Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1217
Review ArticleOpen Access
Life Course In HEARTS: Enhancing Telehealth Resilience and Mindfulness Intervention in Older Adults Experiencing Abuse and Trauma-A Conceptualization Volume 3 - Issue 1
Rose Eva Constantino1*, Andrew Thomas Reyes2, Paul Wesley Scott3, Jennifer Petrie-Wyman4, Suzanne Carmack5, Mary Dioise Ramos6, Balaji Palanisamy7, Pearl Ed G. Cuevas8, Harmeet Kaur Kang9, Daisy R. Palompon10, Vivian Hui11, Rebecca Elizabeth Burkart12, And Larissa Catherine Allen12
1School of Nursing, University of Pittsburgh, USA
2School of Nursing, University of Nevada Las Vegas, USA
3School of Nursing, University of Pittsburgh, USA
4Assistant Director, Joseph M. Katz Graduate School of Business, University of Pittsburgh, USA
5George Mason University Fairfax, USA
6WellStar School of Nursing, Kennesaw State University, USA
7School of Computing and Information, University of Pittsburgh, USA
8School of Nursing, Centro Escolar University, Philippines
9Chitkara School of Health Sciences, Chitkara University, Punjab, India
10Cebu Normal University, Philippines
11Graduate Researcher School of Nursing, University of Pittsburgh, USA
12Graduate Assistant, School of Nursing, University of Pittsburgh, USA
Received: May 13, 2021 Published: May 25, 2021
*Corresponding author: RE Constantino, School of Nursing, University of Pittsburgh, Pittsburgh, Pennsylvania, USA
Introduction
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
Advances in research and evidence-based practice improve the prevention and treatment of diseases, but the marginalized seems to be left behind [1]. The purpose of this paper is to conceptualize a telehealth intervention aimed to improve the health and health span of older adults. More particularly, we articulate the conceptual framework underlying our intervention, Telehealth Resilience Mindfulness (TRM) Intervention, which will be delivered via text messaging (for those who have phones or smartphones), video conferencing such as Zoom (for those with internet connectivity), or in-person (when it is practical) to older adults to enhance HEARTS (health, experiences of abuse and trauma, resilience, technology use, and social support). Healthcare is a human right a resource to mitigate disparities in healthspan, defined as the portion of life spent in good health [2]-enriching opportunities if there is collaboration in interdisciplinary education, research, and practice [1,3]. We propose a telehealth intervention as a resource for older adults in mitigating disparities in healthspan. A telehealth intervention is defined as the use of information and communication technologies for health that encompasses positive emotions, optimism, and cognitive appraisal [4-7]. Telehealth interventions have the potential to reduce the psychobiological exposure to abuse and trauma and their health-related consequences as technology provides a safe, timely, and flexible space for the target population compared with traditional face-to-face approaches [7]. Additionally, interventions for the prevention and reduction of abuse among women [8-11] had positive health and social outcomes. Some telehealth interventions were included in these reviews and showed mixed results [7,12]. For these reasons, we are exploring and conceptualizing opportunities for enhancing the feasibility and efficacy of the telehealth resilience-mindfulness intervention in older adults.
.Our overall objective is to expand causal pathways underlying successful aging using PROMIS health indicators predictive modeling to examine how the HEARTS outcomes by environment interaction in telehealth resilience mindfulness intervention impact healthspan [13]. The telehealth resilience mindfulness intervention could improve health outcomes and increase healthspan delivering it by text messaging, videoconferencing (e.g., Zoom), or in-person (when possible). Once conceptualized, we will test specifically the feasibility and efficacy of the HEARTS telehealth resilience and mindfulness intervention by linking objective tests with subjective tests of health variables and the biobehavioral attributes of resilience in a future study. We will hypothesize that the intervention promotes better health outcomes, openness in sharing experience of abuse and trauma, enhance resilience, and social support. Our long-term goal is to establish a research infrastructure for interprofessional collaboration that expands the evidence-based biobehavioral telehealth resilience interventions and to improve healthspan (the portion of life spent in good health) by linking biobehavioral attributes of resilience with technology use, and social support through predictive modeling technique. The establishment of an infrastructure for interdisciplinary collaboration globally will expand the biobehavioral evidencebased telehealth resilience mindfulness intervention increasing healthspan.
Today’s telehealth nursing care approaches can serve a wide range of populations and make a significant contribution to the efficacy and delivery of health care. However, there is a lack of research data to support the readiness for adopting the use of telehealth interventions among a wide variety of clinical situations, with diverse patients, and in a variety of settings. By examining the feasibility and efficacy of HEARTS Telehealth Resilience Mindfulness (TRM) Intervention among older adults, we will explore older adults’ readiness for adopting the use of technologybased interventions to improve their health and healthspan. For a future study, we ascend to De Los Reyes’s [14] suggestion that a theoretical model framework (Range of Possible Changes [RPC] Model) to conceptualize, examine, and classify the available evidence for interventions. We will adopt the RPC Model to theorydriven hypotheses and conduct a mixed-methods design to test whether the telehealth resilience mindfulness intervention may or may not change biopsychological constructs for older adults who have experienced abuse and trauma.
Significance
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
The older adult population is growing faster than all younger age groups as their healthspan (a portion of life spent in good health) is decreasing. Globally, one in six people of 60 years and older experienced abuse in their homes, community, and institutional settings every year, and the annual loss by victims of financial abuse is estimated to be at least $36.5 billion [15]. The experience of abuse robs older adults of their dignity, security, healthspan, and in some cases, their lives, leaving a stubborn imprint as they age [13,15-17]. Elder abuse and history of abuse include physical, emotional, sexual, economic, and neglect [15,18]. The risks of leaving the experience of abuse and its consequences unmitigated are devastating to the survivor (personally), family (interpersonally), and community [19].
