Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Research Article(ISSN: 2690-5760) 
Seroprevalence of Treponema pallidum, HIV- Co-Infection, Cognitive Effects and Risk–Variables for Infection in a Tertiary Psychiatric Hospital in Nawfia, Nigeria Volume 2 - Issue 3
Andrew K Amegovu1*, Timothy Chewere3, SusanJokudu2 and Michael Mawadri3
- 1Department of Food Science and Technology, University of Juba , South Sudan
- 2Andre Foods South Sudan (AFSS), South Sudan
- 3Andre Foods International (AFI), Uganda
Received: July 17, 2020 Published: August 27, 2020
Corresponding author: Andrew Kiri Amegovu, University of Juba, Juba, South Sudan
DOI: 10.32474/JCCM.2020.02.000138
Abstract
Background: Despite assessment of nutritional status by Mid-Upper Arm Circumference (MUAC) being easier, requiring less expertise than with Body Mass Index (BMI), there are no internationally recommended cutoffs for the assessment of overweight and obesity in adults. To-date the BMI is the most widely used anthropometric measure as the World Health Organization (WHO) gold standards to diagnose overweight and Obesity (WHO 1995). However, BMI requires some technical skills and therefore limiting its usage. This study explored the use of MUAC as an alternative diagnostic tool for overweight and obesity in adults.
Methods: Anthropometric data obtained from 251 adults was used for the study. Correlation between MUAC and BMI was determined using the Pearson correlation and simple linear regression. The diagnostic accuracy of MUAC was determined using Receiver Operating Characteristics (ROC) curve analysis for WHO standards BMI reference for underweight, overweight and obesity. Youden’s index was used to determine optimal MUAC cut offs from the ROC curve coordinates.
Results: A strong positive correlation between BMI and MUAC is observed [r (249) = 0.8621, p < .0001]. Results showed outstanding diagnostic characteristics of MUAC generated by ROC curves compared with standard BMI reference with diagnostic accuracy of 100% (obesity) and 90% (overweight).
Conclusions: This study suggests MUAC>31.1cm for obesity; MUAC29.9cm to ≤ 31.1cm for overweight; MUAC 25.4cm to<29.9cm for normal weight and MUAC < 25.4cm underweight. MUAC can therefore be used as an alternative to BMI in the diagnosis of obesity and in early detection of overweight in adults.
Keywords: Nutrition assessment in adults; Mid-upper Arm Circumference; Body mass index; Overweight and Obesity
Abbreviations:
BMI: Body Mass Index; MUAC: Mid-upper-arm-circumference; NGOs: Nongovernmental organisations; ROC curve: Receiver operating characteristic curve; WHO: the World Health Organisation
Background
According to the World Health Organization, an estimated 2.8 million dying each year from overweight or being obese (WHO, 2020) while more than 1.9billions from18years and older were overweight in 2016. Of these over 650 million adults were obese. Additionally, 39% of adults aged 18 years and over (39% of men and 40% of women) were overweight in 2016. Overall, about 13% of the world’s adult population (11% of men and 15% of women) was obese in 2016. The worldwide prevalence of obesity nearly tripled between 1975 and 2016. In 2019, an estimated 38.2 million children under the age of 5 years were overweight or obese. Once considered a high-income country problem, overweight and obesity are now on the rise in low- and middle-income countries, particularly in urban settings [1]. Systematic reviews of the international literature suggest that people with obesity spend 30% more on medical care [2]. Estimates of the cost of obesity to health systems vary between nations but may account for between 0.7% and 2.8% of a country’s total health care costs [3]. Anthropometric measurements are a series of quantitative measurements of the muscle, bone, and adipose tissue used to assess the composition of the body. The core elements of anthropometry are height, weight, body mass index (BMI), body circumferences (waist, hip, and limbs), and skin fold thickness.
These measurements are important because they represent
diagnostic criteria for obesity, which significantly increases the
risk for conditions such as cardiovascular disease, hypertension,
diabetes mellitus, and many more which lead to increased risk
of morbidity and mortality and affect the country’s economy
by increasing the burden on state-funded and out-of-pocket
expenditure and also by affecting productive life years [4,5].
Although these anthropometric assessments are considered to
be less reliable for assessing malnutrition than sophisticated
but expensive body composition assessment techniques such as
hydro densitometry, electronic bio impedance, dual-energy X-ray
absorptiometry among others, simplicity of usage and low cost
of implementation make these assessments the ideal choice for
population-based evaluations [6,7].
