Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1217
Research ArticleOpen Access
Phytochemical Screening & Biological Investigations of Ficus Racemosa Volume 2 - Issue 4
Abdul Kader Mohiuddin1*, Sayra Akter Lia2
- 1Secretary and Treasurer, Dr. M. Nasirullah Memorial Trust, Bangladesh
- 2B. Pharm (World University of Bangladesh), M. Pharm (North South University), Bangladesh
Received: July 23, 2020; Published: August 15, 2020
*Corresponding author: Abdul Kader Mohiuddin, Secretary and Treasurer, Dr. M. Nasirullah Memorial Trust, Tejgaon, Dhaka 1215, Bangladesh
Abstract
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Ficus racemosais an important medicinal plant, found in India, Australia, and Southeast Asia. It is popularly known as ‘gular.’ It reduces blood glucose concentration due to the presence of β-sitosterol. Many active constituents that have been isolated from various parts of this plant possess useful pharmacological activities. The objective of this dissertation is to identify the biological activity of the roots of an indigenous medicinal plant, viz., Ficus racemosa (Family: Moraceae) and to evaluate the possible phytochemical and pharmacological profiles of the crude extracts. So far, some chemical and biological investigations have been carried out on this plant mainly focusing on the bark and root of the plant. That’s why the goal of this framework is to explore the potential possibilities of developing new drug candidates from the fruit of this plant which could be crucial for the treatment of various ailments.
Keywords: Ficus racemose; Phytochemical screening; Thrombolytic activity; Antimicrobial activity; Medicinal plants of Bangladesh
Introduction
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Rationale and objective of the work
Phytochemistry is a branch of Pharmacognosy, with chemical and biological characters, which study the obtaining of medicaments by natural or semi synthesis methods? The subject “Phytochemstry” deals with the chemical structures of secondary metabolites, their metabolism, and their distribution and biological functions [1] (Figure 1).
Written records of the use of plants as medicinal agents
date back thousands of years. The oldest records come from
Mesopotamia and date from about 2600 BC. Those records are not
simply a case of one or two plant based ‘drugs’ finding their way
into popular use, because the documents indicate that there were
many drugs in use that contained plants (up to 1,000 in the case
of Mesopotamia) [2]. Approximately 119 pure chemical substances
extracted from higher plants are used in medicine throughout the
world. In most of the traditional, the medicinal plants include the
fresh or dried parts, whole, chopped, powdered or an advanced
form of the herb usually made via extraction by a solvent such as
water, ethanol or an organic solvent play a major role and constitute
the backbone of traditional medicine[3].
Goals of using plants as sources of therapeutic agents are:
To isolate bioactive compounds for direct use as drugs
e.g. digoxin, digitoxin, morphine, reserpine, taxol, vincristine,
vinblastine.
1. To produce bioactive compounds of novel or known
structures as lead compounds for semi synthesis to produce
patentable entities of higher activity and/or lower toxicity
e.g. metformine, nabilone, oxycodone, taxotere, teniposide,
verapamil and miodarone which are based on galegine, A9-
tetrahydrocannabinol, morphine, taxol, podophyllotoxin,
khellin.
2. To use agents as pharmacologic tools e.g. lysergic acid
diethylamide, mescaline [4].
There are several familiar approaches for lead searching from
the plants and the isolated bioactive compounds are utilized in
three basic ways:
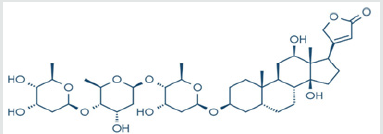
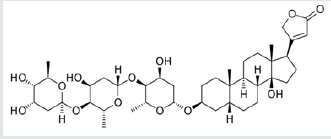
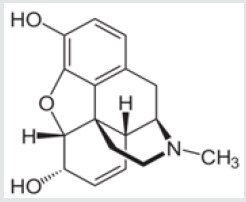
Unmodified medicinal plant products where ethnomedical uses
suggested clinical efficacy e.g. digitoxin (a), digoxin (b), morphine
(c) (Figure 2a-2c).
1. Unmodified natural products of which the therapeutic
efficacy was only remotely suggested by indigenous plant use
e.g. vincristine.
2. Modified natural or synthetic substances based on a
natural product used in folk medicine e.g. aspirin [5].
3. Terrestrial plants, especially higher plants, have a long
history of use in the treatment of human diseases [6]. Fossil
records date human use of plants as medicines at least to the
Middle Paleolithic age some 60,000 years ago [7].
Several well-known species, including licorice (Glycyrrhiza glabra) myrrh (Commiphoraspecies), and poppy capsule latex (Papaver somnjferum), were referred to by the first known written record on clay tablets from Mesopotamia in 2600 BC, and these plants are still in use today for the treatment of various diseases as ingredients of official drugs or herbal preparations used in systems of traditional medicine. Furthermore, morphine, codeine, noscapine (narcotine), and papaverine isolated from P. somnferumwere developed as single chemical drugs and are still clinically used. Hemisuccinate carbenoxolone sodium, a semi-synthetic derivative of glycyrrhetic acid found in licorice, is prescribed for the treatment of gastric and duodenal ulcers in various countries [6].
Success in natural products research is conditioned a careful plant selection, based on various criteria such as chemotaxonomic data, ethnomedical information, field observations or even random collection [8]. Historical experiences with plants as therapeutic tools have helped to introduce single chemical entities in modem medicine. Plants, especially those with ethno- pharmacological have been the primary sources of medicines for early drug discovery. In fact, a recent sis by Fabrican and Farnsworth showed that the uses of 80% of 122 plant-derived drugs were related to their original ethno pharmacological purposes. Current drug discovery from terrestrial plants has mainly relied in bioactivity-guided isolation methods, which, for example, have led to discoveries of the important anticancer agents, paclitaxel from Taxus radioligand camptothecin from Camptothecaacuminate [6].
The goals of using plants as sources of therapeutic agents are
a) To isolate bioactive compounds for direct use as drugs,
e.g. digoxin, digitoxin, morphine, reserpine, taxol, vinbiastine,
vincristine.
b) To produce bioactive compounds of novel or known
structures as lead compounds for semisynthesis to produce
patentable entities of higher activity and/or lower toxicity, e.g.,
metformin, nabilone, oxycodon (and other narcotic analgesics),
taxotere, teniposide, verapamil, and miodarone, which are
based, respectively, on galegine, 9- tetrahydrocannabinol,
morphine, taxol, podophyllotoxin, and khellin.
c) To use agents as pharmacologic tools, e.g., lysergic acid
diethlamide (LSD), mescaline, yohimbine.
d) To use the whole plant or part of it as an herbal remedy,
e.g., cranberry, echinacea, feverfew, garlic, etc[9].The number
of higher plant species (angiosperms and gymnosperms)
on this planet is estimated at 250,000[10]with a lower level at 215,000 [11]and an upper level as high as 500,000[12].Of
these, only about 6% have been screened for biologic activity,
and a reported 5% have been evaluated phytochemically[13].
It was estimated that in 1991 in the United States, for every
10,000 pure compounds most likely those based on synthesis)
that arebiologically evaluated (primarily in vitro), 20 would be
tested in animal models, and 10 of these would be clinically
evaluated, and only one would reach U.S. Food and Drug
administration approval for marketing. The time required for
this process was estimated at 10 years at a cost of $231 million
(U.S.) [14].
The major drawback of this strategy is the frequent isolation of known metabolites. Therefore, hyphenated techniques (LC-UV, LCMS, and LC-NMR have been developed; in order to detect is early as possible potential original structures. These compounds can then be tested in various bioassays [8]. More recently combinatorial chemistry and high throughput robotic screening techniques have been employed as viable strategies for drug discovery programs [15]. Chemical diversity of secondary plant metabolites that results from plant evolution is superior to at found in synthetic combinatorial chemical libraries [14]. Medicinal plants have played an essential role in the development of human culture, for example religions and different ceremonies. (E.g. Dutura has long been associated with the worship of Shiva, the Indian God). Plants are directly used as medicines by a majority of cultures around the world, for example Chinese medicine and Indian medicine. Many food crops have medicinal effects, for example garlic. Medicinal plants are resources of new drugs. Studying medicinal plants helps to understand the plant toxicity and protect human and animals from natural poisons. Cultivation and preservation of medicinal plants protect biological diversity, for example metabolic engineering of plants [16]. The medicinal plants find application in pharmaceutical, cosmetic, agricultural and food industry. With onset of scientific research in herbals, it is becoming clearer that the medicinal herbs have a potential in today’s synthetic era, as numbers of medicines are becoming resistant. According to one estimate only 20% of the plant flora has been studied and 60% of synthetic medicines owe their origin to plants. Ancient knowledge coupled with scientific principles can come to the forefront and provide us with powerful remedies to eradicate the diseases.
In real sense, coupling of ancient knowledge and scientific
principle is essential:
1. To identify alternative and complementary medicine.
2. To reduce the toxicity of drug therapy especially toxicity
reduction of synthetic and semi synthetic drugs.
3. To find the lead compound diversification to treat various
diseases [17].
History of traditional herbal medicine in Bangladesh
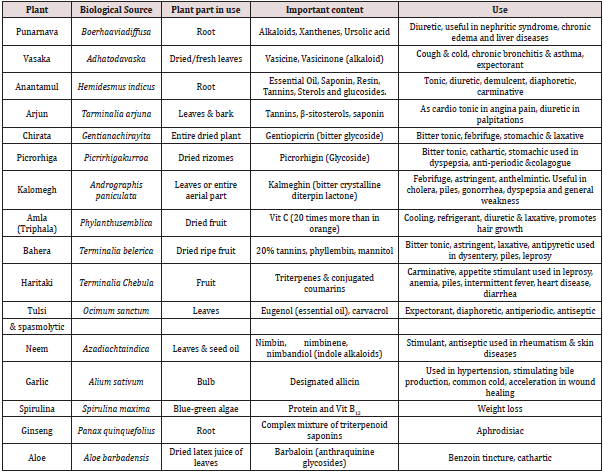
Traditional Medicine is the medicine or treatment based on traditional uses of plants, animals or their products, other natural substances (including some inorganic chemicals), religious verses, cultural practices, and physical manipulations including torture. As this system of medicine has been in use almost unchanged generation after generation throughout the ages for the treatment of various physical and psychological diseases, it is called traditional. Most of the times, the type, preparation, and uses of traditional medicines are largely influenced by folklore customs and the cultural habits, social practices, religious beliefs and, in many cases, superstitions of the people who prescribe or use them [18]. The earliest mention of traditional medicine is found in “Rigveda”, the oldest repository of knowledge in this subcontinent. Later “Ayurveda”, developed from the Vedic concept of life, became the important source of all systems of medical sciences. In course of time it became a part of culture and heritage of the people of the Indian subcontinent Traditional medicine involves the use of both material and non-material components. The material components invariably comprise parts or organs of plants and their products. They also consist of animal organs, minerals and other natural substances. The non-material components, which constitute important items of religious and spiritual medicines, include torture, charms, magic, incantations, religious verses, amulets and rituals like sacrifices, appeasement of evil spirits, etc. [18]. Treatments in traditional medicine are carried out by internal and external application of medicaments, physical manipulation of various parts of the body, performing rituals, psychological treatment, and also by minor surgery. Ayurvedic medicinal preparations consist mainly of plant materials in the form of powders, semi-solid preparations, decoctions, elixirs and distillates. Many of them also contain inorganic chemical substances, minerals and animal products. Alcoholic extracts and alcoholic solutions of the ingredients, tinctures and elixirs are also frequently used in Ayurvedic medicine [18]. Whole plants or their powders or pastes or products and their extracts, infusions, decoctions and distillates constitute the major constituents of Unani medicine. Minerals, inorganic chemicals and animal products are also frequently used in preparing these medicines. For hundreds of years, the medical knowledge of the Indian subcontinent is termed as Ayurveda. Ayurveda remains an important system of medicine and drug therapy in India and Bangladesh. Plant alkaloids are the primary active ingredients of Ayurvedic drugs. Toda’ the pharmacologically active ingredients of many Ayurvedic medicines are being identified and their usefulness in drug therapy being determined. As only a certain percentage of plants are used in traditional medicines, it is roughly estimated that of the discovered 17,000 species, nearly 3,000 species are used in medicinal field [19]. Some crude drugs used as medicine in Bangladesh are reported in following (Table 1).
Research of traditional drugs in Bangladesh
In rural areas medicinal plants have been being used as remedy
for disease for a long time. They not only cure the disease but
also provide an important role in the economy. Medicinal plants
are cheap and easy to get to those people who knew it very well.
Bioactive compounds are deposited in medicinal plants; it can serve
as important raw materials for pharmaceutical manufacturing.
They comprise a precious asset of a country and donate to its health
care system. Well-judged and scientific investigation of this wealth
can significantly contribute to the public health. Besides being
available commodity of commerce. A country can also earn a good
amount of foreign currency by exporting this natural wealth to
other countries. More than 500 of such medicinal plants have so far
been established as growing in Bangladesh [20]. Almost all of these
indigenous medicinal plants are extensively used in the preparation
of unani, ayurvedic and homeopathic medicines in Bangladesh.
A survey conducted in 1990 in different villages of Bangladesh
shows that on average of 14% of people suffering from illness
approach qualified allopathic doctors, 29% contact unqualified
village doctors, 10% contact mullahs, 29% contact quack and
19% contact homeopaths. The survey indicates an extensive
use of medicinal plants, most of which are served in crude and
substandard form, by our people [21]. Traditional medicines
are still manufactured in our country by following the ageold
unscientific, traditional methods. Hundreds of indigenous
medicinal plants are employed in different Ayurvedic and Unani
commercial preparations without proper standardization, quality
control, evaluation and determination of the chemical nature,
pharmacological and toxicological studies of the active components
which are essential to utilize their therapeutic potential fully.
Toxicity of the plants or plant extracts is coming to light with the
advancement of science. Since Bangladesh is a country of low
economic growth, a proper health care system can be established by supplying low cost medicines to its population. This may be
possible only by developing standard drugs from our natural
resources of medicinal plants. In order to achieve this goal research
and development of traditional medicines should be given the
due priority [20]. Besides, Bangladesh imports a large quantity of
pharmaceutical raw materials including medicinal plants and semiprocessed
plant products to manufacture drugs. Each year a great
deal of money is spent on this purpose.
General approaches to drug discovery from natural sources
In general, three different approaches have been, and continue to be used in the drug discovery process from natural sources. These approaches are traditional empirical and molecular [22]. During the Vedic period the ‘Susruta samhita’ and the “charaka samhita” were influential works on traditional medicine. Hundreds of medicinal plants were identified and have been traditionally used since then. Over the following centuries, Ayurvedic practitioners developed a number of medicinal preparations and surgical procedures for the treatment of various ailments and diseases. WHO (World Health organization) estimates that 80% of the populations living in the developing countries rely exclusively on traditional medicine for their primary health care needs. In almost all the traditional medicine, the traditional plants play a major role and constitute the backbone of the traditional medicine. Indian Materia medical includes about 1600 drugs of vegetable origin almost all of which are derived from different traditional system and folklore practices [23]. Examples include drugs like morphine, quinine and ephedrine that have been in widespread use for a long time, and more recently adopted compounds such as the antimalarial artemisinin. The empirical approach builds on an understanding of a relevant physiological process and often develops a therapeutic agent from a naturally occurring lead molecule. Examples include tubocurarine and other muscle relaxants, propranolol and other b-adrenoceptor antagonists, and cimetidine and other H2 receptor blockers. Development of molecular biological techniques and the advances in genomics lead to molecular approach. The molecular approach to drug discovery can be further subdivided into three general categories. The first is rational drug design using computer aided techniques. A second area is the antisense approach, which is based on manipulation of genetic targets. The third technique, which currently dominates drug discovery activity, is the pragmatic approach of random screening. With recent technological developments in molecular biology, instrumentation and information technology, screening of compounds can be conducted by high throughput screening method. High throughput screening is an automated testing process of large number of compounds versus a large number of targets which is particularly effective in identifying potential lead compounds. Robotics and miniaturization of in vitro tests on genetically modified cells has led to high throughput screening [22]. The major advantage of natural products for random screening is the structural diversity. Since Bioactive natural products often occur as a part of a family of related molecules, it is therefore possible to isolate a number of homologues compounds and obtain structure-activity relationship. Of course, lead compounds found from screening of natural products can be optimized by traditional medicinal chemistry or by application of combinatorial approaches. Overall, when faced with molecular targets in screening assays for which there is no information about low molecular weight leads, use of a natural products library seems more likely to provide the chemical diversity to yield a hit than a library of similar numbers of compounds made by combinatorial synthesis. Since only a small fraction of the world’s biodiversity has been tested for biological activity, it can be assumed that natural products will continue to offer novel leads for novel therapeutic agents [22]. In earlier times, all drugs and medicinal agents were derived from natural substances, and most of these remedies were obtained from higher plants. Today, many new chemotherapeutic agents are synthetically derived, based on “rational” drug design. The study of natural products has advantages o’er synthetic drug design in that it leads optimally to materials having new structural features with novel biological activity. Not only do plants continue to serve as important sources of new drugs, but phytochemicals derived from them are also extremely useful as lead structures for synthetic modification and optimization of bioactivity. The starting materials for about one-half of the medicines we use today come from natural sources. Virtually every pharmacological class of drugs includes a natural product prototype. The future of plants as sources of medicinal agents for use in investigation, prevention, and treatment of diseases is very promising [24].