Preliminary studies suggest that experiencing abuse exacerbates the risks for health indicators, resilience, social support, and technology use a psychosocial impact on the healthspan of older adults [20,21]. It is imperative to determine the socio-behavioral mechanisms that account for older adult’s health disparities related to their experiences of abuse, resilience, technology use, and social support. Social determinants of health are rooted in a system of structuring opportunity and assigning value based on the social interpretation of how young the person is, and it unfairly disadvantages individuals and communities, sapping the strength of persons through the waste of human resources [3,22]. We have accepted that during this pandemic, that distancing, quarantines, and social isolation, are perfect deterrents for the COVID-19 virus to spread, however, it is a risky practice in caring for older adults. The socio-behavioral interventions such as social support [23], and self-efficacy and behavioral therapies [24] throughout the lifecourse are known but certain forms of interventions that enhance biobehavioral attributes of resilience facilitating reappraisal and promote social support preserving a sense of purpose in the face of abuse are not well developed [6,25]. There is a critical need to explore the biobehavioral processes associated with telehealth resilience and mindfulness intervention using objective tests and subjective tests [12,25-26].
Conceptual Framework
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
The Life Course Health Development (LCHD) framework [27,28] provides the theoretical foundation of our conceptualization of health and health trajectory of our target population in our research - the older adults with experience of abuse and trauma. The LCHD constitutes comprehensive biological, social, and environmental aspects of health that influence health outcomes later in life [27]. The conceptual foundation of LCHD came when Elder [29] developed an integrated ecological systems model examining changing life trajectories by leveraging contextual effects that accumulate over time and influence the individual’s trajectory. There are six key tenets of the LCHD framework, all predicated by health: 1) health is a set of capacities that develops over time (older adults); 2) health constantly develops by interactions between biology (health), and environment (social support, technology use); 3) health involves a complex, non-linear system over several dimensions, phases, and levels; 4) health is responsive to the social structuring and timing of ecological experiences (experience of abuse); 5) health has an evolving process that uses resilience and plasticity to adapt to changing ecological contexts; and 6) health is responsive to the timing and synchronization of the level of ecological pathways (personal, interpersonal, community, and society), with molecular to biological to social and cultural functions [28]. We are using these tenets with a focus on the ecological pathways and integrating health, experience of abuse, resilience, technology use, and social support.
Literature Review
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
The socio-behavioral interventions in abuse throughout the life course are known but certain forms of interventions that enhance biobehavioral attributes of resilience facilitating reappraisal and promote mindfulness preserving a sense of purpose in the face of abuse are not well developed [6,25,30]. There is a critical need to explore the changes and biobehavioral processes associated with telehealth resilience-mindfulness intervention that has biopsychosocial underpinnings of resilience [6].
The Health of Older Adults
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
Despite improvements in current approaches to an aging population, the health of older adults is not keeping up with increasing longevity [31,32]. Older adults contribute to society in diverse ways - through their family, community, and society. The extent of their contributions to society depends on their health. One major challenge in assessing the health of older adults is the sheer diversity of health and functional states they experience that are loosely associated with chronological age [15]. Diversity, inequity, stereotyping, and other social determinants of health must be addressed to transform a comprehensive global public health response to an actively aging world population. The need to transform misaligned health systems with the older adults’ needs, clearly and convincingly requires redefinition and reconceptualization. Adding healthspan and continuous improvement of health care systems is crucial. Our proposed study attempts at redefining the health of older adults more broadly and diversely including physical function, anxiety, depression, fatigue, sleep disturbance and sleep-related impairments, the ability to participate in social roles and activities, pain interference, and pain intensity.
In our HEARTS study [20], we operationally defined health as that of the determinants stated in the PROMIS-29 questionnaire [33,34], which specifically pertains to physical function, anxiety, depression, fatigue, sleep disturbance, sleep-related impairment, ability to participate in social roles and activities, pain interference, and pain intensity. The experience of abuse refers to the different types of abuse older adults experience, physical, emotional, sexual, economic, and neglect [18,35]. Finally, resilience in our study is operationally defined as “personal qualities that enable one to thrive in the face of adversity” [36, p. 76]. Results showed that all the PROMIS health subscales are significantly correlated with each other [20,21]. Resilience is correlated with anxiety, depression, and pain intensity, such that higher resilience corresponds to lower anxiety, depression, and pain intensity [20,21]. Additionally, we find that suspicion of abuse has significant correlations with depression, pain intensity, and resilience [20,21]. Namely, higher depression and pain intensity correspond to higher older adults’ abuse suspicion, while higher resilience corresponds to lower older adults’ abuse suspicion [20,21]. Technology use or without technology use impacts the experience of abuse and social support [37]. We also have to be careful that technology could have a bias because they are created by humans, of humans, and for humans.
Detailed correlation results from regression models indicated that above and beyond demographic features, resilience had a significant prediction of anxiety [β = −0.46, p = .014] and depression [β = −0.54, p = .008]. Our findings on the significant negative relationship between older adults’ resilience and their depression and anxiety are consistent with other related studies exploring correlates of older adults’ resilience [11,38]. Additionally, our findings on the significant predictive effect of resilience on depression and anxiety imply the protective properties of resilience on depression and anxiety among older adults [38,39]. Hence, our findings concur with the conceptualization of resilience as that of a multidimensional construct comprising of individual characteristics such as attitudes and behaviors that facilitate adaptive coping despite adversities [40]. In a review of studies exploring the characteristics of the resilience of older adults, MacLeod et al. [41] reported that adaptive coping styles contribute to building resilience and thereby, reduce high levels of anxiety and depression.