BMI, a marker for generalized adiposity and measured as
body weight (in kg) divided by height (in meter2) squared, is the
most widely used anthropometric measure as it is inexpensive
and non-invasive and can be collected by evaluators with minimal
training [7,8]. Therefore, assessment of BMI became popular not
only as individual-level clinical and nutritional assessments but
also as a survey tool, especially for assessment of undernutrition
in developing nations [9]. Nevertheless, in large-scale populationbased
surveys and for regular monitoring, assessment of nutrition
status, BMI becomes impractical and tedious because of logistical
reasons as the equipment for assessment of weight and height
often proves clunky in the field. Moreover, it is difficult to measure
weight and height for non-ambulatory participants/patients. As
a result MUAC has long been used as a tool for anthropometric
measurement as it is easier to implement than BMI, with minimum
requirement of equipment and acceptable sensitivity and
specificity for detecting underweight [10]. During recent times,
MUAC has been used for evaluation of adult nutritional status as
well, especially in resource-limited settings [11] and populationbased
surveys, where accurate measurements of height and weight
require reasonably large logistical mobilization. MUAC is a simpler
measure than BMI, requiring minimum equipment and has been
demonstrated to predict morbidity and mortality in 6–59 months
old Senegalese children [12]. Such measurements have recently
been used in the diagnosis of adult malnutrition in hospitals [13]
and it is found that low MUAC better predicts mortality than low
BMI in Dutch older adults [14]. Several studies have reported a close
[15-18]. ts simplicity and ease of use makes it a candidate for use
in adult nutritional assessment. All these studies found strong and
significant associations between MUAC and BMI.18In all studies,
only one study included both men and women while the rest of
the studies included either only men or only women [19]. Many of
these studies have established their own MUAC cutoffs to match the
<18.5Kg/m2 criteria for diagnosing undernutrition. Their results
ranged between 22.5cm and 25.5cm as suitable cut off point for
BMI 18.5Kg/m2. Some of the cut offs have overlapped [20].
This study therefore explored the possibility of using MUAC
to screen for overweight and obesity among adults, and thus to
suggest suitable cut-off value for overweight and obesity in addition
to color coding for ease of use for those with low level of literacy.
Methods
Study setting
This study was conducted at University of Juba, South Sudan. The University was established as comprehensive premier learning hub in 1975 and currently has a population of 20,000 students and staff spread across 15 Schools, 3 Colleges, 3 Institutes, and 4 specialized centers.
Study design and participants
We conducted a cross-sectional study design that employed systematic simple random sampling technique. Using Kish and Leslie’s formula for sample size determination for cross-sectional studies (N= Zα 2 P (1- P) δ 2), a total of 272 adult students aged 18yearsand above including teaching staff were sampled. Study participants were selected from the constructed frame based on the existing University students’ and teaching staff’s lists using simple random sampling technique without replacement. Pregnant and/ or lactating mothers and disabled persons were excluded.
Anthropometric data collection
The anthropometric variables obtained from study participants included sex, age in years, weight (in Kg to nearest 0.1Kg), height (in cm to the nearest 1 cm) and MUAC (in cm to the nearest 0.1cm) using standard procedures. Measurement of the MUAC was conducted using a non-stretched measuring tape with the right or left arm hanging in a relaxed position and the tape was positioned midway between the tip of the acromion and olecranon. The tape was placed gently but firmly around the arm to avoid compression of soft tissue. Weight measurements were taken while barefoot and in standing position using digital scales. To ensure accuracy, the weighing scales were calibrated periodically. Weight measurements were taken twice and the average recorded. Height was measured to the nearest centimeter using a standard tape. To achieve this, the non-stretchable tape was vertically fixed on a wall perpendicular to the ground. The tape was glued using transparent adhesives and was taken to ensure that there was no fold or tilting to either side. During the measurement, the tape was repeatedly checked for loosening or tilting. Height was taken twice and the average recorded to the nearest 1cm. BMIs were calculated from the recorded height and weight variables. It was computed as a fraction of weight in Kilograms and square of the corresponding individual’s height in square meters (Kg/m2). Following WHO cut offs, the results were converted into a categorical variable and grouped as underweight if BMI <18.5; normal weight for BMI 18.5 to <25; overweight for BMI 25 to <30 and obese if BMI equaled or exceeded 30.