Phytotherapy
The treatment of diseases by the use of the plants is known as phytotherapy. Phytotherapy was the beginning of pharmacotherapy or treatment of disease by means of drugs. Therapeutics uses of plants had in effect stored at the very beginning of human life on the earth when the primitive man out of necessity and by intuition, restored to using plants to alleviate suffering from injuries and diseases [25]. Phytotherapy laid the foundation stone of all from of medical treatment that are practiced today. With the development of human civilization of phytotherapy exhibits a stepwise development, which can be enumerated as:
A. 1st stage: Crude drugs were employed, prepared in the roughest manner, such as powdered willow in the management of pain.
B. 2nd stage: These were converted into more active and manageable forms, such as extracts or solutions watery or alcoholic.
C. 3rd stage: The pure active principles separated from crude drug were employed e.g. salicylic acid.
D. 4th stage: Attempt to synthesize the active drug in the laboratory and indeed structural modification. e.g.Aspirin.
Medicinal plants and drug development
Development of drugs from medicinal plants is often an
elaborate laborious time consuming and expensive exercise.
Careful phytochemical analysis and pharmacological and clinical
tests are pre-requisites for developing drugs from medicinal plants.
The stage involve in the following way development exercise may
be summarize as follows:
(i) Selection and correct identification of the proper
medicinal plants and its extraction with a suitable solvent.
(ii) Detection of biological activity of the crude extent and
establishment of a bioassay system to permit the identification
of the active fractions and rapid discarding of the inactive ones.
(iii) Fraction of the crude extracts by using physico-chemical
procedure and monitored by biological tests identification and
separation of the active fractions.
(iv) Isolation of the active constituents by chromatographic or
other technique and purification of the isolation compounds by
repeated chromatography and crystallization.
(v) Establishment of the chemical structures of the
pure compound by various physicochemical techniques
and determination of their biological activity by various
pharmacological tests.
Contribution of medicinal plants to modern drug
Plants have contributed and are still contributing to the
development of modern synthetic drugs and medicine in a number
of ways as stated below:
(i) Novel structure of biologically active chemical compounds
isolated from plants sources, often to prompt the chemists to
synthesis similar or better semi-synthetic compounds.
(ii) Synthetic drugs with similar or more potent therapeutic
activity are often prepared by structural modification of the
plant derived compound with known biological activity.
(iii) Chemists for use as potent drugs often prepare various
analogues of derivatives of plant constituents with similar or
better pharmacological action and therapeutics properties.
Homatropine (a synthetic tropane alkaloid similar to atropine)
syrosingopine (a synthetic derivative of reserpine) chloroquine
(a synthetic derivative of quinine) dihydromorphinone,
oxymorphine, methyldihydromorphinone, ethyl morphine and
N-allylnormorphine (synthetic derivatives of morphine) are some of the example of such synthetic drug which plants have
contributed indirectly. Even in this age of synthetic drug there are
some naturally occurring drugs, such as the Digitalis glycoside used
in cardiac complications and the Catharanthus alkaloids used in
cancers, which have no synthetic alternatives. In such cases plants
continue to remain as their principal and oily sources.
Status of medicinal plants of Bangladesh
(i) About 500 medicinal plants have been reported to occur
in Bangladesh.
(ii) Almost 80% of rural populations are dependent on
medicinal plants for their primary health care.
(iii) The local people conserve traditional knowledge through
their experience and practices which is handed down orally
without any documentation.
(iv) The over exploitation of wild medicinal plants has become
a threat to its extinction.
(v) In Bangladesh there is no systematic cultivation process
of conservation strategies about medicinal plants.
(vi) There is no government policy or rules and regulations
about the medicinal plants cultivation conservation and
marketing.
(vii) There are almost 422 herbal medicinal companies using
medicinal plants as raw materials mostly by importing from
abroad.
Chemical constituents of medicinal plants
The commonly occurring chemical substances which are
responsible for the medicinal (as well as toxic) properties of plants
include the following:
1. Volatile or essential oils
2. Fixed oils
3. Gum-resins and mucilage
4. Alkaloid and amines:
a. Pyridine group
b. Tropane group
c. Isoquiloline group
d. Quinoline group
e. Quinolizidile group
f. Indole group
g. Steroidal group
h. Phenylethylamine group
i. Alkaloid amines
5. Glycosides:
a. Anthraquinone glycoside
b. Cardiac glycoside
c. Saponin glycoside Thiocyanate glycoside
d. Other glycoside
6. Vitamin and mineral
Flow Chart of bioactivity guided phytochemical approach
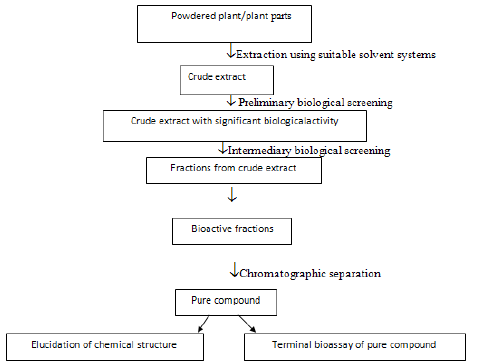
The objective of this dissertation is to identify the biological activity of the roots of an indigenous medicinal plant, viz., Ficus racemosa (Family: Moraceae) and to evaluate the possible phytochemical and pharmacological profiles of the crude extracts. So far, some chemical and biological investigations have been carried out on this plant mainly focusing on the bark and root of the plant. That’s why the goal of this framework is to explore the potential possibilities of developing new drug candidates from the fruit of this plant which could be crucial for the treatment of various ailments.
Plant Preview
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
The plant family: Moraceae
Ficus racemosa is an attractive fig tree with a crooked trumk
and a spreading crown. Unlike the banyan, it has no aerial roots.
The most distinctive aspect of this tree is the red, furry figs in short
clusters, which grow directly out of the trunk of the tree [26].
Leaves: The leaves are dark green, 6-10cm long, glabrous;
receptacles small subglobose or piriform, in large clusters from old
nodes of main trunk.
Fruits: The fruits receptacles are 3-6cm in diameter, pyriform,
in large clusters, arising from main trunk or large branches. The fruits resemble the figs and are green when raw, turning orange, dull
reddish or dark crimson on ripening. The fruit of Ficus racemosa
Linn is 3/4inch to 2 inches long, circular and grows directly on the
trunk [27].
Flowers:
Seeds: The seeds are tiny, innumerable, and grain-like. Outer surface of the bark consists of easily removable translucent flakes grayish to rusty brown, uniformly hard and non-brittle.
Bark: Bark is reddish grey or grayish green, soft surface, uneven and often cracked, 0.5-1.8cm thick, on rubbing white papery flakes come out from the outer surface, inner surface light brown, fracture fibrous, taste mucilaginous without any characteristic odour. Unlike the banyan, it has no aerial roots. Those looking for the flower of goolar should know that the fig is actually a compartment carrying hundreds of flowers [28].
Roots: The roots of F. racemosa are long, brownish in color. It’s having characteristic odor and slightly bitter in taste Roots are irregular in shape [29,30].
Vernacular names
Scientific Name: Ficus racemosa
Synonyms: Ficusracemosa var. mollis, Ficusglomerata
Bengali: Dumor, উউউউউউউ,Udumbara
English: Gular fig, Country Fig, Cluster Fig
Gujarati: Goolar, Umbaro
Hindi: Dumar, Jantu Phal, Goolar, Goolar, Pani Bhuj, Pushp-hina,
Udumbara, Dharma Patra, Umari
Malayalam: Aththi, Udumbaram, Atthi, Jantuphalam, Atthi-al
Other name: Dumrii, Redwood Fig, Indian Fig, Cluster Fig,
Atteeka, Goolar, Vellaiatthi, Crattock, Country Fig, Gular Fig,
Rumbodo, Athi
Oriya: Dimri
Tamil: Anai, NallaAtthi, MalaiyinMunivan, VellaiAtthi, Atti,
Utumparam, Atti
Telugu: Atti, Bodda, Brahmamamidi
Urdu: Dumar
Recent taxonomic revisions of the family include these genera: [29][30].
a. Ficus chittagonga
b. Ficus glomerata
c. Ficus glomerata var. chittagonga
d. Ficus glomerata var. elongata
e. Ficus glomerata var. miquelii
f. Ficus glomerata var. mollis
g. Ficus goolereea
h. Ficus henrici
i. Ficus lanceolata
j. Ficus lucescens
k. Ficus mollis
l. Ficus racemosa var. miquelii
m. Ficus racemosa var. mollis
n. Ficus racemosa var. vesca (F. Müll. ex Miq.) Barrett
o. Ficus semicostata
p. Ficus trichocarpa
Classification (Ficusracemosa L. Taxonomic Serial No.: 506544)
Domain: Eukaryota
Kingdom: Plantae
Sub-kingdom: Viridiplantae
Phylum: Magnoliophyta
Sub-phylum: Euphyllophytina
Infra-phylum: Radiatopses
Division: Tracheophyta
Class: Magnoliopsida
Subclass: Magnoliidae
Order: Rosales
Family: Moraceae
Genus: Ficus
Species: Ficusracemosa (Figure 3-5)
Plant Description
Ficus racemosa, 20 to 30m high; bole buttressed; bark 8-10mm thick, surface reddish-brown or yellowish-brown smooth, coarsely flaky, fibrous; blaze creamy pink; latex milky; young shoots and twigs finely white hairy, soon glabrous; branchlets 1.5-3mm thick, puberulous [31].Leaves simple, alternate, stipules 12-18mm long, lanceolate, linearlanceolate, pubescent, often persistent on young shoots; petiole 10-50mm long, slender, grooved above, becoming brown scurfy; lamina 6-15 x 3.5-6cm, ovate, obovate, elliptic-oblong, elliptic-lanceolate, elliptic-ovate or oblongovate, base acute, obtuse or cuneate, apex narrowed, blunt or acute, margin entire, membranous, glabrous, blistered appearance on drying; 3-ribbed from base, 4-8 pairs, slender, pinnate, prominent beneath, intercostae reticulate, obscure. Flowers unisexual; inflorescence a syconia, on short leafless branches or warty tubercles of trunk or on larger branches, subglobose to pyriform, smooth, often lenticellate-verrucose; peduncle 3-12mm long, stout, orifice plane or slightly sunken, closed by 5-6 apical bracts; internal bristles none; basal bracts 3, 1-2m long, ovate, triangular, obtuse, persistent; flowers of unisexual, 4 kinds; male flowers near the mouth of receptacles, in 2-3 rings, sessile, much compressed; tepals 3-4, dentate-lacerate, lobes jointed below, red, glabrous; stamens 2, exserted; filaments 1mm, connate below; anthers oblong, parallel; female flowers sessile or very shortly stalked among gall flowers; tepals 3-4, dentate-lacerate, lobes jointed below, red, glabrous, ovary superior, sessile or substipitate, red spotted; style 2-3mm long, glabrous, simple; stigma clavate; gall flowers long stalked; ovary dark red, rough; style short[32].Syconium 2.5 x 2cm, orange, pink or dark crimson; achene granulate.
Scientific name: Ficus racemosa.
Common name: Dumor.
Family: Moraceae
Plant type: Evergreen and Shrub
Origin: The plant is found in Bangladesh, India, Pakistan, China,
Myanmar, Thailand, Indonesia, Vietnam, Australia etc.
Ecology: Ficus racemosa a well-known medicinal plant
commonly known as Dumor in Bengali is indigenous to Bangladesh.
The farmers on the roadside and fallen land can also cultivate
Ficusracemosa. This bush grows in all parts of the worlds. This
plant occurs throughout Bangladesh. This shrub grows on the
plains of Bangladesh and in the lower regions, up to a range of 1000
meters above sea level. This plant is also cultivated in other tropical
areas. It is also distributed in India, Myanmar, Thailand Indonesia
Vietnam, Australia etc.
Cultivation: Ficus species are common and form an important
element of lowland rain forest, both as canopy and understory
trees. Most species prefer per-humid forest, but several are found
in areas with a monsoon climate and in teak forest, including
locations where the soil dries out. Succeeds in full sun to partial
shade. Succeeds in most soils that are reasonably moist but welldrained.
Cluster fig is resistant to fire.
Parts used: Root, leaf, flower, fruit are used for therapeutic use. The leaves, roots, flowers and stem bark of this plant are used in medicinal applications.
Chemistry of the plant Ficus racemosa
Racemosa Linn species contain flavanoid glycosides, alkaloids, phenolic acids, steroids, saponins, coumarins, tannins, triterpinoids-oleanolic acid rusolic acid, α- hydroxy ursolic acid protocatechuic acid, maslinic acid. The nonenzymatic constituents include phenolic compounds, flavonoids, vitamin C. The enzymatic constituents present are ascorbate oxidase, ascorbate peroxidise, catalase, peroxidise. The phenolic compounds present are gallic acid and ellagic acid [33].
Medicinal uses of the plant Ficus racemosa
1. The leaves are used in the treatment of diarrhea.
2. The bark is astringent. It is used in the treatment of
hematuria, menorrhagia, and hemoptysis.
3. The fruit is astringent. It is used in the treatment of
hematuria, menorrhagia, and hemoptysis. The fruit, when filled
with sugar, is considered to be very cooling.
4. A fluid that exudes from the cut roots of the tree is
considered to be a powerful tonic when drunk for several
days together. The sap is a popular remedy in Bombay, that is
applied locally to mumps and other inflammatory glandular
enlargements and is also used in the treatment of gonorrhea.
5. The root is chewed as a treatment for tonsillitis.
Medicinal applications of the plant Ficus racemosa
A few of the health benefits derived from figs include:
Prevention of constipation: There are 5 grams of fiber in every three-fig serving. That high concentration of fiber helps promote healthy, regular bowel function and prevents constipation. Fiber works to add bulk and mass to bowel movements, so it not only prevents constipation, but also eliminates diarrhea and unhealthy or irregular bowel movements.
Weight loss: The fiber in Ficus racemosa also helps to reduce weight and is often recommended for obese people. However, their high calorie count can also result in weight gain, especially when consumed with milk. A few figs are enough to get the recommended amount of nutrients, so don’t overdo it! Remember, it is possible to have too much of a good thing.
Lower cholesterol: Ficus racemosa contain Pectin, which is a soluble fiber. When fiber moves through the digestive system, it basically mops up excess clumps of cholesterol and carries them to the excretory system to be eliminated from the body. As a soluble fiber, pectin from figs also stimulates healthy bowel movements. Figs can have a laxative effect, as they are one of the most fiberdense foods available. High amounts of fiber in your diet can benefit your overall health by preventing certain types of abdominal cancer, as well as colon cancer.