Experience of Abuse
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
Elder abuse refers to acts whereby a trusted person (a family member, close friend, or caregiver) creates a risk of harm to an older adult [15]. The legal definition of older adult investment in and return on investment in adding health to years in older adult abuse varies by state and country but is defined as a person who is or may be mistreated and who, because of age, disability, or both, is unable to protect themselves [42]. The World Health Organization [15] reported that older adult abuse is now recognized internationally as a public health problem. As a result, older adults’ health as a pervasive societal concern requires the attention of health care systems, social welfare agencies, policymakers, researchers, educators, and the general public [42]. With a global increase in the older adult population, older adult abuse is expected to become an even more pressing problem, affecting millions of individuals worldwide. Older adult abuse is associated with devastating health consequences and societal costs. The global population of older persons will triple from 672 million in 2010 to 1.9 billion in 2050 [43]. It is becoming increasingly important to focus on policies and practices that support and enhance the wellbeing of older adults. For many, older adult abuse is cause for alarm, albeit their voices are drowned by poverty, disability, and cultural stereotypes. It is extremely difficult to quantify the extent of abuse, neglect, and exploitation because many cases go undetected and unreported [42].
A study of victimization among older adults and the effects of two resilience factors (i.e., sense of coherence [SOC] and social support) reported a negative association between victimization and health status [18]. In this study [18], victimization was associated with two resilience factors, SOC and social support. Additionally, SOC had a positive correlation with health status and social support moderated the association, i.e.., participants without social support had lower health scores [18]. Lack of social support and low SOC was found to be associated with high victimization with a suggestion that both resilience factors (SOC and social support) should become targets for future interventions [18].
In another study about the effects of abuse on health, Hui and Constantino [44] analyzed the data from the 2007 Behavioral Risk Factor Surveillance System (BRFSS) with a sample size of n=19,102 from the states of Hawaii, Virginia, and West Virginia. In this study, about 16.9% had experience with intimate partner violence (IPV). They also found that those who had experience with IPV by their sex partner had more mentally unhealthy days in a month compared with persons who have no experience of IPV [44]). Additionally, persons who had unwanted sex had at least 72 unhealthy days in a year, negatively impacting their healthspan [44]. These results appear somewhat consistent with the findings from the World Health Organization multi-country sample that found women who reported IPV at least once in their lifetime also reported significantly more emotional distress, suicidal thoughts, and suicidal attempts, compared to women who did not experience IPV [45].
The Resilience of Older Adults
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
Resilience is the human regenerative capacity that maintains health and function in the face of loss, disability, or disease [46] or bending without breaking, transforming failure to growth and challenges into opportunities, but it is fungible and expendable [47]. Hoare [25] suggested that the human attribute of resilience has a lengthy history, with positive adaptation as a marker [48]. The construct of resilience is found in theories of motivation and self-efficacy [49]. Recently, resilience is considered an attribute that supports health outcomes for those who had been exposed to trauma, environmental hazards, or poor caregiving [50]. Resilience throughout the life course enhances the ability to recover from adversity, thrive with a sustained purpose, and grow in a world of trauma, change, and chronic illness [46]. Resilience allows older adults to adapt to the wear and tear of aging while coping with problems and crises in ways that leave them feeling stronger and wiser than they would have been if they had not encountered those problems [46]. Furthermore, resilience is seen as both a process and an outcome [48] while others consider resilience a trait or inborn capability [48] or as a more fluid attribute that comes into play as one equilibrates after trials and tribulations of life [51].
Anderson et al. [52] conducted a mixed-method study to examine the resilience and growth in the aftermath of violent experience. The study elicited that spirituality, religious beliefs, and social support are crucial in the recovery process by giving them strengths and life purpose [52]. Survivors from her interviews display resilience by evaluating and adjusting mindsets, understanding life is not easy, and achieving greater life purposes by helping other survivors and sharing their own stories. In another study, the sense of coherence (SOC) as a factor of resilience had a positive correlation with health status and social support as well as moderate the association between lack of social support and lower health scores [18]. Lack of social support and low SOC was also found to be associated with high victimization with a suggestion that both SOC and social support as factors of resilience should become targets for future interventions [18].
The issue of whether the resilience phenomenon stands on its own or is the same as longsuffering, endurance, or positive emotionality [53,54] needs further study. Literature seems to suggest that resilience is fungible and can be “diminished,” “replenished,” or “regained” after adversity [55]. Despite its definition and conceptualization variance, resilience is possessed throughout the lifespan but varies in levels, therefore, assessable, and measurable [53,56-57]. Among resilience intervention studies, cognitive reframing can alter negative perceptions and mastery development can enhance a sense of achievement [25] in older adults. Furthermore, collaborations among researchers promise new resilience-enhancing interventions [6].
