbc.com/news/world-51235105
- Mathur N, Tyagi S, Dwivedi V, Narang A, Tyagi P, et al. (2020) Dental considerations amidst COVID-19 scare. Int J Med Biomed Stud 4(3): 1.
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, et al. (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382: 1708-1720.
- Hassan SA, Sheikh FN, Jamal S, Ezeh JK, Akhtar A (2020) Coronavirus (COVID-19): A review of clinical features, diagnosis, and treatment. Cureus 12(3): e7355.
- Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, et al. (2020) A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res 7: 4.
- Ge ZY, Yang LM, Xia JJ, Fu XH, Zhang YZ (2020) Possible aerosol transmission of COVID-19 and special precautions in dentistry. J Zhejiang Univ Sci B 1-8.
- Guidelines for dental professionals in Covid-19 pandemic situation.
- Protocol- Covid 19.
- Infection control manual, University of Illinois Chicago.
- Peditto M, Scapellato S, Marcianò A, Costa P, Oteri G (2020) Dentistry during the COVID-19 Epidemic: An Italian Workflow for the Management of Dental Practice. Int J Environ Res Public Health 17(9): 3325.
- Caprioglio A, Pizzetti GB, Zecca PA, Fastuca R, Maino G, et al. (2020) Management of orthodontic emergencies during 2019-NCOV. Prog Orthod 21: 10.
- M Srirengalakshmi, Adith Venugopal, Paolo Jesus P Pangilinan, Paolo Manzano, Jassin Arnold, et al. (2020) Orthodontics in the COVID-19 Era: The way forward Part 1 orthodontic treatment considerations. J Clin Orthod 54(6): 341-349.
- M Srirengalakshmi, Adith Venugopal, Paolo Jesus P Pangilinan, Paolo Manzano, Jassin Arnold, et al. (2020) Orthodontics in the COVID-19 Era: The way forward Part 2 orthodontic treatment considerations. J Clin Orthod 54(6): 341-349.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...