Prevention of coronary heart disease: Dried figs contain phenol, Omega-3 and Omega-6. These fatty acids reduce the risk of coronary heart disease. Furthermore, the leaves of figs have a significant effect on the level of triglycerides in a person’s system. Fig leaves have an inhibitory effect on triglycerides and makes the overall number of triglycerides drop. Triglycerides are another major factor behind various heart diseases.
Prevention of colon cancer: The presence of fiber helps to stimulate the elimination of free radicals and other cancer-causing substances, particularly in the colon, since fiber increases the healthy movement of the bowels.
Protection against post-menopausal breast cancer: Fiber content in figs have been known to protect against breast cancer, and after menopause, the hormonal balance in women can often fluctuate. The body’s systems are so interconnected that hormones affect the immune system, which is turn affect the ability of antioxidants to fight free radicals. Free radicals are prime factors behind the development of cancer, so figs take care of one extra line of defense by providing its wealth of fiber.
Good for diabetic patients: The American Diabetes Association recommends figs as a high fiber treat that helps promote functional control of diabetes. Fig leaves reduce the amount of insulin needed by diabetic patients who have to regularly take insulin injections. Ficus racemosa are rich in Potassium, which helps to regulate the amount of sugar which is absorbed into the body after meals. Large amounts of potassium can ensure that blood sugar spikes and falls are much less frequent, so figs can help diabetics live a much more normal life.
Prevention of hypertension: People usually take in sodium in the form of salt, but low potassium and high sodium level may lead to hypertension. Figs are high in potassium and low in sodium, so they are a perfect defense against the appearance and effects of hypertension, making figs a relaxing food as well, which can settle the nerves and bring some calmness to your day.
Bronchitis: The natural chemicals in Ficus racemosa leaves make it an ideal component for a tea base. Fig leaf tea has been popularly prescribed for various respiratory conditions like bronchitis, and it is also used as a way to prevent and lessen the symptoms of asthmatic patients.
Venereal Diseases: Figs have been traditionally used in the Indian subcontinent and a few other areas of the world as a calming salve for venereal diseases. Ingestion or topical application both work for relief from sexually transmitted diseases, although further research needs to be done on the exact range of symptoms and diseases which figs positively effect.
Sexual Dysfunction: For centuries, Ficus racemosa have been recommended as a way to correct sexual dysfunction like sterility, endurance, or erectile dysfunction. It has been a major part of mythology and culture, and most of the time, it is referenced as a powerful fertility or sexual supplement. Its actual success as an aphrodisiac is questionable, but the huge number of valuable vitamins and minerals might result in the sudden boost in energy and stamina that people mistake for a sexual surge. Soak 2-3 figs in milk overnight and eat them in the morning to enhance your sexual abilities.
Strengthens Bones:Ficus racemosa are rich in calcium, which is one of the most important components in strengthening bones and reducing the risk of osteoporosis. It is also rich in phosphorus, which encourages bone formation and spurs regrowth if there is any damage or degradation to bones.
Urinary calcium loss: People that maintain a high-sodium diet may be affected by increased urinary calcium loss. The high potassium content in figs helps to avoid that condition and regulates the content of waste in urine and minimizes the calcium lose, while increasing the amount of uric acid and other harmful toxins which you want to get out of your body.
Prevention of macular degeneration: Vision loss in older people is normally due to macular degeneration. Fruits and figs are particularly good at helping you avoid this very common symptom of aging.
Pharmacological activities of Ficus racemosa
Antimicrobial activity
Methanolic extracts of Ficus racemosa showed significant activity against four clinical strains of bacteria Staphylococcus aureus, Bacillus subtilis, Proteus vulgaris, and E. coli. The standard drug used was tetracycline (100mcg/ml). In both the cases, the methanolic extracts at dose concentration of 500μg/ml showed significant antimicrobial activity.
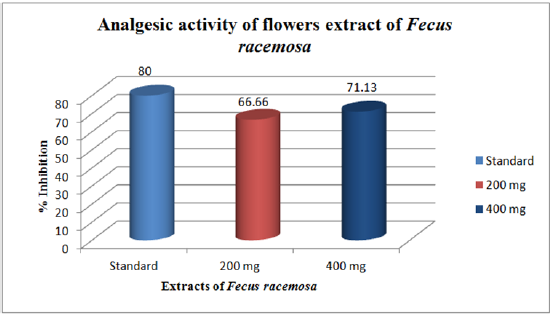
Analgesic activity
Saponin (SN) isolated from Ficus racemosa flowers exhibited protection from writhing induced by 1.2% v/v acetic acid in Adult Swiss albino mice. SN1 was administered ip at doses of 30, 50, 75 and 100mg/kg and standard drug used were aspirin, paracetamol, and morphine sulphate. In hot plate method, SN not only produced analgesia in mice but also potentiated the analgesic action of pentazocine and aspirin [34].
Antibacterial activity
The methanol extract of flowers of the plant have been screened for their antibacterial activity. The extract (7.5mg/disc) showed broad-spectrum antibacterial activity against gram positive and gram-negative bacteria. The results were compared with the standard drug streptomycin (10μg/ disc). The zone inhibition was found to be increased with the increase in concentration of the extract and thus exhibiting concentration dependent activity [35].
Preparation of Plant Extract
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Biological investigation of the experimental plants
A plant species representing to the family: Ficus racemosa was investigated in this study.

The investigations of the plant will be discussed in two different
sections.
• Phytochemical Investigation, and
• Biological Investigation.
Biological investigation of Ficus racemosa
Collection and preparation of the plant material: The whole plant of Ficus racemose was collected from Khamarbari, Farmgate, Dhaka and identified by taxonomist of National Herbarium, Bangladesh situated at Mirpur in Dhaka. The sample is preserved in the Phytochemical Laboratory of World University of Bangladesh for as further reference (Accession No. 41878). Fruits air dried for several days and then oven dried for 24 hours at considerably low temperature (not more than 400C) for better grinding. The dried fruits were then ground to a coarse powder using high capacity grinding machine in the Phytochemical Research Laboratory, Faculty of Pharmacy, World University of Bangladesh (WUB).
Extraction of the plant material: The powdered material (250gm) was taken in a cleaned, amber colored reagent bottle (5 liters) and soaked in 1.5L of methanol. The container with its content was sealed by bottle cap and kept for a period of 10 days accompanying occasional shaking and stirring. The whole mixtures were then filtered through a fresh cotton plug and finally with a Whatman No.1 filter paper. The volume of the filtrate was then allowed to evaporate at ambient temperature until approximately 70% solvent was evaporated.
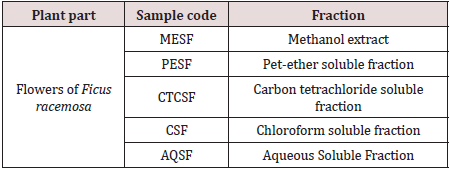
Solvent-Solvent partition of crude extract by Modified Kupchan Partition method: Solvent-solvent partitioning was done using the protocol designed by Kupchan [36]. The crude extract (5gm) was dissolved in 10% aqueous methanol. It was extracted with Petroleum ether, then with carbon tetrachloride and finally with Chloroform. The whole partitioning process is schematically shown in Figure 1. All the five fractions were evaporated to dryness and were used for further analysis.
Partitioning with Petroleum ether: The mother solution was taken in a separating funnel. 100ml of the Petroleum ether was added to it and the funnel was shaken and then kept undisturbed. The organic portion was collected. The process was repeated thrice, and the fractions collected were evaporated together in Rotary evaporator.
Partitioning with Carbon Tetrachloride: To the mother solution left after partitioning with petroleum ether, 12.5ml of distilled water was added and mixed. The mother solution was then taken in a separating funnel and extracted with carbon tetrachloride (100ml x3). The carbon tetrachloride fractions were collected together and evaporated. The aqueous fraction was preserved for the next step.
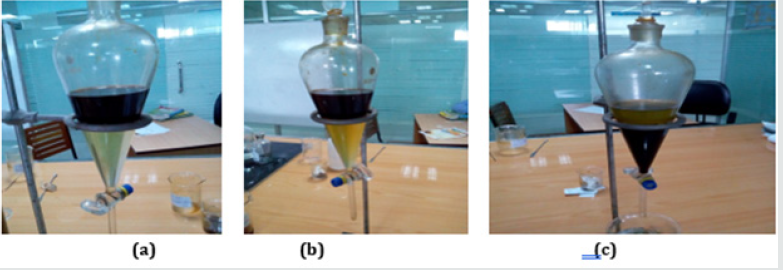
Partitioning with Chloroform: To the mother solution that left after washing with petroleum ether and carbon tetrachloride, 16ml of distilled water was added and mixed uniformly. The mother solution was then taken in a separating funnel and extracted with Chloroform (CHCl3) (100ml X 3). The CHCl3 soluble fractions were collected together and evaporated. The aqueous methanol fraction was preserved as aqueous fraction (Figure 6-8) (Table 2).
Figure 6: Schematic representation of the modified Kupchan Partitioning of crude extract of root of Ficus racemose.
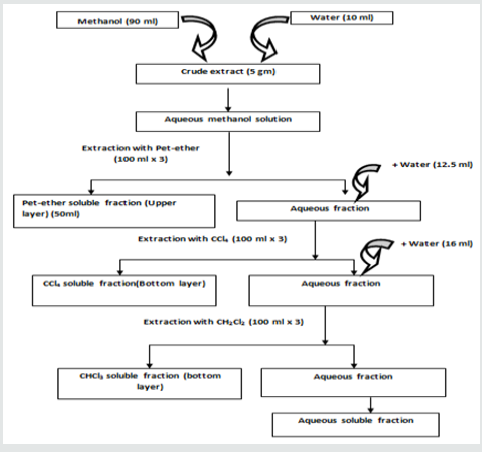
Figure 7: Partitioning of plant extract.
a. CHCl3 Soluble Fraction
b. Carbon Tetra Chloride SolubleFraction
c. Petroleum Ether Soluble Fraction
Design of Biological Investigation
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
General Approaches to Drug Discovery from Natural Sources
Natural products have been the most successful source of drugs ever. Research progressed along two major lines: Ethno pharmacology (medicinal herbs, substances of abuse, ordeal poisons) and toxicology (poisonous plants, venomous animals, arrow, and fish poisons). These strategies have already produced many valuable drugs and are likely to continue to produce lead compounds. Approximately 60% of the world’s population relies entirely on plants for medication [37]. Of the 520 new drugs approved between 1983 and 1994, 39% were natural products or derived from natural products and 60-80% of antibacterial and anticancer drugs were derived from natural products. Thirteen natural product related drugs were approved from 2005 to 2007, and five of these represented the first members of new classes of drugs: the peptides exenatide and ziconotide, and the small molecules ixabepilone, retapamulin. Current commercial evidence also supports the case for natural products. Of the 20 bestselling non-protein drugs in 1999, nine were either derived from or developed as the result of leads generated by natural products simvastatin, lovastatin, enalapril, pravastatin, atorvastatin, augmentin, ciprofloxacin, clarithromycin and cyclosporin with combined annual sales of >US$16 billion. Newer developments based on natural products include the antimalarial drug artemisinin and the anticancer agent’s taxol, docetaxel and camptothecin [38].
Today, many new chemotherapeutic agents are synthetically derived, based on “rational” drug design. The study of natural products has advantages over synthetic drug design in that it leads optimally to materials having new structural features with novel biological activity. Not only do plants continue to serve as important sources of new drugs, but phytochemicals derived from them are also extremely useful as lead structures for synthetic modification and optimization of bioactivity.
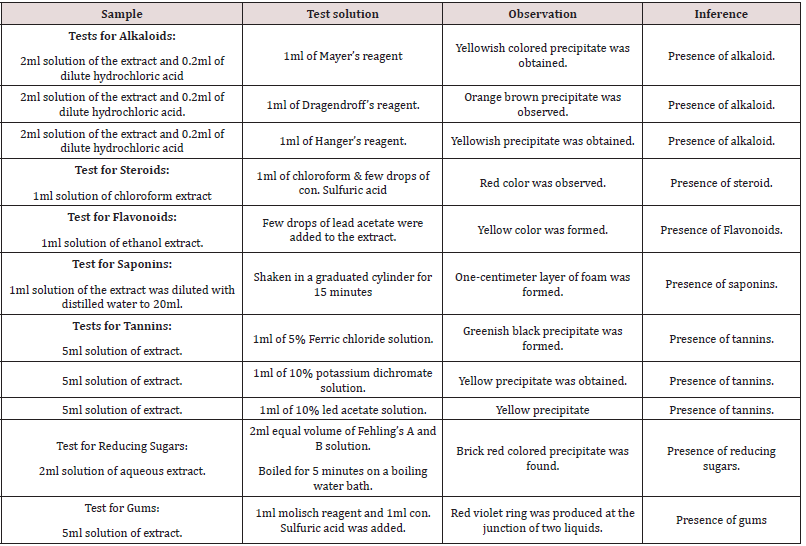
Investigations
The crude extract was subjected for chemical group tests and identified for - steroids, alkaloids, tannins, gums, flavonoids, reducing sugar and saponins. Results of different group tests are given in Table 3.
Results & Discussions
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Phytochemical studies showed that Alkaloids, Steroids,
Flavonoids, Tannins, Saponin, Gum & Reducing sugars are present
in the methanol extract of the plant. The experimental findings from
the study showed that the methanol extract has some important
groups and secondary metabolites that can show extensively
pharmacological activity.
The medicinal properties of plants have been investigated in the
recent scientific developments throughout the world due to their:
Microbiological investigations
The antibacterial as well as antifungal spectrum of the crude
extracts can be ascertained by observing the growth response with
the help of in vitro antimicrobial study. These experiments are
rationalized on the fact that many infectious diseases are caused
by bacteria and fungi and if the test materials inhibit bacterial or
fungal growth then they may be used in those particular diseases.
However, a number of factors can influence the results likea
a. The extraction method.
b. Inocula volume.
c. Culture medium composition.
d. pH and
e. Incubation temperature.
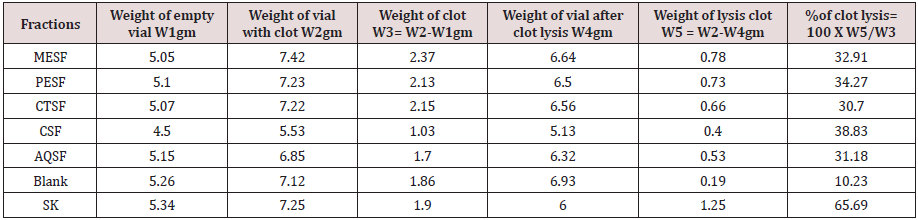
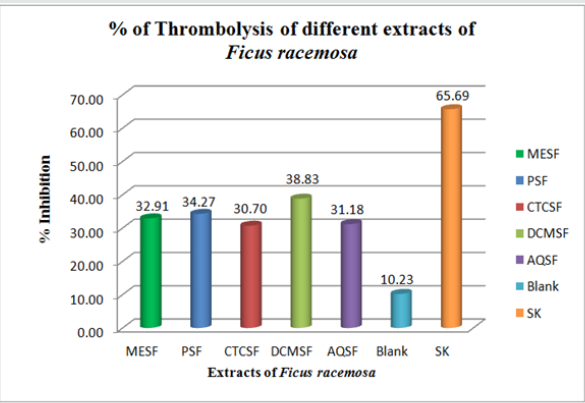
Thrombolytic activity investigation
Cerebral venous sinus thrombosis (CVST) is a common disorder that is often accompanied by significant morbidity and mortality. In anticoagulation therapy the intravenous heparin is the first line of treatment for CVST, because of its efficacy, safety and feasibility. However, thrombolytic therapy with its ability to produce rapid clot lysis has long been considered as an attractive alternative. Thrombolytic drugs like tissue plasminogen activator (t-PA), urokinase, streptokinase etc. play a crucial role in the management of patients with CVST.