Proposed Research Design
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
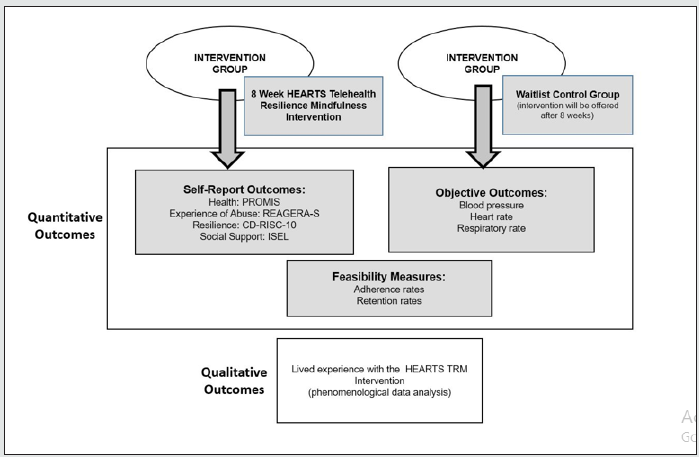
We will use a mixed-method sequential, transformative design to implement and test our proposed intervention, Telehealth Resilience Mindfulness (TRM) intervention. This design features an advocacy lens in which the quantitative and qualitative components of the study vary in order and priority [58]. The quantitative part will utilize a quasi-experimental method. This design will enable us to determine the efficacy of HEARTS telehealth resilience and mindfulness (TRM) Intervention based on objective and subjective outcomes. The objective outcomes will be measures through blood pressure readings, heart rate, and respiratory rate, while the subjective outcomes are measured through their health (PROMIS), the experience of abuse, resilience, and social support. The HEARTS telehealth resilience mindfulness intervention will be mainly delivered by text messaging. A baseline data will be gathered before the start and after the conclusion of the intervention. For comparison, there will be two treatment groups in this study: The Telehealth Resilience Mindfulness (TRM) and the Wait-List Group (WLG). The phenomenological qualitative design of the study will focus on the lived experiences of participants on HEARTS Telehealth Resilience Mindfulness Intervention.
Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
We anticipate that the TRM intervention could result in an observable effect on emotional and physical engagement, attention to the cognitive organization [5,6]. Furthermore, Emezue and Bloom [5] suggest that the more communication technologies (computers or smartphones) are used, the more likely the older adult will reject abusive and disrespectful treatment. Policymakers and program planners should consider the potential implications of information technology access relating to survivors of abuse. Constantino et al. [10] found that survivors felt that disclosing their experience was easier and safer through a computer than face-to-face with a clinician or any “interested” person, and that advice from a computer or phone was acceptable and accessible. However, participants may feel skeptical of a computer’s ability to give empathy, emotional support, or meaningful feedback [20]. For this reason, in this prospective project, we will explore the feasibility of TRM delivered by text messaging to enhance resilience and mindfulness to survivors. Emezue and Bloom [5] report that evidence shows most survivors of abuse prefer the practicality and confidentiality of technology-enabled interventions and guided online support as opposed to in-person individual or group meetings, making this telehealth an opportunity in enhancing resilience and mindfulness. Hoare [25] focused on cognitive reframing and reappraisal, showing that reports of reappraisal and reframing tend to be more flexible and have better social outcomes. The figure shows our proposed mixed-method study.
Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
The HEARTS Telehealth Resilience Mindfulness (TRM) Intervention is comprised of eight weekly sessions, primarily delivered by text messaging. The focus is on the improvement of resilience through the development of mindfulness skills. Below further describe the details of each weekly session.
Week 1
Daily application of one or more of the following mindfulness exercises: Sit comfortably erect on a chair and feet flat on the floor. Open your eyes and drop your gaze to the floor beneath your feet and breathe. Remove as many distractions as you can but keep focus first on the internal sensations from your body. Notice your limbs, neck, shoulders, and breathe, then your abdomen, diaphragm, and chest. Notice your thoughts and feelings. Imagine you are in front of your door, waiting for your visitors to arrive. They came, and you greeted them with love, kindness, and compassion. Then focus on the external sensations that are delivered to your 5 senses. -sight, smell or its absence, taste, or its absence, hearing or its absence, and touch-cooler or warm temperature. Then integrate these 2 (internal and external) sensations you have. Thirty 30 minutes. Weekly journaling of lessons learned and the flow of thoughts and feelings. Weekly phone or TM (Text Messages) check-in.
Week 2
Exercises-Movement for Week 2 includes the following: (1) Bend your thumb across the palm as far as you can. Do this 20 times. (2) Place palm flat on the table. Spread them apart and bring them close together. Do this 20 times. (3) Pick up a pencil or a pen. Roll it between the thumb and each finger. Do this 20 times [59]. (4) Setup: Begin sitting in an upright position. Movement: gently squeeze your shoulder blades together, relax, and then repeat 20 times. (5) Setup: Begin in a standing upright position in the center of a doorway. Movement: With your elbow bent, place your hand on the side of the doorway. Take a small step forward and slightly rotate your body until you feel a stretch in the front of your shoulder. Hold this position for 3 seconds and repeat it 10 times. Imagine your agility, flexibility, and concentration [60]. Total of 25-30 minutes. Weekly journaling of lessons learned and the flow of thoughts and feelings. Weekly phone or TM check-in.
Week 3
Daily application of one or more of the following mindfulness exercises: Setup in an upright position with your feet flat on the floor. Movement: Gently draw your chin in, while keeping your eyes fixed on something in front of you. Do not look down or bend your neck forward, being mindful of feelings, and thoughts without judging (10 minutes). Observe yourself (15 minutes) by focusing on the upper portion of your body, your chest, heart, and lungs, and diaphragm-observe their function [60]. Total of 25 minutes. Weekly journaling of lessons learned from these exercises. Weekly phone or TM check-in.
Week 4
Unscramble these words and put them in a correct sentence on a clean sheet of writing paper: (1) “almond my cream favorite chocolate is ice”; (2) “crackers bed should never one eat”; (3) “the swipe machine card your through”; (4) “picked of peppers Piper peck Peter a pickled”; (5) “Senate vetoed tax the the both the and House bill”; and (6) “the 200th States marked birthday 1976 of the United” [61]. No judgment but focus, concentrate and relax. Weekly journaling of lessons learned from these exercises. Weekly phone or TM check-in.