Statistical analysis
The relationship between MUAC and BMI was linearly determined using the Pearson correlation and simple linear regression. The diagnostic accuracy (sensitivity and specificity) of the MUAC was determined using Receiver Operating Characteristics (ROC) curve analysis. For the ROC curve analysis, validity of MUAC was evaluated against BMI as the reference. To achieve this, ROC curves of MUAC values were plotted at different BMI cut off points. For each graph, the Area Under the Curve (AUC) was used to determine the accuracy of MUAC to classify nutritional status at the specified BMI cut off point. Diagnostic accuracy denoted by area under a ROC curve ranges from 0–1. Following Schoonjans et al (1995), the closer the shift to the upper left corner of the ROC plot, the closer the area is to 1 and therefore the better the measure. Youden’s indices were then generated and used to define the optimal MUAC cut-off point for selected BMI limits. At each BMI cut off, the MUAC value with highest Youden’s index was chosen as the corresponding cut-off as defined in Youden, W. J. (1969).
Results
Anthropometric characteristics of the participants
Table 1 shows anthropometric parameters collected from 251 participants; 85% male (n=214) and 15% female (n=37). The mean age, weight, height, MUAC and BMI of the population were 26.8±4.7years, 64.4±9.8Kg, 1.8±0.1m, 26.2±2.7cm and 20±3.1Kg/ m2 respectively.
Relationship between BMI and MUAC using linear regression and Pearson correlation
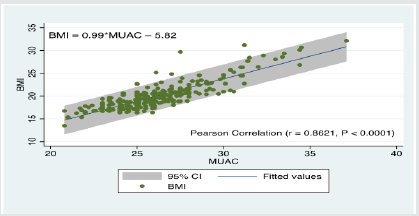
A simple linear regression model with BMI as the dependent variable and MUAC as a single independent variable showed a strong linear relationship between BMI and MUAC. MUAC can predict BMI at statistical significance F (1, 219) = 720.7, p= 0.0000 and MUAC accounted for 74% of the explained variation in BMI. The regression equation is expressed as: BMI = 0.99*MUAC – 5.82 + ε. In addition, a Pearson’s product-moment correlation was run to assess the relationship between BMI and MUAC. Results showed a strong positive correlation between BMI and MUAC r (249) = 0.8621, p < .0001). The relationship between BMI and MUAC with 95% prediction limits is represented in Figure 1.
Diagnostic accuracy using Receiver Operating Characteristics (ROC) curve analysis
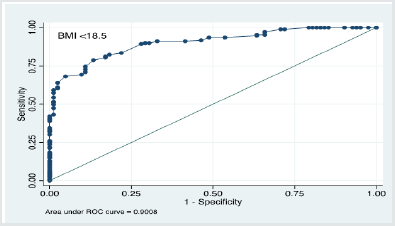
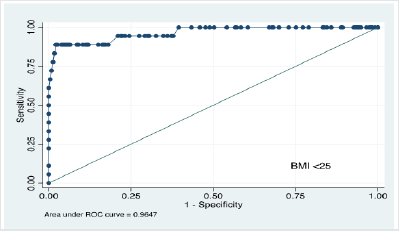
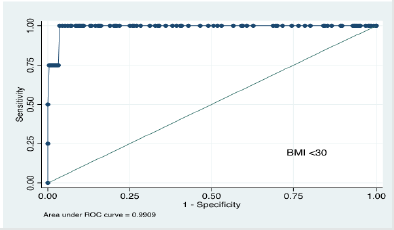
The study conducted ROC curve analysis of MUAC values and generated area under the curve for three different BMI cut offs i.e. <18.5Kg/m2, <25Kg/m2 and <30 Kg/m2 corresponding to underweight, normal weight and overweight respectively. Results revealed that the area under the curve were 90% (86% – 94%), 96% CI (92%-100%) and 99% CI (97%-100%) as shown in Figures 2, 3 and 4. These results reveal that with BMI as the reference, the diagnostic characteristics of MUAC (sensitivity, specificity and accuracy) generated by the ROC curve analysis were outstanding.
Based on the coordinates of each curve, Youden’s index was used to determine the optimal MUAC cut-off points to classify nutritional status. Optimal cut off points were identified as those which combined the highest sensitivity and specificity within the standard BMI cut off points. Based on the results of ROC analysis, the MUAC cut offs corresponding to the BMI cut offs are summarised in table 2. Intuitively, these findings suggest that a MUAC of ≥ 31.1cm should be considered obese.