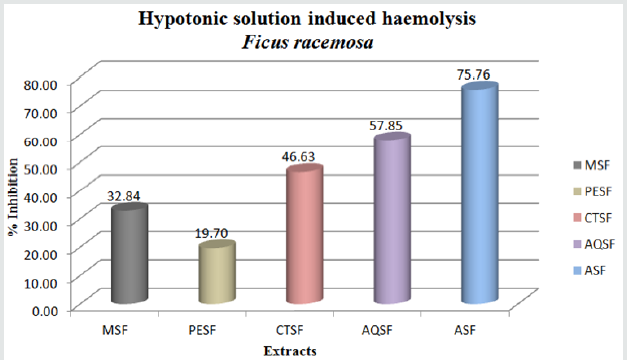
Membrane stabilizing activity investigation
Inflammatory cells produce a complex mixture of growth differentiation cytokines as well as physiologically active arachidonate metabolites .In addition they possess the ability to generate reactive oxygen species (ROS) that can damage cellular biomolecules which in return augments the state of inflammation [39]. The erythrocyte membrane resembles to lysosomal membrane and such as the effect of drugs on the stabilization of erythrocytes can be extrapolated to the stabilization of lysosomal membrane [40]. Therefore when membrane stabilizes they interfere in the release and in the action of mediators like histamine, serotonin, prostaglandine, leukotrines etc. [41].
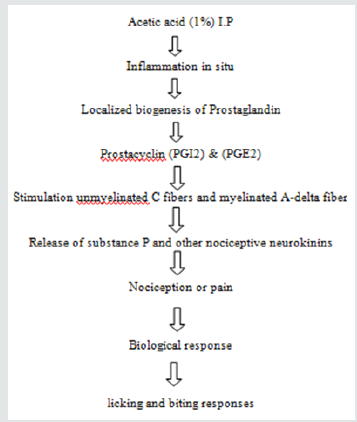
Analgesic activity investigation
Due to having adverse side effects like gastric lesion caused by
NSAIDs and tolerance and dependence induced by opiates, the use
of these drugs as analgesic agents have not been successful in all the
cases. So, analgesic drugs are being searched all over the world as
alternatives to NSAIDs and opiates. The investigation of the efficacy
of plant-based drugs used as traditional medicines have been paid
great attention because they are:
1. Cheap.
2. Have little side effects.
3. According to WHO, about 80% of the world’s population
rely mainly on plant-based drugs? So, in these dissertation two
types of analgesic activity has been evaluated.
4. Peripheral analgesic activity.
5. Central analgesic activity.
Hypoglycemic activity investigation
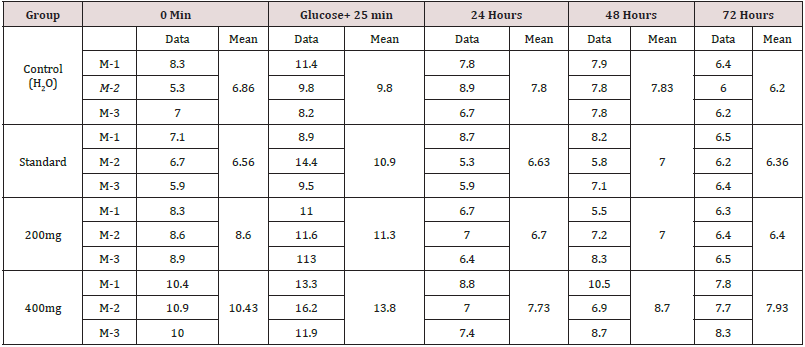
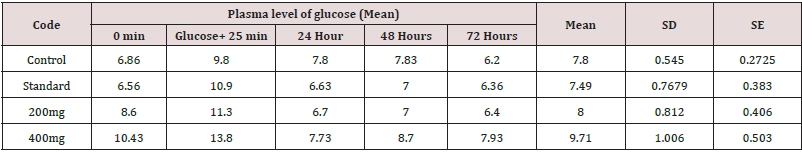
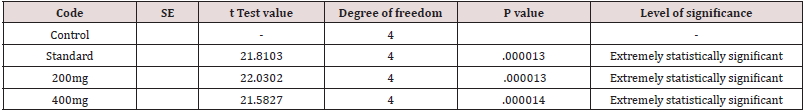
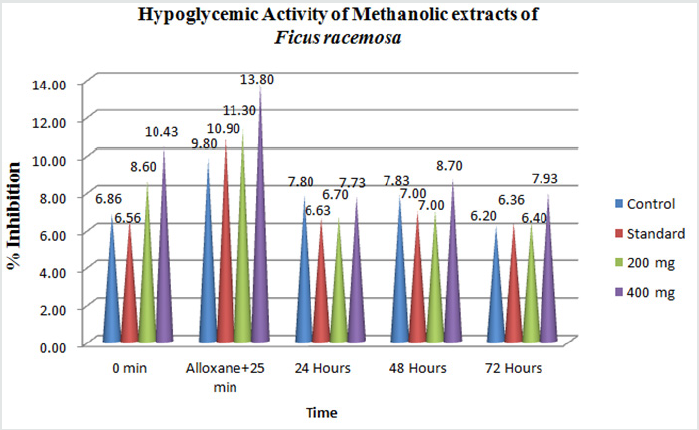
The origin of the term is Greek: “hyper”, meaning excessive; “glyc”, meaning sweet; and “emia”, meaning of the blood Hyperglycemia, or high blood sugar, is a condition in which an excessive amount of glucose circulates in the blood plasma. This is generally a glucose level higher than (120mg/dl) but symptoms may not start to become noticeable until even higher values such as 250-300mg/dl. A subject with a consistent range above 126mg/dl is generally held to have hyperglycemia. Chronic levels exceeding 125mg/dl can produce organ damage [42]. Despite considerable progress in the management of diabetes mellitus by synthetic drugs, the search for improved and safe natural anti-diabetic agents is ongoing. The plant kingdom offers a wide field to look for oral hypoglycemics. More than 400 species have been reported to display hypoglycemic effects, but only few of them have been investigated [43] and the World Health Organization has recommended that this area warrants attention [44]. This study was thus undertaken to evaluate the hypoglycemic effect of a methanolic extracts of Ficus racemosa flowers and their different fractionates.
Anti-diarrheal activity investigation
Diarrhea is characterized by an increase in the frequency of the bowel movements, wet stool, and abdominal pain. It is the world’s third highest killer disease, contributing substantially to pediatric morbidity and mortality, especially in the malnourished. The incidence of diarrhea is still high (about 7.1 million per year), despite the effort of the international organization to control the disease. Thus, in this study, the anti-diarrheal activity was investigated by giving the plant extractives. Here, the plant extractive causes the inhibition of excessive peristaltic movement induced by oral administration of castor oil.
Evaluation of Total Phenolic content (TPC)
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Introduction
Nature has been a source of medicinal agents for thousands
of years and an impressive number of modern drugs have been
isolated from natural sources, many of which are based on their
uses in traditional medicine. Plants produce a diverse array of
bioactive molecules that are particularly important in the treatment
of life-threatening conditions [45]. Oxidation reactions initiated by
excess free radicals have been shown to lead to the formation of
tumors, damage of DNA, mRNA, proteins, enzymes; cause cancer,
cardiovascular diseases, nervous disorders, premature ageing,
Parkinson’s and Alzheimer’s diseases, rheumatic and pulmonary
disorders [46]. Therefore, the need for systematic screening of
medicinal plants for antioxidant activity cannot be overemphasized.
Free radicals are atoms or group of atoms that have at least one
unpaired electron, making them highly reactive. The potentially
reactive derivatives of oxygen are known as reactive oxygen species
(ROS) (e.g. superoxide anions, hydrogen peroxide and hydroxyl,
nitric oxide radicals), and play an important role in oxidative damage
to various biomolecules including proteins, lipids, lipoproteins and
DNA, related to the pathogenesis of various important diseases
such as diabetes mellitus, cancer, atherosclerosis, arthritis, and
neurodegenerative diseases and also in the ageing proces.
Antioxidants are the substance that when present in low concentrations compared to those of an oxidisable substrate significantly delays or prevents oxidation of that substance. Antioxidants prevent the oxidative damage by directly reacting with ROS, quenching them and/or chelating catalytic metal ions and also by scavenging free oxygen. Since ancient times, many herbs have been potentially used as an alternative remedy for treatment of many infections, diseases and as food preservatives suggesting the presence of antimicrobial and antioxidant constituents [47]. There is an increasing interest in the antioxidants effects of compounds derived from plants, which could be relevant in relations to their nutritional incidence and their role in health and diseases [48]. Plants are the potential source of natural antioxidants. Natural antioxidants or phytochemical antioxidants are the secondary metabolites of plants. Carotenoids, flavonoids, cinnamic acids, benzoic acids, folic acid, ascorbic acid, tocopherols, tocotrienols etc., are some of the antioxidants produced by the plant for their sustenance. Beta-carotene, ascorbic acid and alpha tocopherol are the widely used antioxidants.
Different synthetic antioxidant such as tert-butyl-1- hydroxytoluene (BHT), butylated hydroxyanisole (BHA), propyl gallate (PG) and tert-butylhydroquinone (TBHQ) used as food additives to increase shelf life are known to have not only toxic and carcinogenic effects in humans, but abnormal effects on enzyme systems. Therefore, the interest in natural antioxidant, especially of plant origin, has greatly increased in recent years. Plant polyphenols have been studied largely because of the possibility that they might underlie the protective effects afforded by fruit and vegetable intake against cancer and other chronic diseases.
Because of the complex nature of phytochemicals, the antioxidant activities of plant extracts must be evaluated by combining two or more different In-vitro assays. A number of reports on the isolation and testing of plant derived antioxidants have been described during the past decade. The purpose of this study was to evaluate different extractives of roots of Ficus racemosa as new potential sources of natural antioxidants and phenolic compounds.
Assays for total phenolic content
The anti-oxidative effect is mainly due to phenolic components, such as flavonoids, phenolic acids, and phenolic diterpenes. The phenolic compounds exert their antioxidant properties by redox reaction, which can play an important role in absorbing and neutralizing free radicals, quenching singlet and triplet oxygen, or decomposing peroxides. Many phytochemicals possess significant antioxidant capacities that may be associated with lower incidence and lower mortality rates of cancer in several human populations. Phenolic compounds are secondary metabolites of plants and can act as antioxidants by many potential pathways such as free radicalscavenging, oxygen radical absorbance, and chelating of metal ions [49].
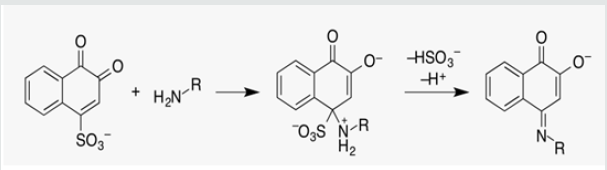
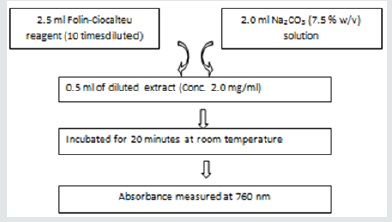
Principle: In the alkaline condition phenols ionize completely. When Folin-Ciocalteu reagent is used in this ionized phenolic solution the reagent will readily oxidize the phenols. Usual color of Folin-Ciocalteu reagent is yellow and after the oxidation process the solution becomes blue. The intensity of the color change is measured in a spectrophotometer at 760nm. The absorbance value will reflect the total phenolic content of the compound [50] (Figure 9).
Materials & Methods: Total phenolic content of root of Phytochemical and biological investigations of Ficusracemosa extractives was measured employing the method as described earlier [51]. involving Folin-Ciocalteu reagent as oxidizing agent and gallic acid as standard [52].
Materials
Folin-Ciocalteu reagent (10-fold diluted) UV-spectrophotometer
Na2CO3 solution (7.5 %) Vial
tert-butyl-1-hydroxytoluene (BHT) Beaker (100 & 200ml)
Ascorbic acid Test tube
Methanol Pipette (1ml)
Chloroform Pipette (5ml)
Carbon tetra chloride Micropipette (50-200 μl)
Pet-ether
Distilled water
Composition of Folin-Ciocalteu reagent [53]

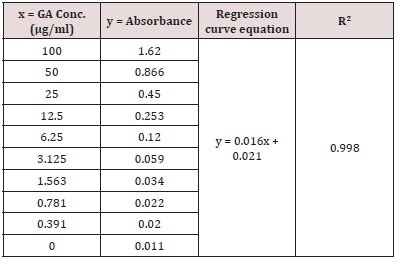
Standard curve preparation: Gallic acid was used here as standard. Different gallic acid solutions were prepared having a concentration ranging from 100μg/ml to 0μg /ml. 2.5ml of Folin- Ciocalteu reagent (diluted 10 times with water) and 2.0ml of Na2CO3 (7.5 % w/v) solution was added to 0.5ml of gallic acid solution. The mixture was incubated for 20 minutes at room temperature. After 20 minutes the absorbance was measured at 760nm. After plotting the absorbance in ordinate against the concentration in abscissa a linear relationship was obtained which was used as a standard curve for the determination of the total phenolic content of the test samples.
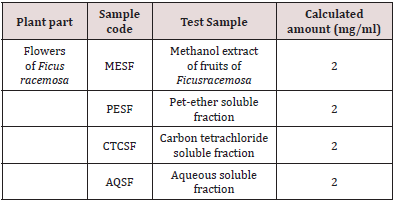
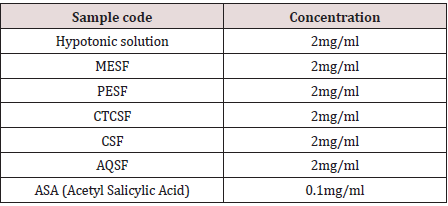
Sample preparation
2mg of the extractives was taken and dissolved in the distilled water to get a sample concentration of 2mg/ml in every case. The samples along with their concentration for the total phenolic content measurement are given in the Table 4.
Total phenolic content analysis
To 0.5ml of extract solution (conc. 2mg/ml), 2.5ml of Folin- Ciocalteu reagent (diluted 10 times with water) and 2.0ml of Na2CO3 (7.5%w/v) solution was added. The mixture was incubated for 20 minutes at room temperature. After 20 minutes the absorbance was measured at 760nm by UV-spectrophotometer and using the standard curve prepared from gallic acid solution with different concentration, the total phenolic content of the samples was measured. The phenolic contents of the sample were expressed as mg of GAE (gallic acid equivalent)/gm of the extract [54] (Figure 10).
Results and discussion of the test samples of fruits of Ficusracemosa
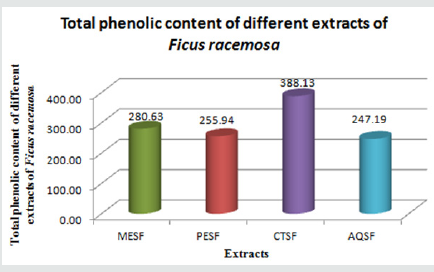
Total phenolic content (TPC)
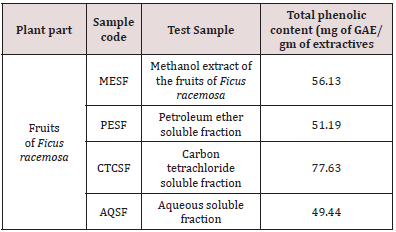
The methanolic extract of Ficus racemosa (MESF) and different
partitionates i.e. petroleum ether (PESF), carbon tetrachloride
(CTCSF), and aqueous (AQSF) soluble partitionates to total phenolic
content determination. Based on the absorbance values of the
various extract solutions, reacted with Folin-Ciocalteu reagent and
compared with the standard solutions of gallic acid equivalents,
results of the colorimetric analysis of the total phenolics are given.
Total phenolic content of the samples is expressed as mg of GAE
(gallic acid equivalent)/gm of extractives.
The amount of total phenolic content differed in different
extractives and ranged from 4mg of GAE /gm of extractives to
25.43mg of GAE/gm of extractives of Ficus racemose. Among all
extractives of Ficus racemosa the highest phenolic content was
found in CTCSF (77.63 mg of GAE /gm of extractives) followed by
AQSF (49.44mg of GAE/gm of extractives).Significant amount of
phenolic compounds were also present in MESF (56.13mg of GAE/
gm of extractives), PESF (51.19mg of GAE/gm of extractives) are
also found (Table 5 & 6) (Figure 11 & 12).