Week 5
Daily application of the following mindfulness exercises: Being mindful of your feelings. Close your eyes and imagine you are a leaf on a stream who aims never to be swept to the banks-always focus and concentrate to float in the middle of the stream no matter where the wind or the waves from the rocks toss you until you get to the river and then to the sea and travel to the ocean. The wind and waves could be the trials and tribulations that you meet in your journey to life’s stream, river, sea, and ocean; you can mention them but do not focus on them-they are only distractions. Focus on your journey and the positive emotions, sensations, memories, and resilience. 20 minutes. Weekly journaling of lessons learned from this exercise-- awareness of one’s values, greater resilience, reduce autopilot, and less reactive. Weekly journaling of lessons learned from these exercises. Weekly phone or TM check-in.
Week 6
Answer each question with a one-word response on a writing paper. The number of letters provided is a clue to the answer: (1) A sound of laughter- 2 letters; (2) To harm or cause pain-4 letters; (3) Equals 60 seconds- 6 letters; (4) Equals 60 minute- 4 letters; (5) What you walk on- 5 letters; (6) Between sunset and sunrise- 5 letters; ( 7) What many people live in -5 letters; (8) opposite of man-5 letters; (9) not this one, but-one- 4 letters; and (10) an eating utensil- 4 letters [61]. Weekly journaling of lessons learned from these exercises, following directions, focus, and concentration. Weekly phone or TM check-in.
Week 7
The following are the activities for Week 7: (1) Listen to the news show for 5-10 minutes and write down your summary of the most important information. (2) Read a paragraph in a magazine or newspaper or online and write down a summary of what you read. (3) Provide directions to your friend from your airport to your place house. Weekly journaling of lessons learned from these exercises, following directions, focus, and concentration. Weekly phone or TM check-in.
Week 8
Daily application of one or more of the following mindfulness exercises: Write down specific directions you would like to five to a friend, from your local church or airport to your house—improved focus, give/following directions, ability to face challenges, and cognitive regulation. Weekly journaling of lessons learned from a video: Cognitive regulation. Weekly phone or TM check-in.
The mindfulness exercises and lessons described above were adapted from Erin Commendatore, a mindfulness webinar interventionist at the University of Pittsburgh Mindfulness Series, from March to April 2021. The resiliency sessions were adapted from works on the resilience of Feder et al. [6], Hoare [25], and Reyes et al. [62].
The answers to the Week 4 exercises (unscramble the words to form into a sentence) are the following: 1) My favorite ice cream is chocolate almond. 2) One should never eat crackers in bed. 3) Please swipe your machine card through. 4) Peter Piper picked a peck of pickled peppers. 5) The Senate vetoed both the tax and the House bill. 6) 1976 marked the 200th birthday of the United States. Here are answers to Week 6- One-word response to 10 questions: 1) HA, 2) HURT, 3) MINUTE, 4) HOUR, 5) FLOOR, 6) NIGHT, 7) HOUSE, 8) WOMAN, 9) THAT, and 10) FORK.
Instruments for Evaluation
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
A brochure will be distributed to communities where potential participants gather. Below are the descriptions of each of the instruments for evaluation that will be used:
Sociodemographic Data Questionnaire (SDQ)
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
The SDQ will be used at baseline only to document age, race, education, employment, religion, and income. The SDQ can be completed in 3-5 minutes.
Health
We will use the PROMIS (Patient-Reported Outcomes Measurement Information System) version 1.0 short form [33,34] to assess anxiety to determine health status including, four items on physical function, anxiety, anger, depression, fatigue, sleep disturbance, ability to participate in social roles and activities, pain interference, and pain intensity [33,34]. Testing among over 20,000 individuals from the U.S. general population has resulted in individual item calibrations that enable one to generate a T-score (mean = 50; standard deviation = 10). The health subscale can be completed in 4-5 minutes.
Elder Abuse and Lifetime Experiences
We will use the Responding to Elder Abuse in Geriatric care - Self-administered (REAGERA-S) [35] will assess elder abuse (e.g., has anyone threatened to harm you? and have you experienced physical abuse before or after you were 18 years old?). Space will be provided to check the type of abuse the participant has experienced: emotional, physical, sexual, or economic. The sensitivity of the instrument, for lifetime abuse, is 71.9% (95% CI 53.3-86.3) and specificity 92.3% (95% CI 79.1-98.4). For current abuse, the sensitivity is 87.5% (95% CI 61.7-98.5) and specificity is 92.3% (95% CI 79.1-98.4). REAGERA-S can be completed in 3-5 minutes.
Resilience
The Connor-Davidson Resilience Scale 10-item, CD-RISC-10 [63] will be used to measure psychological resilience. The CD-RISC-10 comprises 10 items, and each item on the scale is rated on a 5-point Likert scale from 0 (not true) to 4 (true nearly all the time). The total score ranges from 0 to 40, with higher total scores indicating greater resilience. The scale demonstrated good construct validity and internal consistency (α = .85) during the development of the scale [63]. The CD-RISC-10 also had a good Cronbach’s alpha level of .85 [63]. The CD-RISC-10 can be completed in 5¬-7 minutes.
Social Support
The Interpersonal Support Evaluation List (ISEL) is the instrument we will use to measure social support. ISEL was originally developed for a standard adult population [64,65]. The scale measures interpersonal support in four dimensions: information support, spending free time together, instrumental support, and appreciation - self-esteem. The type of coping strategy depends primarily on informational support received, and finally, how a person responds to stress is highly associated with received social support [66]. Reliability and validity studies of the ISEL using adult samples reported internal reliability (alpha coefficient) for the ISEL ranging from 0.88 to 0.90, and between 0.70 and 0.82 for appraisal, 0.62 and 0.73 for self-esteem, 0.73 and 0.78 for belonging, and 0.73 and 0.81 for tangible support [65,67-69]. The ISEL can be completed in 57 minutes.