Comparison of Nutrition Status Classification by BMI and MUAC using ROC curves
An analysis of nutritional status classification by MUAC in comparison to the standard BMI cut offs shows that MUAC generates very good estimates for especially underweight (87%), normal weight (72%) and obese (100%) but not overweight (21.4%). Actually 64% of what BMI grouped as overweight was obese by MUAC measures as seen in table 3 below.
Table 3:Nutrition status classification of study group by MUAC in comparison with BMI classification using ROC curve analysis.

Discussion
Several studies have identified limitations with the use of body mass index (BMI) for measuring overweight and obesity. For examples; KJ Rothman et al. [22] in their study stated that although BMI is ideally suited for population-level studies, describing obesity by BMI can result in inaccurate assessment of adiposity, because the numerator in the calculation of BMI does not distinguish lean muscle from fat mass; similarly Kok, P et al. [23] stated that caution should be observed when using the BMI as a measure for interpreting overweight and obesity as body composition can be highly variable yet have the same BMI and therefore, not a reliable measurement of body composition in individuals particularly in older and younger people. In other studies by R, Corral et al. [24] pointed that despite the good correlation between BMI and BF % in a large sample of adults, the diagnostic accuracy of BMI to diagnose obesity is limited, particularly for individuals in the intermediate BMI ranges and C, Vanderwall et al. [25] indicated that BMI appeared to be a good proxy for adiposity and overweight related problems. Like any other measure it is not perfect because it is only dependant on height and weight and it does not take into consideration different levels of adiposity based on age, physical activity levels and sex. Therefore, BMI is a not reasonable indicator of body fat for both adults and children because it does not measure body fat directly, it should not be used as a diagnostic tool. Instead, BMI should be used as a measure to track weight status in populations and as a screening tool to identify potential weight problems in individual [26].
Mid-Upper Arm Circumference (MUAC) is a simple measurement which has been used for many years in nutritional evaluation, being an indicator of protein and energy reserves of the individual. Diverse studies have employed MUAC as a nutritional diagnostic tool in different population groups i.e., inpatients, elderly, schoolchildren, pregnant women or lactating women, adolescent and adult females [4-6,18, 21, 22, 27]. The use of MUAC, which is considered very simple to use, cheap with relatively less technical demand has long been emphasised. However, studies have had varied opinions on how MUAC values can be translated into equivalent BMI cut offs [18, 20, 21,27-29].In all referenced studies so far, there is no consensus on if BMI and MUAC can be used interchangeably to screen nutrition status of adults and what MUAC measures would correspond to the standard BMI cut offs.
Diagnostic screening for malnutrition (underweight, overweight and obesity) in adults is a critical public health measure. Globally, malnutrition in the form of undernutrition or over nutrition has reached epidemic proportions in all age groups. Overweight and obesity have become an epidemic not only in developed world but also in developing world. Overweight and obesity are among the top most attributing factors of disability-adjusted life years [30]. For long, measurement of MUAC has been used as a practical proxy for underweight. However, this study showed that MUAC can be used to determine overweight and obesity and could also be used as a predictive tool for early detection of obesity. The study alsofound a very strong linear relationship between BMI and MUAC defined by the equation BMI= 0.99MUAC -5.82+ ε (Adjusted R2= 0.74, p<0.0001) and Pearson’s correlation coefficient (r = 0.8621, P < 0.0001). This relationship demonstrates that both BMI and MUAC could provide reasonable, equal and comparable measures for nutritional status classification or categorization in adult population with similar demographic characteristics. This findings are in line with studies conducted by A Daset al., Mukherjee, S. et al.,Sultana, T et al.,Tumilowicz A, et al. and S.Garg et al. [2, 27-29] who detected a significant positive correlation between BMI and MUAC (r = (07- 0.8), P < 0.0001) among adults using MUAC as alternate to BMI. In another study where they used bivariate analysis, results showed BMI and MUAC had a positive correlation for both female and male participants, and the relationship between BMI and MUAC was very strong [30].