Figure 11: Standard curve of gallic acid for total phenolic content determination (Author’s own work).
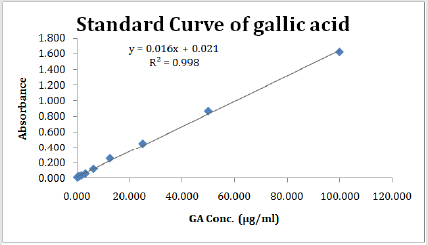
Figure 12: Total phenolic content (mg of GAE/gm of extractives) of different extractives of leaf of Ficus racemosa(Author’s own work).
Antimicrobial Activity
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Introduction
Infectious disease is one of main causes of death accounting
for approximately one-half of all deaths in tropical countries
worldwide. Perhaps, it is not surprising to see these statistics in
developing nations, but what may be remarkable is that infectious
disease mortality rates are actually increasing in developed
countries, such as the United States. Death from infectious disease,
ranked 5th in 1981, has become the 3rd leading cause of death in
1992; an increase of 58%. It is estimated that infectious disease is
the underlying cause of death in 8% of the deaths occurring in the
US [55]. This is alarming given that it was once believed that we
would eliminate infectious disease by the end of the millennium.
The increases are attributed to increases in respiratory tract
infections and HIV/AIDS. Other contributing factors are an increase
in antibiotic resistance in nosicomial and community acquired
infections. Furthermore, the most dramatic increases are occurring
in the 25-44 years old age group [55].
These negative health trends call for a renewed interest in
infectious disease in the medical, public health communities
and renewed strategies on treatment and prevention. It is the
last solution that would encompass the development of new
antimicrobials [56]. The antimicrobial screening which is the first
stage of antimicrobial drug research is performed to ascertain the
susceptibility of various fungi and bacteria to any agent. This test
measures the ability of each test sample to inhibit the in vitro fungal
and bacterial growth. This ability may be estimated by any of the
following three methods [57]. Disc diffusion method-
A. Serial dilution method
B. Bioautographic method
But there is no standardized method for expressing the results
of antimicrobial screening [58]. Some investigators use the diameter
of zone of inhibition and/or the minimum weight of extract to inhibit
the growth of microorganisms. However, a great number of factors
viz., the extraction methods, inoculums volume, culture medium
composition, pH, and incubation temperature can influence the
results [59]. Among the above-mentioned techniques, the disc
diffusion is a widely accepted in vitro investigation for preliminary
screening of test agents which may possess antimicrobial activity
[59]. It is essentially a quantitative or qualitative test indicating the
sensitivity or resistance of the microorganisms to the test materials.
However, no distinction between bacteriostatic and bactericidal
activity can be made by this method [60].
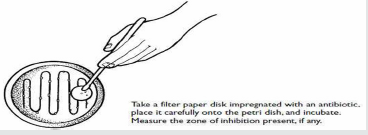
Principle of disc diffusion method
In this classical method, antibiotics diffuse from a confined source through the nutrient agar gel and create a concentration gradient. Dried and sterilized filter paper discs (6mm diameter) containing the test samples of known amounts are placed on nutrient agar medium uniformly seeded with the test microorganisms. Standard antibiotic (Ciprofloxacin) discs and blank discs are used as positive and negative control. These plates are kept at low temperature (4 °C) for 24 hours to allow maximum diffusion of the test materials to the surrounding media [61]. The plates are then inverted and incubated at 37 °C for 24 hours for optimum growth of the organisms. The test materials having antimicrobial property inhibit microbial growth in the media surrounding the discs and thereby yield a clear, distinct area defined as zone of inhibition. The antimicrobial activity of the test agent is then determined by measuring the diameter of zone of inhibition expressed in millimeter [59,61]. In the present study the crude extracts as well as fractions were tested for antimicrobial activity by disc diffusion method. The experiment is carried out more than once and the mean of the readings is required [59].
Experimental
Apparatus and reagents
Filter paper discs Autoclave
Nutrient Agar Medium Laminar air flow hood
Petri-dishes Spirit burner
Sterile cotton Refrigerator
Micropipette Incubator
Inoculating loop Chloroform
Sterile forceps Ethanol
Screw cap test tubes Nose mask and Hand gloves
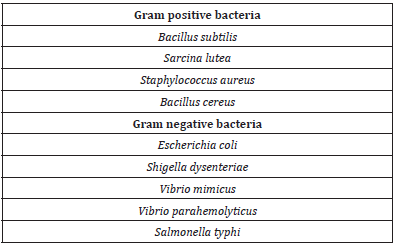
Test organisms
The bacterial and fungal strains used for the experiment were collected as pure cultures from the State University of Bangladesh. Both gram positive and gram-negative organisms were taken for the test and they are listed in the Table 7.
Nutrient agar medium is the most frequently used and also used in the present study for testing the sensitivity of the organisms to the test materials and to prepare fresh cultures.
Preparation of the medium
To prepare required volume of this medium, calculated amount of each of the constituents was taken in a conical flask and distilled water was added to it to make the required volume. The contents were heated in a water bath to make a clear solution. The pH (at 25 °C) was adjusted at 7.2-7.6 using NaOH or HCl. 10ml and 5ml of the medium was then transferred in screw cap test tubes to prepare plates and slants respectively. The test tubes were then capped and sterilized by autoclaving at 15-lbs. pressure at 121°C for 20 minutes. The slants were used for making fresh culture of bacteria and fungi that were in turn used for sensitivity study.
Sterilization procedure
In order to avoid any type of contamination and cross contamination by the test organisms the antimicrobial screening was done in Laminar Hood and all types of precautions were highly maintained. UV light was switched on one hour before working in the Laminar Hood. Petri dishes and other glassware were sterilized by autoclaving at a temperature of 121ºC and a pressure of 15-lbs/ sq. inch for 20 minutes. Micropipette tips, cotton, forceps, blank discs etc. were also sterilized by UV light [62].
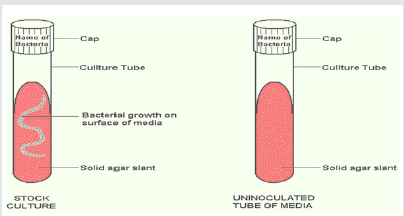
Preparation of subculture
In an aseptic condition under laminar air cabinet, the test organisms were transferred from the pure cultures to the agar slants with the help of a transfer loop to have fresh pure cultures. The inoculated strains were then incubated for 24 hours at 37 °C for their optimum growth. These fresh cultures were used for the sensitivity test (Figure 13).
Preparation of the test plate
The test organisms were transferred from the subculture to the test tubes containing about 10ml of melted and sterilized agar medium with the help of a sterilized transfer loop in an aseptic area. The test tubes were shaken by rotation to get a uniform suspension of the organisms. The bacterial and fungal suspension was immediately transferred to the sterilized petri dishes. The petri dishes were rotated several times clockwise and anticlockwise to assure homogenous distribution of the test organisms in the media (Figure 14).
Figure 14: (a) Preparation of the test plates (b) Freshly prepared culture medium, (c) Pouring culture medium to petridishes, (d) Transfer of bacterial and fungal suspension to the petridishes.
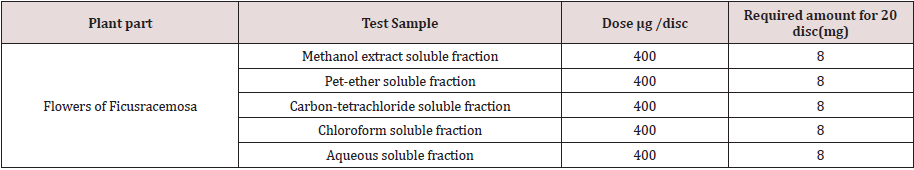
Preparation of discs
Measured amount of each test sample was dissolved in specific volume of solvent (Chloroform or methanol) to obtain the desired concentrations in an aseptic condition. Sterilized metrical (BBL, Cocksville, USA) filter paper discs were taken in a blank petridish under the laminar hood. Then discs were soaked with solutions of test samples and dried (Figure 15) (Table 8).
Standard Ciprofloxacin (50mg/disc) discs were used as positive control to ensure the activity of standard antibiotic against the test organisms as well as for comparison of the response produced by the known antimicrobial agent with that of produced by the test sample. Blank discs were used as negative controls which ensure that the residual solvents (left over the discs even after air-drying) and the filter paper were not active themselves.
Diffusion and incubation
The sample discs, the standard antibiotic discs and the control discs were placed gently on the previously marked zones in the agar plates pre-inoculated with test bacteria and fungi. The plates were then kept in a refrigerator at 4 °C for about 24 hours upside down to allow sufficient diffusion of the materials from the discs to the surrounding agar medium. The plates were then inverted and kept in an incubator at 37 °C for 24 hours.
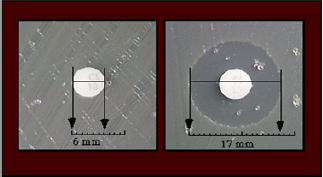
Determination of the zone of inhibition
The antimicrobial potency of the test agents is measured by their activity to prevent the growth of the microorganisms surrounding the discs which gives clear zone of inhibition. After incubation, the Antimicrobial activities of the test materials were determined by measuring the diameter of the zones of inhibition in millimeter with a transparent scale [63] (Figure 16 & 17).
Results and discussion of In vitro antimicrobial screening of Ficusracemosa
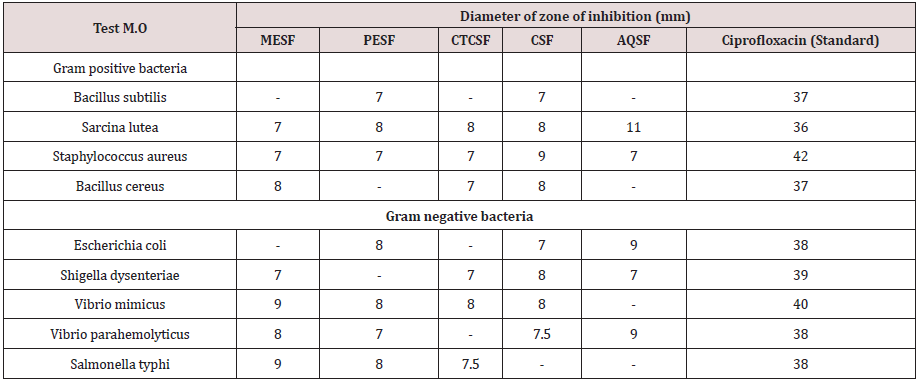
The Methanol extract of leaf of Ficusracemosa (MESF) and different partitionates i.e. Petroleum ether (PESF), carbon tetrachloride (CTCSF), chloroform (CSF) and aqueous (AQSF) soluble partitionate of the methanol extract of leaf of Ficusracemosa were subjected to antimicrobial screening with a concentration of 400 mg/disc in every case. The results are given in the table.
The Aqueous soluble fraction (AQSF) exhibited the highest inhibition against microbial growth having zone of inhibition ranged from 7.0 mm to 11.0 mm. The maximum zone of inhibition produced by AQSF was found to be 11.0 mm against Sarcina lutea (+). This partitionate also showed moderate antibacterial activity against Vibrio parahemolyticus (-), Escherichia coli (-), having zone of inhibition of 9.0mm. The AQSF also exhibited minimum inhibition against microbial growth Staphylococcus aureus (-), Shigella dysenteriae (-), having zone of inhibition 7.0mm.
The Methanolic extract soluble fraction (MESF) also exhibited 2nd highest inhibition against microbial growth having zone of inhibition ranged from 7.0mm to 9.0mm. The maximum zone of inhibition produced by MESF was found to be 9.0mm against Salmonella typhi (-), Vibrio mimicus (-).This partitionate also showed moderate antibacterial activity having zone of inhibition of 8.0mm against Bacillus cereus(+), Vibrio parahemolyticus (-). The MESF also exhibited minimum inhibition against microbial growth Sarcina lutea (+), Staphylococcus aureus (+), Shigella dysenteriae (-) having zone of inhibition 7.50mm.
The chloroform soluble fraction (CSF) exhibited the 3rd highest inhibition against microbial growth having zone of inhibition ranged from 7.0mm to 9.0mm. The maximum zone of inhibition produced by CSF was found to be 9.0mm against staphylococcus aureus (+). This partitionate also showed moderate antibacterial activity having zone of inhibition of 8.0mm against Sarcina lutea, Bacillus cereus (+), Shigella dysenteriae (-), Vibrio mimicus (-).The CSF also exhibited minimum inhibition against microbial growth Vibrio parahemolyticus (-) having zone of inhibition 7.50mm.
The Petroleum ether soluble fraction (PESF) exhibited 4th highest inhibition against microbial growth having zone of inhibition ranged from 7.0mm to 8.0mm. The maximum zone of inhibition produced by PESF was found to be 8.0mm against Sarcina lutea (+), Escherichia coli (-), Vibriomimicus (-), Salmonella typhi (-). The PESF also exhibited minimum inhibition against microbial growth Bacillus subtilis (+), Staphylococcus aureus (+), Vibrio parahemolyticus (-) having zone of inhibition 7.00mm.
The Carbon tetra-chloride soluble fraction (CTCSF) exhibited the 5th highest inhibition against microbial growth having zone of inhibition ranged from 8.0mm to 7.0mm. The maximum zone of inhibition produced by CTCSF was found to be 8.0 mm against Sarcina lutea (+), Vibrio mimicus (-). This partitionate also showed moderate antibacterial activity against Salmonella typhi Staphylococcus aureus (+), Bacillus cereus (+), Shigella dysenteriae (-), having zone of inhibition of 7.5.0mm and exhibited minimum inhibition against microbial growth Staphylococcus aureus (+),Bacillus cereus (+),Shigella dysenteriae having zone of inhibition 7.0mm.
The results of in-vitro microbial screening of flowers of Ficusracemosa indicated that AQSF, MESF, CSF, PESF and CTCSF, possess better antimicrobial activity and these can be further studied to explore potent antimicrobial agents. Besides all these test subjects have significant activity against gram positive and gram-negative bacteria (Table 9).
Membrane Stabilizing Activity
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Introduction
In many of the pathological disorders, inflammation is the one of the important processes. Inflammatory cells produce a complex mixture of growth and differentiation of cytokines as well as physiologically active arachidonate metabolites. In addition, they possess the ability to generate reactive oxygen species (ROS) that can damage cellular biomolecules which in turn augment the state of inflammation [64]. Compounds that possess radical scavenging ability may therefore expect to have the therapeutic potentials for inflammatory disease [65]. The erythrocyte membrane resembles to lysosomal membrane and as such, the effect of drugs on the stabilization of erythrocyte could be extrapolated to the stabilization of lysosomal membrane [40]. Therefore, as membrane stabilizes that interfere in the release and or action of mediators like histamine, serotonin, prostaglandins, leukotrienes etc. [66]. Thus, the aim of the present study was to investigate the anti-inflammatory activity of methanolic extract and its different fractions of fruits of Ficus racemosa.
Materials and Method
Preparation of the extract
Solvent used: Methanol analytical grade (Table 11).
Table 11: Effect of different extractions of Fruits of Ficus racemosa of hypnotic solution induced hemolysis of erythrocyte membrane.
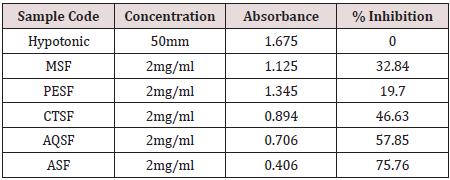
Drug: Standard Acetyl Salicylic Acid (ASA) or Aspirin was used as standard drug for comparison with different methanolic extracts of roots of Ficusracemosa.
Red Blood Cells (RBC) collection: Human RBCs were collected for the study. RBCs collected from the human was male, 70kg, fare complexion and free from diseases. The collected RBCs were kept in a test tube with an anticoagulant EDTA under standard conditions of temperature 23±2 °C and relative humidity 55±10%.