Feasibility and Acceptability of the Intervention. An interview guide will be used to explore the feasibility and acceptability of the intervention and the quality of its administration and accessibility of the HEARTS Telehealth Resilience and Mindfulness Intervention among participants. The interview can be completed in 25-35 minutes.
Conclusions
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
Systemic factors in healthcare and justice services increase or decrease healthspan (a portion of life spent in good health) throughout the life course. Lifecourse Health Development [27,28] is a theory that integrates biological, socioeconomic, justice, and environmental infrastructure. This conceptualized TRM practice change can be delivered in-person by text messaging or by video conferencing (i.e., Zoom). The rationale is to span the digital, biological, socioeconomic, justice, and environmental infrastructure divide between the service providers Strategies that will be used to implement the practice change (TRM) are community-based participatory research and practice, that emphasize collaborating, consulting, and where ethics, role and role responsibility and accountability, communication, and teamwork competencies in community participants’ engagement are paramount [70].
We are aware that sometimes during our life course we have been marginalized. Marginalization is a process through which certain individuals experience multiple social determinants concurrently placing them in sections and margins, by rejecting one’s culture, race, age, gender, or sexual orientation by the dominant host population [1]. Legarde [71] identifies an approach to empowerment and equality as judging people by their capability to do the things they value. This approach to empowerment facilitates the ability to participate in one’s community and contribute to sustainability in health outcomes. Failed attempts at integration lead to marginalization expressed in three main outcomes: the creation of margins, living between cultures, and the creation of vulnerabilities. The creation of margins is a process of creating boundaries, sections (intersectionality), and peripheralized by approximation (not proximation) of the individual, group, or population. Age and poverty create margins, sections, and vulnerabilities [71].
The second outcome of marginalization is living between cultures leading to incomplete integration where the individual relinquishes characteristics of the parent culture to connect with the dominant society and fails in both [1]. In the process of living between cultures, the person lives on the periphery on the verge of exclusion, and the intersection of multiple ways of distancing. The third and last outcome of marginalization is the creation of vulnerabilities. Vulnerabilities are a state of being exposed to, and unprepared to fight or flee from health, people, and environment’s damaging circumstances that pose a physical, psychological, biological, social, and economic threat to the individual, group, or population. Age disparities are an example of the creation of vulnerabilities. Globally, older adults make up 60% of the living on less than a dollar a day, locked out of leadership positions, underutilized, underpaid, under-appreciated, stressed, abused, and traumatized [18]. The cumulative outcome of these three themes of marginalization is toxic stress that leads to maladaptive coping behaviors, poor self-esteem, lack of self-efficacy, cognitive dissonance, and increased incidence of substance abuse, posttraumatic stress, and suicide [3].
The strength of the evidence guiding the change (HEARTS Telehealth Resilience Mindfulness [TRM] Intervention) in practice comes from the Range of Possible Changes (RPC) Model that guides the theory of change in intervention. We are aware that technology may have some bias, prejudice, and stereotypes because they are made by, for, and of humans. The stakeholders that will influence and participate in the change in practice are observable in institutions’ ethics, role, communication, and teamwork help and not hinder, catapult and not shackle and cutting away obstacles and barriers to true human flourishing. The evaluation strategies will assess the impact of change that are embodied in HEARTS (health, experiences of abuse and trauma, resilience, technology use, and social support) in a mixed-methods strategy where qualitative data are quantified and quantified data are qualified, in the development of a telehealth resilience mindfulness intervention.
Conflict of Interest Statement
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
No conflict of interest has been declared by the authors.
References
- Introduction
- Significance
- Conceptual Framework
- Literature Review
- The Health of Older Adults
- Experience of Abuse
- The Resilience of Older Adults
- Proposed Research Design
- Hearts Telehealth Resilience Mindfulness (HEARTS TRM) Intervention
- Description of the HEARTS Telehealth Resilience Mindfulness (TRM) Intervention
- Instruments for Evaluation
- Sociodemographic Data Questionnaire (SDQ)
- Conclusions
- Conflict of Interest Statement
- References
- Baah FO, Teitelman AM, Rieegel B (2019) Marginalization: Conceptualizing patient vulnerabilities in the framework of social determinants of health-An integrative review. Nursing Inquiry 26(1).
- Kaeberlein M (2018) How healthy is the healthspan concept? GeroScience 40(4): 361-364.
- Trent M, Dooley D, Douge J (2019) The impact of racism on child and adolescent health. American Academy of Pediatrics 114(2).
- Carmack S, Kennedy S, Clow L, Joshi A, Tupy S (2018) Promoting whole health at school: How mindfulness movement and compassion practices transformed three underserved communities. American Public Health Association San Diego CA.
- Emezue C, Bloom TL (2021) PROTOCOL: Technology-based and digital interventions for intimate partner violence: A meta-analysis and systematic review. Campbell Systematic Reviews 17(1): e1132.
- Feder A, Fred-Torres S, Southwick SM, Charney DS (2019) The biology of human resilience: Opportunities for enhancing resilience across the life span. Biological Psychiatry 86(6): 443-453.
- Linde DS, Bakiewicz A, Normann AK, Hansen NB, Lundh A (2020) Intimate partner violence and electronic health interventions: Systematic review and meta-analysis of randomized trials. Journal of medical Internet research 22(12): e22361.