In categorization of nutritional status by MUAC using ROC curves
to determine MUAC cut offs, the MUAC cut offs established using
ROC curve analysis corresponded well with BMI and overlapped to
a good extent especially in the classification of underweight (87%) and obesity (100%).This is in agreement with the study of A Das
et al. [27] who used ROC curve analysis [28] for the predictive
accuracy to the determined MUAC cutoffs which ranged between
88% and 97%. While this study showed an outstanding diagnostic
characteristics of MUAC with 100% sensitivity for obesity; 90%
for overweight; and 87% for underweight against WHO standard
BMI reference for adult population. This study therefore proposes
the following references, MUAC>31.1cm to indicate obesity,
MUAC =30.1cm to <31.1cm to indicate overweight, MUAC = 25.4
to <30.1cm to indicate normal weight and MUAC ≤ 25.4cm to
indicate underweight respectively. In order to simplify the use of
reference points amongst those with low literacy levels, the study
also proposes the use of colour calibration of the references where
necessary. This is in agreement with S Gary et al. [27] who suggested
colors of traffic light red, yellow, and green could be used to triage
the adults as obese, overweight, and normal.
This study had relatively large sample size with a good range
of age groups and ethnics among the study participants- students
(aged 18yrs+), and teaching staff respectively. Anthropometric
measurements were conducted in the same environment and/or
locality under research conditions by skilled staff. The study is,
however, limited by proportionally fewer female adults compared
to the male adults regardless of ethnicity. Another limitation is
that, BMI is affected by body shape and we did not assess sitting
height to be able to correct BMI for the cormic index (sitting height
to standing height ratio). However, the results were still within our
expected level of precision [31-35].
Conclusions
We concluded that MUAC can be used as an alternative to BMI in the diagnosis of obesity and in early detection of overweight in adults.The finding of this study could contribute significantly to public health interventions in the fight of obesity and associated risk factors in areas where resources are constrained, population largely illiterate and public health prevention measures of obesity related non-communicable diseases such as hypertension, diabetes, etc., which are rising rapidly are not adequately addressed.
Availability of Data and Materials
The datasets used are available from the corresponding author on reasonable request.
Authors’ Contributions
Authors’ Contributions AKA, SJ, TC & MM were involved in all stages from the concept, study design, data gathering, analysis and writing of the manuscript. All the authors approved the final version of the article.
Acknowledgement
We acknowledged the contributions of Department of Food Science and Technology, University of Juba, Andre Foods International
Ethics Approval and Consent to Participate
There was no need for ethical clearance. All Study participants consented to taking part in the study. Confidentiality was assured and maintained. Non-invasive anthropometric measurement procedures were well explained.
References
- World Health Organization (2020) Obesity and overweight. World Health Organization, Switzerland.
- Tremmel M, Gerdtham UG, Nilsson PM, Saha S (2017) Economic Burden of Obesity: A Systematic Literature Review. International journal of environmental research and public health 14(4): 435.
- Withrow D, Alter D (2011) The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev 12(2): 131‐141.
- Casadei K, Kiel J (2020) Anthropometric Measurement In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
- Luma HN, Eloumou S, Mboligong FN, Temfack E, Donfack OT, Doualla MS (2017) Malnutrition in patients admitted to the medical wards of the Douala General Hospital: A cross-sectional study. BMC Res Notes 10: 238.
- Sánchez-García S, García-Peña C, Duque-López MX, Juárez-Cedillo T, Cortés-Núñez AR, et al. (2007) Anthropometric measures and nutritional status in a healthy elderly population. BMC Public Health 7: 2.
- Nguyen P, Ramakrishnan U, Katz B, Gonzalez-Casanova I, Lowe AE, (2014) Mid-upper-arm and calf circumferences are useful predictors of underweight in women of reproductive age in northern Vietnam. Food Nutr Bull 35: 301-311.
- Lee R, Nieman D (2003) Nutritional assessment.Mc Graw Hill; New York, USA.
- Nube M, Asenso-Okyere WK, van den Boom GJ (1998) Body mass index as indicator of standard of living in developing countries. Eur J Clin Nutr 52: 136-144.
- FAO (2019) Defining chronic energy deficiency. FAO.
- Chakraborty R, Bose K, Koziel S (2011) Use of mid-upper arm circumference in determining undernutrition and illness in rural adult Oraon men of Gumla District, Jharkhand, India. Rural Remote Health 11: 1754.
- Sultana T, Karim MN, Ahmed T, Hossain MI (2015) Assessment of under nutrition of Bangladeshi adults using anthropometry: Can body mass index be replaced by mid-upper-arm-circumference? PLoS One p. 10.