Preparation of phosphate buffer solution: A buffer is an aqueous solution that has a highly stable pH. The buffer was prepared at pH 7 using monosodium phosphate and its conjugate base, disodium phosphate.
Phosphate buffer materials
• Monosodium phosphate
• Disodium phosphate
• Water
• pH meter
• Glassware
• Stirring bar
Calculation of Phosphate buffer
A pH of about 7.4 with buffer strength of 10mM was obtained using 0.0352% monosodium phosphate dehydrate and 0.1099% disodium phosphate anhydrate. The buffer was made by adding 0.352gm monosodium phosphate dehydrate and 1.099gm disodium phosphate anhydrate to 1000mL water.
• pH: 7.4
• Buffer strength: 10.00mM
• Monosodium phosphate, dehydrate: 0.0352%
• Disodium phosphate, anhydrate: 0.1099%
Preparation of isotonic solution
A solution that has a concentration of electrolytes, nonelectrolytes,
or a combination of the two that will exert equivalent
osmotic pressure as that solution with which it is being compared.
Either 0.16M sodium chloride (NaCl) solution (approximately
0.95% salt in water) or 0.3M non-electrolyte solution is
approximately isotonic with human red blood cells.
For the preparation of 500ml isotonic solution of 154mM
strength, 4.5045gm NaCl was added and mixed.
Material for isotonic solution
• Sodium chloride (NaCl)
• Water
• Glassware
• Stirring bar
Calculation for isotonic solution
1000ml solution of strength 1M contain = 58.5gm NaCl
500ml solution of strength 1M contain = 58.5/2gm NaCl
500ml solution of strength 1000mM contain = 58.5/2gm NaCl
500ml solution of strength 154mM contain = 58.5 × 154/2 ×
1000gm NaCl
= 4.5045gm NaCl
Preparation of hypotonic solution
A solution of lower osmotic pressure than that of a reference
solution or of an isotonic solution is called hypotonic solution.
For the preparation of 500ml hypotonic solution, having
strength of 50mM, 1.4625gm NaCl was added and mixed.
Materials for hypotonic solution
• Sodium chloride (NaCl)
• Water
• Glassware
• Stirring bar
Calculation for hypotonic solution
1000ml solution of strength 1M contain = 58.5gm NaCl
500ml solution of strength 1M contain = 58.5/2gm NaCl
500ml solution of strength 1000mM contain = 58.5/2gm NaCl
500ml solution of strength 50mM contain = 58.5 × 50/2 ×
1000gm NaCl
= 1.4625gm NaCl
Effect on hemolysis
Erythrocyte suspension
Whole blood was collected from male human under standard condition. EDTA was used to prevent clotting. The blood was washed three times with isotonic solution (154mM NaCl) in 10mM sodium phosphate buffer (pH 7.4) through centrifuge action for 10min at 3000rpm. Thus, the suspension finally collected was the stock erythrocyte (RBC) suspension.
Hypotonic solution Induced hemolysis
The experiment was carried out with hypotonic solution. The test sample consisted of stock erythrocyte (RBC) suspension(0.5ml) with 5ml of hypotonic solution(50mm NaCl) in 10 mm sodium phosphate buffer saline (pH 7.4) containing either the different methanolic extract (2mg/ml) or acetyl salicylic acid (.1mg/ml). The acetyl salicylic acid was used as reference standard. The mixture was incubated for 10min of room temperature centrifuge for 10min of 3000RPM and the absorbance of the separated was measured of 540nm using shimadzu UV spectrophotometer.
The percentage inhibition of either hemolysis or membrane stabilization was calculated using the following equation.
% inhibition of haemolysis =100× {(OD1-OD2)/OD1}
Where,
OD1= optical density of hypotonic buffered saline solution
alone (control) and
OD2= optical density of the test sample in hypotonic solution.
Result and discussion of the test sample of Ficus racemosa
The different methanolic extracts of the fruits of concentration 2.0mg/ml significantly protected the lysis of human erythrocyte membrane induced by hypotonic solution as compared to the standard acetyl salicylic acid. The roots of Ficus racemosa were effective in the membrane stability activity as the extractive prevented the lysis of erythrocyte induced by hypnotic solution. The methanolic extract (MESF) inhibited 39.84%, petroleum ether soluble fractionate(PESF) inhibited 19.70%, carbon tetrachloride soluble fractionate (CTCSF) inhibited 46.63% and aqueous soluble fractionate (AQSF) inhibited 57.85% for membrane stabilizing activity acetyl salicylic acid was used as standard drug that exhibited 75.76% inhibition of hemolysis of normal condition (Figure 18) (Table 12).
Table 12: Effect of different extraction of fruits of Ficus racemosa of heat induced hemolysis of erythrocyte membrane.
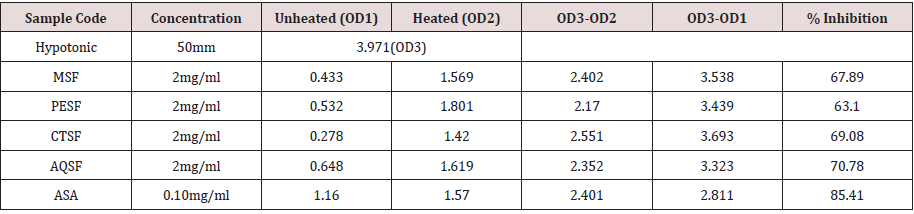
Heat induced hemolysis: Aliquots of the isotonic buffer containing 2mg/ml of different extractive of Ficus racemosa were put into two duplicates of centrifuging tube [66]. The vehicle in the same amounts was added to another tube as control. Erythrocyte suspension (30μl) was added to each tube and mixed gently by inversion. One pair of tubes was incubated at 54 °C for 20min in a water bath. The other pair was maintained of 0-5 °C in an ice bath. The reaction mixture was centrifuged for 10min at 1300RPM and the absorbance of the supernatant was measured at 540nm. The percentage inhibition or acceleration of hemolysis in tests and was calculated according to the equation.
% inhibition of hemolysis= 100× {1-×(OD2-OD1)/(OD3-OD1)}
=100× {(OD3-OD1-OD2+0D1)/(OD3-OD1)}
=100×(OD3-OD2)/(OD3-)D1)
Where,
OD1= test sample unheated
OD2= test sample heated and
OD3= control sample
The different methanolic extracts of the roots of concentration 2.0mg/ml significantly protected the lysis of human erythrocyte membrane induced by heat as compared to the standard acetyl salicylic acid. The fruits of Ficus racemosa were effective in the membrane stability activity as the extractive prevented the lysis of erythrocyte induced by hypnotic solution. The methanolic extract (MESF) inhibited 67.89%, petroleum ether soluble fractionate (PESF) inhibited 63.10%, carbon tetrachloride soluble fractionate (CTCSF) inhibited 69.08% and aqueous soluble fractionate (AQSF) inhibited 70.78% for membrane stabilizing activity acetyl salicylic acid was used as standard drug that exhibited 85.41% inhibition of hemolysis of normal condition (Table 13) (Figure 19).
The effect of synthetic and herbal anti-inflammatory agents on
the stabilization of erythrocyte membrane exposed to hypotonic
solution has been studied extensively. The erythrocyte membrane
resembles to lysosomal membrane and as such, the effect of drugs
on the stabilization of erythrocyte could be extrapolated to the
stabilization of lysosomal membrane. The results showed that the
extracts were potent on human erythrocyte adequately protecting
it against hypotonic induced lysis. The activity was comparable to
that of standard anti-inflammatory drug (Acetyl Salicylic Acid). It
has been reported that flavonoids exert profound stabilizing effects
on lysosomes both in vitro and in vivo experimental animals while
tannin have the ability to bind cations and another biomolecules
and are able to stabilize erythrocyte membrane.
The present investigation suggests that the membrane
stabilizing activity of root of Ficus racemosa plays a significant role
in its anti-inflammatory activity may be due to its high flavonoids
and tannin content.
Evaluation of Thrombolytic Activity
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Introduction
Since ancient periods, herbal preparations have been used for the treatment of several diseases. The leaves and/or twigs, stem, bark and underground parts of plants are most often used for traditional medicines. Herbal products are often perceived as safe because they are “natural” [67]. Cerebral venous sinus thrombosis (CVST) is a common disorder which accompanied by significant morbidity and mortality [68]. Heparin, an anti-coagulating agent, is the first line of treatment for CVST, because of its efficacy, safety and feasibility [69]. Thrombolytic drugs like tissue plasminogen activator (t-PA), urokinase, streptokinase etc. play a crucial role in the management of patients with CVST [70]. Thus, the aim of the present study was to investigate the thrombolytic activity of methanolic extracts and its different fractions of roots of Ficus racemosa.
Materials & Methods
Preparation of sample: The thrombolytic activity of all extractives was evaluated by a method using streptokinase (SK) as standard substance. 10 mg of methanolic extracts and its different fractions of whole plant of Ficus racemosa or were taken in different vials to which 1ml distilled water was added.
Streptokinase (SK): Commercially available lyophilized Altepase (Streptokinase) vial (Beacon pharmaceutical Ltd) of 15, 00,000 I.U., was collected and 5ml sterile distilled water was added and mixed properly. This suspension was used as a stock from which 100μl (30,000 I.U) was used for in vitro thrombolytic.
Blood Sample: Whole blood (n=10) was drawn from healthy human volunteers without a history of oral contraceptive or anticoagulant therapy and 1ml of blood was transferred to the previously weighed sterile vials and was allowed to form clots.
Thrombolytic activity
Aliquots (5ml) of venous blood were drawn from healthy
volunteers who were distributed in ten different pre weighed sterile
vials (1ml/tube) and incubated at 37 °C for 45 minutes. After clot
formation, the serum was completely removed without disturbing
the clot and each vial having clot was again weighed to determine
the clot weight (clot weight = weight of clot containing tube-weight
of tube alone).
To each vial containing pre-weighed clot, 100μl aqueous
solutions of Ficus racemosa different partitionates along with the
crude extracts was added separately. As a positive control, 100μl of streptokinase (SK) and as a negative non thrombolytic control,
100μl of distilled water were separately added to the control vials.
All the vials were then incubated at 37 °C for 90 minutes and
observed for clot lysis. After incubation, the released of fluid was
removed and vials were again weighed to observe the difference
in weight after clot disruption. Difference obtained in weight taken
before and after clot lysis was expressed as percentage of clot lysis
as shown below:
% of clot lysis = (wt of released clot /clot weight) × 100
Results and Discussion of thrombolytic activity of Ficus racemosa
As a part of discovery of cardio protective drugs from
natural sources the extractive of the leaf either assess or not for
thrombolytic activity and results are presented in the table (8.1).
Addition of 100M1SK, a positive control (30000.00) to the clot and
subsequent incubation for 90minutes at 37 °C showed 65.69% lysis
of clot on the other hand distilled water was treated as negative
control which exhibited (10.23%) a negligible percentage between
positive and negative control was found very significant.
In this study, the thrombolytic activity, among all extractives
of rots of Ficus racemosa was found to be negligible. The amounts
of thrombolytic activity were present in Methanol soluble fraction
(MESF 32.91%), Pet-ether soluble fraction (PESF 34.27%), carbon
tetra chloride soluble fraction (CTCSF 30.70%) and dichloromethane
soluble fraction (CSF 38.83%), and Aqueous soluble fraction (AQSF
31.18%) (Table 13).
From this experiment, it can be concluded that the extractives
of Ficusracemosa showed less clot lysis activity than the standard
substance streptokinase (SK) (Figure 20).
Evaluation of Peripheral Analgesic Activity
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Introduction
Inflammation is the response of a tissue and its microcirculation to pathogenic injury. It is characterized by the generation of inflammatory mediators and movement of fluid and leucocytes from the blood into extra vascular tissues which gives rise to the four cardinal signs of inflammation, namely rubor (redness), calor (heat), tumor (swelling) and dolor (pain) as described by Anlus Celsus, the Roman encyclopedist, in the second century AD. Inflammation may be classified into acute, sub-acute and chronic or immunological. There are various mediators for these types of inflammation in different stages, which are histamine, 5-hydroxytryptamine, bradykinin, prostaglandins, leukotrienes, etc
Principle
Peripheral analgesic activity can be evaluated by acetic acid induced writhing method [70,71]. In this method acetic acid is administered intra-peritoneal to the experimental animals to create pain sensation. As a result, the animals squirm their body at regular interval out of pain. This squirm or contraction of the body is termed as “writhing”. As long as the animals feel pain, they continue to give writhing. Each writhing is counted and taken as an indication of pain sensation. Any substance that has got analgesic activity is supposed to lessen the number of writhing of animals within in a given time frame and with respect to the control group. The writhing inhibition of positive control was taken as standard and compared with test samples and control. As positive control, any standard NSAID drug can be used. In the present study, Diclofenac was used as a standard drug [72]. According to this principle the crude methanolic extract of roots of Fecus racemosa was subjected to analgesic testing at two different doses: Dose 200mg/kg and 400mg/kg of body weight.
Experimental animal
Swiss-albino mice of either sex, aged 4-5 weeks, obtained from the Animal Resource Branch of the International Centre for Diarrhoeal Diseases and Research, Bangladesh (ICDDRB) were used for the experiment. They were housed in standard polypropylene cages and kept under controlled room temperature (24 ± 2ºC; relative humidity 60-70%) in a 12h light-dark cycle and fed ICDDR; B formulated rodent food and water (ad-libitum). As these animals are very sensitive to environmental changes, they are kept before the test for at least 3-4 days in the environment where the experiment will take place (Figure 21).
Experimental design
Twelve experimental animals were randomly selected and divided into four groups denoted as group-I, group-II and group- III (A-B) consisting of 3 mice in each group. Each group received a particular treatment. Prior to any treatment, each mouse was weighed properly, and the doses of the test samples and control materials were adjusted accordingly. As it was difficult to observe the biologic response of three mice at a time receiving same treatment, it was necessary to identify individual animal of a group during the treatment. The animals were individualized in the following way and marked as M-1= Mice 1, M-2= Mice 2, M-3= Mice 3 (Figure 22).
Preparation of Test Materials: In order to administer the extract at doses of 400mg/kg body wt and 200mg/kg body wt of mice, the exactly weighed extracts were measured respectively and triturated in unidirectional way by adding of small amount of Tween-80 (a suspending agent). After proper mixing of extract and suspending agent, normal saline was slowly added. The final volume of the suspension was made up to 3.0ml. To stabilize the suspension, it was stirred well by vortex mixture. For the preparation of Diclofenac at the, 50mg of diclofenac was taken and a suspension of dose of 50mg/kg-body weight was made.
Procedure
Figure 23. Schematic representation of procedure for screening of analgesic property.
Counting of licking and biting responses
Each mouse of all groups was observed individually for counting the number of licking and biting responses they made in 5 minutes commencing just after the subcutaneous administration of formalin solution (Figure 24).
Data collection
According to the data that the above table, the Methanolic extracts of leaf of Fecusracemosa at dose of 400mg/kg exhibited significant peripheral analgesic activity and at doses of 200mg/ kg also showed peripheral analgesic activity to a lesser extent compared to Diclofenac Na. Statistical evaluation of the data obtained after the administration of the samples confirmed that the Methanolic extract of roots of Fecus racemosa at doses of 200mg/ kg and 400mg/kg were showed a percent Inhibition of 4.55% and 9.09% respectively. Both data was extremely statistically significant (Figure 25) (Table14-16).
Table 14: Test materials used in the evaluation of analgesic activity of flowers of Fecusracemosa.
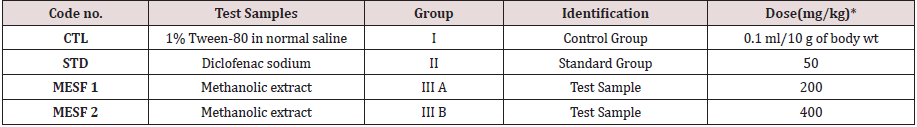
*All doses were given orally. 0.1 ml of 1% acetic acid solution was injected into the peritonial to each mouse.