- Constantino RE, Hamdan-Mansour AM, Henderson A, Noll-Nelson B, Doswell W, et.al. (2014a) Assessing the readability and usability of online H-E-L-P intervention for PV survivors. Open Journal of Nursing 4(3): 150-157.
- Constantino R, Wu L, de la Cruz D, Burroughs J, Hwang JH, et.al. (2014b) Exploring the feasibility of text messaging intervention in intimate partner violence. Open Journal of Nursing 4(3): 528-537.
- Constantino RE, Braxter B, Ren D, Burroughs JD, Doswell W, et.al. (2015) Comparing online with face-to-face HELP intervention in women experiencing intimate partner violence. Issues in Mental Health Nursing 36(6): 430-438.
- Fossion P, Leys C, Kempenaers C, Braun S, Verbanck P, et.al. (2013) Depression, anxiety, and loss of resilience after multiple traumas: An illustration of a mediated moderation model of sensitization in a group of children who survived the Nazi Holocaust. Journal of Affective Disorders 151(3): 973-979.
- Moffitt TE, The Klaus-Grawe 2012 Think Tank (2013) Childhood exposure to violence and lifelong health: Clinical intervention science and stress biology research join forces. Development and Psychopathology 25(4pt2): 1619-1634.
- Hodes RJ (2020) The National Institute on Aging: Strategic directios for research, 2020-2025.
- De Los Reyes A, Kazdin AE (2006) Conceptualizing changes in behavior in intervention research: the range of possible changes model. Psychological Review 113(3): 554-583.
- World Health Organization (2015) World report on ageing and health.
- Centers for Disease Control and Prevention (2020) Planning for an emergency: Strategies for identifying and engaging at-risk groups. A guidance document for emergency managers.
- Clayton JA (2020, October 8). Social determinants of health: Like water to a fish. National Institute of Health Office of Research on Women’s Health.
- Simmons J, Swahnberg K (2021) Lifetime prevalence of polyvictimization among older adults in Sweden, associations with ill-heath, and the mediating effect of sense of coherence. BMC Geriatrics 21 Article 129.
- Bates RA, Blair LM, Schlegel EC, McGovern CM, Nist MD, et.al. (2018) Nursing across the lifespan: Implications of life course theory for nursing research. Journal of Pediatrics Health Care 32(1): 92-97.
- Constantino RE, Reyes AT, Kregg-Byers CM, Braxter B, Scott PW, et.al. (2020) Matters of HEARTS: Health, the experience of abuse, resilience, technology use, and safety of older adults. Educational Gerontology, 46(7): 367-381.
- Cuevas PEG, Urgel EL, Dela Cruz DC, Mizona KJB, Constantino RE (2020) Elder Abuse Correlation to Health and Resilience in Older Adults. Elder Abuse & Neglect Educational Gerontology 46(6): 331-338.
- Jones CP, Truman BI, Elam-Evans LD, Jones CA, Jones CY, et.al. (2008) Using "socially assigned race" to probe white advantages in health status. Ethnicity & disease 18(4): 496-504.
- Constantino R, Kim Y, Crane PA (2005) Effects of a social support intervention on health outcomes in residents of a domestic violence shelter: A pilot study. Issues in Mental Health Nursing 26(6): 575-590.
- Cuevas PEG, Urgel EL, Dela Cruz DC, Mizona KJB, Constantino RE (2020) Elder Abuse Correlation to Health and Resilience in Older Adults. Elder Abuse & Neglect Educational Gerontology 46(6): 331-338.
- Hoare C (2015) Resilience in the elderly. Journal of Aging and Life Care 1(3): 3-14.
- O’Connor M, Bowles KH (2021) Telehealth and mHealth. Research in Nursing and Health 44(1): 3-4.
- Halfon N, Hochstein M (2002) Life course health development: an integrated framework for developing health, policy, and research. The Milbank Quarterly 80(3): 433-479.
- Halfon N, Larson K, Lu M, Tullis E, Russ S (2014) Lifecourse health development: Past, present and future. Maternal and Child Health Journal 18(2): 344-365.
- Elder GH Jr (1998) The life course as developmental theory. Child Development 69(1): 1-12.
- Singer C (2018) Health effects of social isolation and loneliness. Journal of Aging Life Care 1: 1-7.
- Chatterji S, Byles J, Cutler D, Seeman T, Verdes E (2015) Health, functioning, and disability in older adults–present status and future implications. Lancet 385(9967): 563-575.
- Crimmins EM, Beltrán-Sánchez H (2011) Mortality and morbidity trends: Is there compression of morbidity? The Journals of Gerontology: Series B Psychological Sciences and Social Science 66B(1): 75-86.
- Craig BM, Reeve BB, Brown PM, Cella D, Hays RD, et.al. (2014) US valuation of health outcomes measured using the PROMIS-29. Value in Health 17(8): 846-853.
- Hays RD, Spritzer KL, Schalet BD, Cella D (2018) PROMIS-29 v2.0 profile physical and mental health summary scores. Quality of Life Research 27(7): 1885-1891.
- Simmons J, Wiklund N, Ludvigsson M, Nägga K, Swahnberg K (2020) Validation of REAGERA-S: a new self-administered instrument to identify elder abuse and lifetime experiences of abuse in hospitalized older adults. Journal of Elder Abuse & Neglect 32(2): 173-195.
- Connor K, Davidson J (2003) Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depression and Anxiety 18(2): 76-82.
- Palompon D, Reyes AT, Garcia L, Cutamora J, Gonzaga J, et.al. (in review). HEARTS matter: The moderation and mediation effects of resilience, experience of abuse and technology use, and safety in older persons. Ageing International.
- Laird KT, Krause B, Funes C, Lavretsky H (2019) Psychobiological factors of resilience and depression in late life. Translational Psychiatry 9(1): 88.