- Briend A, Garenne M, Maire B, Fontaine O, Dieng K (1989) Nutritional status, age and survival: The muscle mass hypothesis. Eur J ClinNutr 43(10): 715-726.
- Gassull MA, Cabré E, Vilar L, Alastrue A, Montserrat A (1984) Protein-energy malnutrition: An integral approach and a simple new classification. Hum Nutr ClinNutr. 38(6): 419-431.
- Wijnhoven HA, van Bokhorst-de van der Schueren MA, Heymans MW, de Vet HC, Kruizenga HM, et al. (2010) Low mid-upper arm circumference, calf circumference, and body mass index and mortality in older persons. J Gerontol A BiolSci Med Sci 65(10): 1107-1114.
- Brito N B, Llanos JPS, Ferrer MF, Garcia JGO, Brito ID, et al. (2016) Relationship between mid-upper arm circumference and body mass index in inpatients. PLoS One 11(8).
- Bhattacharya A, Pal B, Mukherjee S, Roy SK (2019) Assessment of nutritional status using anthropometric variables by multivariate analysis. BMC public health 19(1): 1045.
- Diverse Populations Collaborative Group (2005) Weight‐height relationships and body mass index: some observations from the Diverse Populations Collaboration. American journal of physical anthropology 128(1): 220-229.
- Sultana T, Karim MN, Ahmed T, Hossain MI (2015) Assessment of under nutrition of Bangladeshi adults using anthropometry: Can body mass index be replaced by mid-upper-arm-circumference? PloS one 10(4).
- Young H, Jaspars S (2009) Review of nutrition and mortality indicators for the Integrated Food Security Phase Classification (IPC): Reference levels and decision-making. Inter-Agency Standing Committee Nutrition Cluster.
- BM Marriots (1990) Body Composition Measurement: Accuracy, Validity, and Comparability.
- Rothman KJ (2008) BMI-related errors in the measurement of obesity .Int J Obes (Lond) 32 (Suppl 3): S56-S59.
- Kok P, Seidell Jaap, Meinders AE (2004) [The value and limitations of the body mass index (BMI) in the assessment of the health risks of overweight and obesity]. Nederlands tijdschriftvoorgeneeskunde. 148: 2379-2382.
- Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, et al. (2005) Accuracy of body mass index in diagnosing obesity in the adult general population. International journal of obesity 32(6): 959-966.
- Vanderwall C, Randall Clark R, Eickhoff J, Carrel AL (2017) BMI is a poor predictor of adiposity in young overweight and obese children. BMC pediatrics 17(1): 135.
- United States Center for Diseases Control, CDC.
- http:/www.cdc.gov/healthyweight/assessing/bmi/
- Das A, Saimala G, Reddy N, Mishra P, Giri R, et al. (2020) Mid-upper arm circumference as a substitute of the body mass index for assessment of nutritional status among adult and adolescent females: learning from an impoverished Indian state. Public health 179: 68-75.
- Lillie M, Lema I, Kaaya S, et al. (2019) Nutritional status among young adolescents attending primary school in Tanzania: Contributions of mid-upper arm circumference (MUAC) for adolescent assessment. BMC Public Health 19:
- NéstorBenítez Brito, José Pablo Suárez Llanos, Manuel Fuentes Ferrer, Jose Gregorio Oliva García, et al. (2016) Relationship between Mid-Upper Arm Circumference and Body Mass Index in Inpatients. Public Library of Science, 11(8): 1-10.
- Tang AM, Dong K, Deitchler M, Chung M, Maalouf-Manasseh Z, et al. (2013) Use of Cutoffs for Mid-Upper Arm Circumference (MUAC) as an Indicator or Predictor of Nutritional and Health-Related Outcomes in Adolescents and Adults: A Systematic Review. Washington DC, USA.
- Kondrup J, Rasmussen HH, Hamberg O, Stanga Z (2003) Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. ClinNutr 22(3): 321-336.
- Bhattacharya A, Pal B, Mukherjee S, et al. (2019) Assessment of nutritional status using anthropometric variables by multivariate analysis. BMC Public Health 19:
- Shobhit Garg, Bijit Biswas, Swanya P Maharana, Aparajita Dasgupta (2017) Potential of mid-upper arm circumference to replace body mass index as a screening tool for assessment of nutritional status: A study among a rural elderly population in eastern India. National Journal of Physiology, Pharmacy and Pharmacology.
- Youden WJ (1950) Index for rating diagnostic tests. Cancer 3: 32-35.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...