Table 15: Screening of analgesic activity by counting the time of licking and biting after subcutaneously administration of 5% acetic acid.
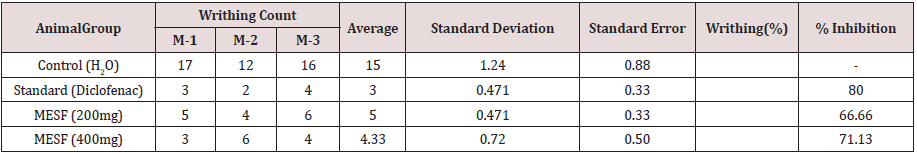
In the table M-1 = mice 1, M-2 = mice 2 and M-3 = mice 3.
According to the data that the above table, the Methanolic extracts of leaf of Fecusracemosa at dose of 400 mg/kg exhibited significant
peripheral analgesic activity and at doses of 200mg/kg also showed peripheral analgesic activity to a lesser extent compared to
Diclofenac Na.
Table 16: Statistical evaluation for the peripheral analgesic activity test.
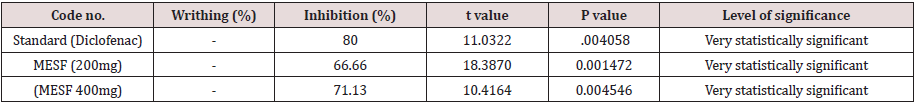
Statistical evaluation of the data obtained after the administration of the samples confirmed that the Methanolic extract of roots of Fecusracemosa at doses of 200mg/kg and 400mg/kg were showed a percent Inhibition of 4.55% and 9.09% respectively. Both data was extremely statistically significant.
Result and Discussion
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
The different test samples were subjected to screening for analgesic activity by acetic acid test. The test was performed by taking samples at doses 200mg/kg and 400mg/kg body weight. The result was statistically evaluated, and the t-test and p values were determined. All the test materials exhibited highly significant peripheral analgesic activity at both the two doses while the crude extract at 400mg/kg dose exhibited maximum inhibition of licking and biting 71.13%.
Evaluation of central Analgesic Activity
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Principle
Evaluation of central analgesic activity was carried by tail immersion method using Morphine as a positive control. The changes in sensitivity of test animal due to analgesic activity of drugs are measured in this method. A constant heat stress is applied to rat tail, which acts as pain stimulus. When the stimulus exceeds the threshold, rat show a quick withdrawal of its tail. Time taken by the rat to withdraw the tail is termed as tail immersion time. Analgesic compound elongates this responding time. By this test discrimination was done between centrally acting morphine –like analgesics and non-opiate analgesics. The test rats were orally fed with test materials whereas the positive control received morphine subcutaneously. From 1-2cm of the tail of mice was immersed in warm water kept constant at 55 °C. The reaction time is the time required by the mice to deflect their tails. The time required to withdraw the tail was recorded.
Experimental animal
Swiss-albino mice of either sex, aged 4-5 weeks, obtained from the Animal Resource Branch of the International Centre for Diarrhoeal Diseases and Research, Bangladesh (ICDDR, B) were used for the experiment. They were housed in standard polypropylene cages and kept under controlled room temperature (24 ± 2ºC; relative humidity 60-70%) in a 12 h light-dark cycle and fed ICDDR, B formulated rodent food and water (ad-libitum). As these animals were very sensitive to environmental changes, they were kept before the test for at least 3-4 days in the environment where the experiment will take place. Food was withdrawn 12 hours before and during the experiment. The ethics for use of experimental animals were followed carefully.
Experimental design
Fifty experimental animals were randomly selected and divided into ten groups denoted as group-I, group-II, group- III(A-B), group- IV(A-B), consisting of 3 mice in each group. Each group received a particular treatment. Prior to any treatment, each mouse was weighed properly, and the doses of the test samples and control materials were adjusted accordingly. As it was difficult to observe the biologic response of three mice at a time receiving same treatment, it was necessary to identify individual animal of a group during the treatment. The animals were individualized in the following way and marked as M1=Mice 1, M2=Mice 2, and M3=Mice 3 (Figure 26).
Materials and equipment
a) Mice holder
b) Feeding needle
c) Syringe
d) Morphine
e) Mice cage
Experimental procedure
Preparation of Test Materials
In order to administer the extract at doses of 400mg/kg body
wt and 200mg/kg body wt of mice, the exactly weighed extracts
were measured respectively and triturated in unidirectional way by
adding of small amount of Tween-80 (a suspending agent). After
proper mixing of extract and suspending agent, normal saline was
slowly added. The final volume of the suspension was made up to 3.0ml. To stabilize the suspension, it was stirred well by vortex
mixture.
Diclofenac-Na (Clofenac Plus of Square Pharmaceuticals Ltd)
was administered orally in the form of solution. The solution was
prepared by diluting the supplied diclofenac-Na (4mg in 10ml) with
saline water. Then diclofenac-Na which ensured a dose of 2mg/kg
for 32mg mice.
Methodology
Test samples and control were given orally by means of a
feeding needle to the mice at zero hour. At zero hour, 1-2cm of
the tail of mice was immersed in warm water kept constant at 55
°C. The reaction time is the time required by the mice to deflect
their tails. The first reading is discarded, and the reaction time is
recorded as a mean of the next three reading. A latency period of 20
seconds was defined as complete analgesia and the measurement
was stopped to avoid injury to mice. The latent period of tail-flick
response was determined before and 0, 30, 60 and 90 minutes
after the administration of drugs. A 30 minute interval was given
to ensure proper absorption of the administered substances.
Then diclofenac-Na solution was administered subcutaneously to
the mice. After 30 minutes, 60 minutes and 90 minutes, the tail
immersion time was measured.
The time for tail immersing of each mouse was recorded and
the average immersing time of each group was calculated. The
% time elongation of tail immersing was calculated in respect to
the control. The higher the elongation percentage of the group
the greater is the group’s central analgesic activity. The central
analgesic activity of the test samples were compared in respect to
diclofenac-Na.
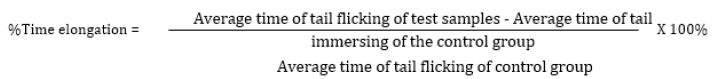
According to the data in the above table the methanol soluble
fraction at dose of 400mg/kg exhibited highly significant central
analgesic activity. The crude extracts at doses of 400mg/kg also
exhibited significant central analgesic activity after 30 minutes
compared to diclofenac Na. The MESF at doses of 200mg/kg also
showed central analgesic activity to a lesser extent.
Statistical evaluation of the data obtained 30 minutes after
the administration of the samples confirmed that the methanolic
extract at doses of 400mg/kg exhibited significant central analgesic
activity. The crude at doses of 200mg/kg showed central analgesic
activity to a lesser extent.
The statistical evaluation of the data showed that the central
analgesic activity of the samples declined after 90 minutes (Figure
27).
Figure 27: Schematic representation for determining blood glucose root of mice after administration of Ficus racemosa extract.
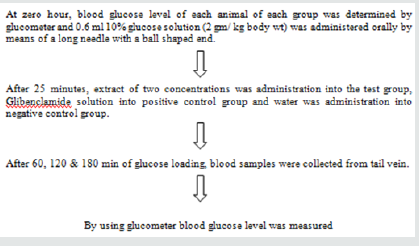
The analysis and statistical evaluation of the data leads to the
following important conclusions.
1. The crude methanol extract has significant central
analgesic activity at 400mg/kg dose.
2. The central analgesic activity is highest after 90 minutes.
3. As the time progress the analgesic activity decreases.
After 90 minutes there is almost no central analgesic activity in
the plant extracts(Table 17-23).
Table 17: Test materials used in the evaluation of central analgesic activity of crude extract and its different fractions of Ficus racemosa.
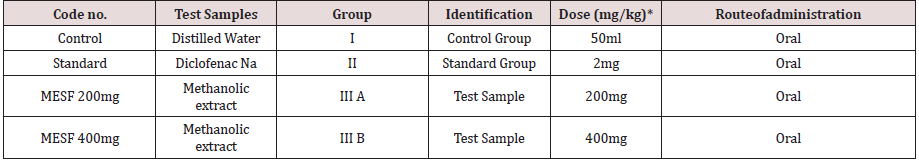
Table 18: Analysis of the data obtained after 30 minutes.
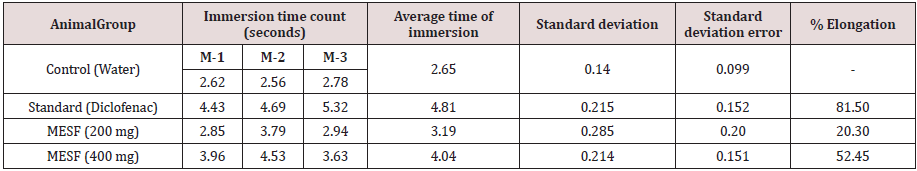
According to the data in the above table the methanol soluble fraction at dose of 400mg/kg exhibited highly significant central analgesic activity. The crude extracts at doses of 400mg/kg also exhibited significant central analgesic activity after 30 minutes compared to diclofenac Na. The MESF at doses of 200mg/kg also showed central analgesic activity to a lesser extent.
Table 19: Statistical Evaluation of the data obtained after 30 minutes.
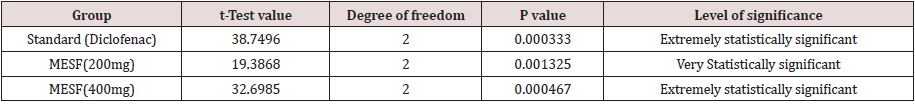
Statistical evaluation of the data obtained 30 minutes after the administration of the samples confirmed that the methanolic extract at doses of 400mg/kg exhibited significant central analgesic activity. The crude at doses of 200mg/kg showed central analgesic activity to a lesser extent.
Table 20: In the table M-1 = mice 1, M-2 = mice 2, M-3 = mice 3
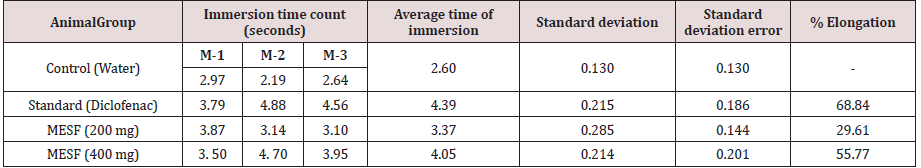
The data in Table: 11.4 showed that after 60 minutes the central analgesic action of Crude Methanol extract at a dose of 400mg/kg became stronger. They showed a percent elongation of 55.77% and 29.61% at a dose of 400mg and 200mg/kg bode weight. But the central analgesic activity of aqueous soluble fraction at 400mg/kg dose still remains highly significant after 60 minutes.
Table 21: Statistical Evaluation of the data obtained after 60 minutes.
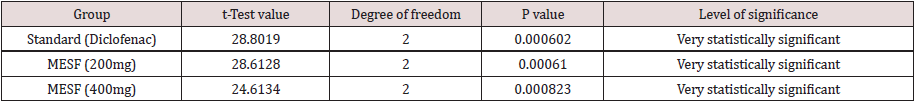
In the table M-1 = mice 1, M-2 = mice 2, M-3 = mice 3
The data in Table: 11.6 showed that after 90 minutes the central analgesic action of Crude Methanol extract at a dose of 400mg/kg
became stronger. It showed a percent elongation of 71.06%. At a dose of 200mg/kg showed a percent elongation of 54.46%.
Table 23: Statistical Evaluation of the data obtained after 90 minutes.
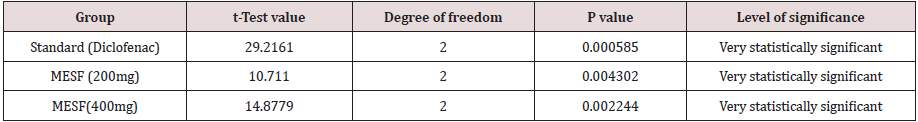
The statistical evaluation of the data showed that the central analgesic activity of the samples declined after 90 minutes.
Evaluation of Hypoglycemic Activity
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
Principle
Diabetes mellitus is the most common endocrine disorder in
men and women and the major public health problem of epidemic
proportion. Once believed to be a disease of west, it is becoming
an endemic to modernizing and urbanizing population in our
country. Ayurvedic literature reveals that many herbal medicines
in different oral formulation have been shown to comprise potent
hypoglycemic activity and therefore recommended in madhumeha
(diabetes mellitus) and confident claims of cure are on record. A
glucose tolerance test (GTT) is one of the most acceptable methods
to evaluate the hypoglycemic activity. It is a medical test in which
glucose is given and blood samples taken afterward to determine
how quickly it is cleared from the blood. The test is usually used
to test for diabetes, insulin resistance, and sometimes reactive
hypoglycemia or rarer disorders of carbohydrate metabolism. Many
variations of the GTT have been devised over the years for various
purposes, with different standard doses of glucose, different routes
of administration, different intervals and durations of sampling,
and various substances measured in addition to blood glucose.
At the present study, hypoglycemic effect of methanolic extract
of roots of Ficusracemosa at 250mg/kg and 500mg/kg doses were
examined & compared with relative to that of control and standard
group. Here Glibenclamide was used as a standard drug.
Experimental animal
Swiss-albino mice of either sex, aged 4-5 weeks, obtained from the Animal Resource Branch of the International Centre for Diarrhoeal Diseases and Research, Bangladesh (ICDDR, B) were used for the experiment. They were housed in standard polypropylene cages and kept under controlled room temperature (24 ± 2 ºC; relative humidity 60-70%) in a 12h light-dark cycle and fed ICDDR; B formulated rodent food and water (ad-libitum). As these animals are very sensitive to environmental changes, they are kept before the test for at least 3-4 days in the environment where the experiment will take place.
Experimental design
Twelve experimental animals were randomly selected and divided into ten groups denoted as group-I, group-II, group-III (A), and group- III (B) consisting of 3 mice in each group. Each group received a particular treatment. Prior to any treatment, each mouse was weighed properly and the doses of the test samples and control materials were adjusted accordingly. As it was difficult to observe the biologic response of three mice at a time receiving same treatment, it was necessary to identify individual animal of a group during the treatment. The animals were individualized in the following way (Figure 13.3) and marked as M-1=Mice 1, M-2=Mice 2, and M-3=Mice 3.
Preparation of Test Materials
In order to administer the extract at doses of 400mg/kg body wt and 200mg/kg body wt of mice, the exactly weighed extracts were measured respectively and triturated in unidirectional way by adding of small amount of Tween-80 (a suspending agent). After proper mixing of extract and suspending agent, normal saline was slowly added. The final volume of the suspension was made up to 3.0ml. To stabilize the suspension, it was stirred well by vortex mixture. For the preparation of standard (Glibenclamide) at the dose of 10mg/kg body weight, 10mg tablet was dissolved into 3.0ml distilled water.
Procedure
(Figure 28) (Table 24-27)
Table 24: Test materials used in the evaluation of hypoglycemic activity of crude extract and its different fractions of Ficus racemosa.
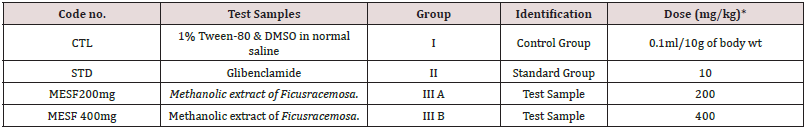
Result & Discussion of hypoglycemic activity of test materials of Ficus racemosa
The effects of methanolic extract of stem roots of Ficus racemosa at 200 and 400mg/kg dose and its different fractionates at 200mg/kg doses to lower blood glucose level were observed as follows to evaluate their hypoglycemic activity (Figure 29).
The methanolic extrat of roots of Ficus racemosa has statistically significant blood glucose lowing activity at dose of 400mg/kg. But significant hypoglycemic activity was exhibited by any other test subject. So, it can be concluded that the crude methanolic extract possesses moderate hypoglycemic activity at 400mg.