- Wermelinger Ávila MP, Lucchetti AL, Lucchetti G (2017) Association between depression and resilience in older adults: a systematic review and meta-analysis. International Journal of Geriatric Psychiatry 32(3): 237-246.
- Burns RA, Anstey KJ (2010) The Connor-Davidson Resilience Scale (CD-RISC): Testing the invariance of a uni-dimensional resilience measure that is independent of positive and negative affect. Personality and Individual differences 48(5): 527-531.
- MacLeod S, Musich S, Hawkins K, Alsgaard K, Wicker ER (2016). The impact of resilience among older adults. Geriatric Nursing 37(4): 266-272.
- Feltner C, Wallace I, Berkman N, Kistler CE, Middleton JC (2018) Screening for intimate partner violence, elder abuse, and abuse of vulnerable adults Evidence report and systematic review for the US Preventive Services Task Force. JAMA 320(16): 1688-1701.
- United Nations, Department of Economic and Social Affairs, Population Division (2015). World population ageing 2015. New York, NY: United Nations.
- Hui V, Constantino RE (2021) The association between life satisfaction, emotional support, and perceived health among women who experienced intimate partner violence (IPV) – 2007 behavioral risk factor surveillance system. BMC Public Health 21, Article 641.
- Ellsberg M, Jansen HA, Heise L, Watts, CH Garcia-Moreno C & WHO Multi-country Study on Women's Health and Domestic Violence against Women Study Team (2008). Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: an observational study. Lancet 371(9619): 1165-1172.
- Edwards ES, Hall J, Zautra A (2015) Resilience in aging. Eldercare: A resource for interprofessional providers. Tucson, AZ: Arizona Center on Aging University of Arizona.
- Constantino RE, Zalon ML (2020) From disruptive to frugal innovation. In AJ Murrell, JL Petrie-Wyman, A Soudi (Eds.), Diversity across the disciplines. Charlotte, NC: Information Age Publishing Inc.
- Hu T, Zhang D, Wang J (2015). A meta-analysis of the trait resilience and mental health. Personality and Individual Differences 76: 18-27.
- Masten AS, Reed MJ (2002) Resilience in development. In CR Snyder, Lopez SJ (Eds.), Handbook of positive psychology. New York, NY: Oxford University Press.
- Luthar SS, Cicchetti D, Becker B (2000). The construct of resilience: a critical evaluation and guidelines for future work. Child Development 71(3): 543-562.
- Gucciardi DF, Jackson B, Hodge K, Anthony DR, Brooke LE (2015) Implicit theories of mental toughness: Relations with cognitive, motivational, and behavioral correlates. Sport Exercise and Performance Psychology 4(2): 100-112.
- Anderson KM, Renner LM, Danis FS (2012) Recovery: Resilience and growth in the aftermath of domestic violence. Violence Against Women 18(11): 1279-1299.
- Bonanno GA (2004) Loss trauma and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist 59(1): 20-28.
- Robinson JS, Larson CL, Cahill SP (2014) Relations between resilience, positive and negative emotionality, and symptoms of anxiety and depression. Psychological Trauma: Theory, Research, Practice, and Policy, 6(Suppl 1): S92-S98.
- Masten AS (2011) Resilience in children threatened by extreme adversity: frameworks for research, practice, and translational synergy. Development and Psychopathology 23(2): 493-506.
- Masten AS (2001) Ordinary magic: Resilience processes in development. American Psychologist 56(3): 227-238.
- Reyes AT, Serafica R, Cross CL, Constantino RE, Arenas RA (2018) Resilience, acculturative stress, and family norms against disclosure of mental health problems among foreign-born Filipino American women. Asian/Pacific Island Nursing Journal 3(3): 80-93.
- Creswell JW, Klassen AC, Clark VLP, Smith KC (2011) Best practices for mixed methods research in the health sciences.
- Shirley Ryan Ability Lab (2017) Upper body: Fine motor exercise program – Finger exercises & activities.
- Medbridge (2021) Home exercise program.
- Brubaker SH (2009) Workbook for language skills. Self-published.
- Reyes AT, Bhatta TR, Muthukumar V, Gangozo WJ (2020) Testing the acceptability and initial efficacy of a smartphone-app mindfulness intervention for college student veterans with PTSD. Archives of Psychiatric Nursing 34(2): 58-66.
- Campbell-Sills L, Stein MB (2007) Psychometric analysis and refinement of the Connor-Davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress 20(6): 1019-1028.
- Cohen S, Hoberman HM (1983) Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology 13(2): 99-125.
- Cohen S, Syme SL (1985) Issues in the study and application of social support. New York: Academic.
- Dunkel-Schetter C, Folkman S, Lazarus RS (1987) Correlates of social support receipt. Journal of personality and social psychology 53(1): 71-80.
- Bovier PA, Chamot E, Perneger TV (2004) Perceived stress, internal resources, and social support as determinants of mental health among young adults. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment Care and Rehabilitation 13(1): 161-170.
- Gjesfjeld CD, Greeno CG, Kim KH, AndersonCM (2010) Economic stress, social support, and maternal depression: Is social support deterioration occurring? Social Work Research 34(3): 135-143.
- Lin J, Thompson MP, Kaslow NJ (2009) The mediating role of social support in the community environment-psychological distress link among low-income African American women. Journal of Community Psychology 37(4): 459-470.
- Interprofessional Education Collaborative. (2016). Core competencies for interprofessional collaborative practice: 2016 update. Washington, DC: Interprofessional Education Collaborative.
- Legarde C (2014). Empowerment – The Amartya Sen lecture 2014.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...