Conclusion
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
All the conducted experiments in the present study which are based on not only cured extract but also many different kinds of soluble frictions are considered to be initially and more sophisticate research is important to gain a concrete conclusion about the findings of the present study. It can be concluded from the above findings, the plant Ficus recaemosa have moderate to significant thrombolytic, membrane stabilizing, antioxidant, antimicrobial, analgesic and hypoglycemic activity. So, further scientific studies are necessary to explain detailed not only mechanism of action but also isolation the responsible active principles.
References
- Abstract
- Introduction
- Plant Preview
- Preparation of Plant Extract
- Design of Biological Investigation
- Results & Discussions
- Evaluation of Total Phenolic content (TPC)
- Antimicrobial Activity
- Membrane Stabilizing Activity
- Evaluation of Thrombolytic Activity
- Evaluation of Peripheral Analgesic Activity
- Result and Discussion
- Evaluation of central Analgesic Activity
- Evaluation of Hypoglycemic Activity
- Conclusion
- References
- Mendoza N, Silva EME (2018) Introduction to Phytochemicals: Secondary Metabolites from Plants with Active Principles for Pharmacological Importance. Phytochemicals-Source of Antioxidants and Role in Disease Prevention. doi:10.5772/intechopen.78226.
- Newman DJ, Cragg GM, Snader KM (2003) Natural Products as Sources of New Drugs over the Period 198-2002. Journal of Natural Products66(7):1022-1037. doi:10.1021/np030096l.
- Farnsworth, Norman R, Akerele, Olayiwola, Bingel, et al. (1985) Medicinal plants in therapy. Bulletin of the World Health Organization 63(6): 965-981.
- Fabricant DS, Farnsworth NR (2001) The Value of Plants Used in Traditional Medicine for Drug Discovery. Environ Health Perspect 109: 169. doi:10.2307/3434847.
- Cox PA, Balick MJ (1994) The Ethnobotanical Approach to Drug Discovery. Scientific American 270(6):82-87. doi:10.1038/scientificamerican0694-82.
- Balunas MJ, Kinghorn AD (2005) Drug discovery from medicinal plants. Life Sci 78(5):431-441. doi:10.1016/j.lfs.2005.09.012.
- Lietava J (1992) Medicinal plants in a Middle Paleolithic grave Shanidar IV.JEthnopharmacol35(3):263-266. doi:10.1016/0378-8741(92)90023-k.
- Hostettmann K, Marston A (2007) The Search for New Drugs from Higher Plants. CHIMIA International Journal for Chemistry61(6):322-326. doi:10.2533/chimia.2007.322.
- Fabricant DS, Farnsworth NR (2001) The value of plants used in traditional medicine for drug discovery. Environ Health Perspect. 109 Suppl 1(Suppl 1):69-75. doi:10.1289/ehp.01109s169.
- Prance GT (1978) Endangered Plants of the USA Endangered and Threatened Plants of the United States. In: Edward S,Ayensu Robert A,DeFilipps (Edt.),BioScience28(9):598-598. doi:10.2307/1307523.
- Goldberg A, Cronquist A (1982) An Integrated System of Classification of Flowering Plants. Taxon31(3):599. doi:10.2307/1220703.
- Tippo O, Stern WL (1977) Humanistic Botany.W.W. Norton, New York, USA.
- Verpoorte R (2000) Pharmacognosy in the New Millennium: Leadfinding and Biotechnology. J Pharm Pharmacol. 52(3):253-262. doi:10.1211/0022357001773931.
- Vagelos P (1991) Are prescription drug prices high? Science.252(5009):1080-1084. doi:10.1126/science.252.5009.1080.
- Abegaz BM, Ngadjui BT, Bezabih M, Mdee LK (1999) Novel natural products from marketed plants of eastern and southern Africa. Pure and Applied Chemistry 71(6):919-926. doi:10.1351/pac199971060919.
- Singh R (2015) Medicinal Plants: A Review. Journal of Plant Sciences. Special Issue: Medicinal Plants. 3(1-1):50-55. doi: 10.11648/j.jps.s.2015030101.18.
- O SAE (2015) Medicinal Importance of Herbs & Spices. Medicinal & Aromatic Plants 04(04). doi:10.4172/2167-0412.1000e160.
- Ghani A, Pasha MK (2004) Alternative Medicine. Banglapedia [CD-ROM]. Version: English. Dhaka. Asiatic Society of Bangladesh.
- Samy RP, Pushparaj PN, Gopala Krishna Koné P (2008) A compilation of bioactive compounds from Ayurveda. Bioinformation3(3):100-110. doi:10.6026/97320630003100.
- Mohiuddin, Abdul Kader (2019) A Brief Review of Traditional Plants as Sources of Pharmacological Interests. Open Journal of Plant Science pp. 001-008. doi:10.17352/ojps.000015.
- Hoque MM, Hassan MA, Khan MR (1986) Studies in the antibacterial activity of plants available in Bangladesh 1.Ploigonum LJ (Edt.), Asiatic society of Bangladesh (Sc). 12(1):77-82.
- Harvey A (2008) Natural products in drug discovery. Drug Discovery Today 13(19-20):894-901. doi:10.1016/j.drudis.2008.07.004.
- Mukherjee PK, Rai S, Kumar V, Mukherjee K, Hylands P, et al. (2007) Plants of Indian origin in drug discovery. Expert Opin Drug Discov2(5):633-657. doi:10.1517/17460441.2.5.633.
- GM Cragg, DJ Newman (2001) Natural Product Drug Discovery in the Next Millennium. Pharm Biol 39(1):8-17. doi:10.1076/phbi.39.7.8.5868.
- Petrovska BB (2012) Historical review of medicinal plants' usage. Pharmacogn Rev6(11):1-5. doi:10.4103/0973-7847.95849.
- Shah SK, Garg G, Jhade D, Pandey H (2016)Ficusracemosa Linn: Its Potentials Food Security and Rural Medicinal Management. J. Pharm. Sci. & Res. 8(5):317-322.
- Shah SK (2016) Evaluate the Antifertility Potential of Ficusracemosa Linn Bark in Female Wistar Rats. Asian Journal of Pharmaceutical and Clinical Research. 9(6):322. doi:10.22159/ajpcr.2016.v9i6.14517.
- Rao RB, Anupama K, Swaroop KA, Murugesan T, Pal M, et al. (2002) Evaluation of anti-pyretic potential of Ficusracemosa Phytomedicine9(8):731-733. doi:10.1078/094471102321621340.
- Wu ZY, Lu AM, Tang YC, Chen ZD, Li DZ (2003) The families and genera of angiosperms in China: A comprehensive analysis. Beijing: Science Press.Ficusracemosa L. Sp. Pl. 1060 (1753).
- KK, An A (2018) The Phytoconstituents and Pharmacological Actions of Ficusracemosa Linn (Family: Moraceae)-An updated review. PharmaTutor.6(12):55. doi:10.29161/pt.v6.i12.2018.55.
- Taxonomic Descriptionofethnobotanical Plants.
- Jassal PS, Sharma M (2019) Evaluation of Antioxidant, Antibacterial, Antihemolytic, And Phyochemical Properties of FicusBenjamina, FicusInfectoria, And FicusKrishnae. Asian Journal of Pharmaceutical and Clinical Research 12(3): 68-73. doi:10.22159/ajpcr.2019.v12i3.25351.
- Amit K Keshari, Ghanendra Kumar, Priya S Kushwaha, Monika Bhardwaj, Pranesh Kumar, et al. (2016) Isolated flavonoids from Ficusracemosa stem bark possess antidiabetic, hypolipidemic and protective effects in albino Wistar rats. J Ethnopharmacol. 181:252-262. doi:10.1016/j.jep.2016.02.004.
- Collee JG, Miles RS, Watt B (1996) Tests for identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A (eds.), Mackie and McCartney Practical Medical Microbiology, 14th(edn), Churchill Livingstone, New York, USA pp. 131-149.
- VanWagenen BC, Larsen R, Cardellinall JH, Randazzo D, Lidert ZC, et al. (1993)Ulosantoin, a potent insecticide from the sponge Ulosaruetzleri. J. Org. Chem. 58: 335-337.
- Farnsworth NR (2007) Ethnopharmacology and Drug Development. Novartis Foundation Symposia 42-59. doi:10.1002/9780470514634.ch4.
- Atanasov AG, Waltenberger B, Pferschy-Wenzig EM, Thomas Linder, Christoph Wowrosh, et al. (2015) Discovery and resupply of pharmacologically active plant-derived natural products: A review. Biotechnol Adv. 33(8):1582-1614. doi:10.1016/j.biotechadv.2015.08.001.
- Reuter S, Gupta SC, Chaturvedi MM, Aggarwal BB (2010) Oxidative stress, inflammation, and cancer: how are they linked. Free Radic Biol Med49(11):1603-1616. doi:10.1016/j.freeradbiomed.2010.09.006.
- James O (2016) Phytoconstituents, nutritional, antioxidant and toxicological study on Cissusmultistriata plant extract. Planta Medica81(S 01). doi:10.1055/s-0036-1596889.
- (2012) Antioxidant and Anti-Inflammatory activity of Synthesized 3(Substituted) Chromen-2-One. International journal of pharmaceutical sciences and research. 3(2). doi:10.13040/ijpsr.0975-8232.3(2).474-78.
- American Diabetes Association (2009) Diagnosis and classification of diabetes mellitus. Diabetes Care 32 Suppl 1(Suppl 1):S62-S67. doi:10.2337/dc09-S062.
- Maraia FE, Naema MSE, Nura NM, Mona AM (2017) Anti-Diabetic Activity of Methanolic Extract of Grape Seeds in Alloxan Induced Diabetic Rats. Agri Res & Tech: Open Access J. 6(5): 555699. DOI:10.19080/ARTOAJ.2017.06.555699.
- WHO (2002)Traditional Medicine strategy 2002-2005, World Health Organization, Geneva,p.74.
- Maclaughlin JL, Anderson JE, Rogers,Lingling L (1998) Drug Info Journal 32: 513-524.
- BakerW, vandenBroekA, CamonE, Hingamp P, Sterk P, et al.(2000) The EMBL Nucleotide Sequence Database Nucl Acid Res (2000) 28(1): 19-23.
- Tepe B, Daferera D, Sökmen M, Polissiou M, Sökmen A (2004) In Vitro Antimicrobial and Antioxidant Activities of the Essential Oils and Various Extracts ofThymuseigiiM. Zohary et P.H. Davis. J AgricFood Chem 52(5):1132-1137. doi:10.1021/jf035094l.
- Kasote DM, Katyare SS, Hegde MV, Bae H (2015) Significance of antioxidant potential of plants and its relevance to therapeutic applications. International journal of biological sciences 11(8):982-991. doi:10.7150/ijbs.12096.
- Kumar S, Pandey AK (2013) Chemistry and Biological Activities of Flavonoids: An Overview. Scientific World Journal 2013:1-16. doi:10.1155/2013/162750.
- Hatami T, Emami SA, Miraghaee SS, Mojarrab M (2014) Total Phenolic Contents and Antioxidant Activities of Different Extracts and Fractions from the Aerial Parts of Artemisia biennisWilld. Iran J Pharm Res13(2):551-559.
- Rajvaidhya S, Byahatti VV (2019)In-Vitro Antioxidant Activity of Various Extracts of Bark of Ficus Racemosa Linn. (MORACEAE). International Journal of Pharmaceutical Sciences and Research 10(3): 1534-1539 doi:10.13040/ijpsr.0975-8232.10(3).1534-39.
- Everette JD, Bryant QM, Green AM, Abbey YA, Wangila GW, et al. (2010) Thorough study of reactivity of various compound classes toward the Folin-Ciocalteu reagent. J Agric Food Chem58(14):8139-8144. doi:10.1021/jf1005935.
- Sultana J, Kabir A, Hakim MA, Abdullah M, Islam N, Reza MA (2013) Evaluation of the Antioxidant Activity of Ficusracemosa Plant Extracts from North-Western District of Bangladesh. Journal of Life and Earth Science8:93-99. doi:10.3329/jles.v8i0.20152.
- Pinner R, Teutsch S, Simonsen L, Klug L, Graber J, et al. (1996) Trends in infectious diseases mortality in the United States. JAMA 275(3):189-193.
- Fauci AS(1998) New and reemerging diseases: The importance of biomedical research. Emerg Infect 4(3): 374-378.
- Ayafor JF (1972) Tetrahedron 28:9343.
- Balouiri M, Sadiki M, Ibnsouda SK (2016) Methods for in vitro evaluating antimicrobial activity: A review. Journal of Pharmaceutical Analysis6(2):71-79. doi:10.1016/j.jpha.2015.11.005.
- Bayer AW, Kirby WMM, Sherris JC, Turck M (1966) Antibiotic susceptibility testing by a standardized single disc method, Am J Clin Pathol 45(4): 493-496.
- Nishat S (2008) Synthesis and Characterization of Organophosphorus Compounds Composed of Diamino Functionalities and Study of Their Biological Activity 1:138.
- Barry AL (1976) Principle & practice of Microbiology. 3rd(edn.), Lea &Fabager, Philadelphia, USA.
- Roy DN, Azad AK, Sultana F, Anisuzzaman ASM (2016) In-vitroantimicrobial activity of ethyl acetate extract of two common edible mushrooms.The Journal of Phytopharmacology 5(2):79-82.
- Hudzicki J (2009) Kirby-Bauer Disk Diffusion Susceptibility Test Protocol.
- Nita M, Grzybowski A (2016) The Role of the Reactive Oxygen Species and Oxidative Stress in the Pathomechanism of the Age-Related Ocular Diseases and Other Pathologies of the Anterior and Posterior Eye Segments in Adults. Oxid Med Cell Longev1-23. doi:10.1155/2016/3164734.
- Kurutas EB (2016) The importance of antioxidants which play the role in cellular response against oxidative/nitrosative stress: current state. Nutr J 15(1):71. doi:10.1186/s12937-016-0186-5.
- Salemcity A, Attah A, Oladimeji O, Olajuyin A, Usifo G, et al. (2016) Comparative study of membrane-stabilizing activities of kolaviron Dryopteris filix-mas and Ocimumgratissimum Egyptian Pharmaceutical Journal15(1):6 doi:10.4103/1687-4315.184026.
- Abdulkhaleq LA, Assi MA, Abdullah R, Zamri-Saad M, Taufiq-Yap YH, et al. (2018) The crucial roles of inflammatory mediators in inflammation: A review. Vet World 11(5):627-635. doi:10.14202/vetworld.2018.627-635.
- Kigen G, Kipkore W, Wanjohi B, Haruki B, Kemboi J (2017) Medicinal Plants Used by Traditional Healers in Sangurur, Elgeyo Marakwet County, Kenya. Pharmacognosy Res9(4):333-347. doi:10.4103/pr.pr_42_17.
- Patil VC, Choraria K, Desai N, Agrawal S (2014) Clinical profile and outcome of cerebral venous sinus thrombosis at tertiary care center. J Neurosci Rural Pract5(3):218-224. doi:10.4103/0976-3147.133559.
- Sun J, He Z, Nan G (2018) Cerebral venous sinus thrombosis presenting with multifocal intracerebral hemorrhage and subarachnoid hemorrhage: A case report. Medicine (Baltimore)97(50):e13476. doi:10.1097/MD.0000000000013476.
- Prasad S, Kashyap RS, Deopujari JY, Purohit HJ, Taori GM, et al. (2006) Development of an in vitro model to study clot lysis activity of thrombolytic drugs. Thromb J4:14doi:10.1186/1477-9560-4-14.
- Gawade SP (2012) Acetic acid induced painful endogenous infliction in writhing test on mice. J PharmacolPharmacother3(4):348. doi:10.4103/0976-500X.103699.
- Munira M, Islam S, Akther N, SabihaFerdowsyKoly (2019) Estimation of anti-inflammatory, analgesic and thrombolytic activities of Sonneratiacaseolaris Linn. (Family: Sonneratiaceae). J Anal Pharm Res. 8(1):20?23. DOI: 10.15406/japlr.2019.08.00305.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...