Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Research ArticleOpen Access 
Irrational Use of the Treatment for H. Pylori Guidelines Volume 1 - Issue 4
Ahmed M Masaad1*, Hazazi Y Sarah2 and Hazazi Yamal2
- 1Department of Pharmaceutics and Industrial Pharmacy, College of Pharmacy, Taif university, Saudi Arabia
- 2College of Pharmacy, Taif university, Saudi Arabia
Received: January 25, 2020 Published: February 11, 2020
Corresponding author: Ahmed MA Masaad, Assistant Professor of Pharmaceutics, Department of Pharmaceutics and Industrial Pharmacy, College of Pharmacy, Taif university, Saudi Arabia
Abstract
The gastric ulcer is epidemic disease in many countries the main cause of the disease is helicobacter pylori which transfers by polluted foods. Many protocols and guidelines for the treatment and the most common guidelines is triple therapy Amoxicillin, Clarithromycin and proton pump inhibitors, but now the resistant to this protocol due to irrational use of the antibiotics. The study was done on the Helicobacter pylori by Kirby-Bauer sensitivity Test method which clarify that one of the components of the triple therapy clarithromycin, which failed to pass the test which indicates the retarding in the recovery to H. Pylori that open road to put new guidelines for H. Pylori especially in countries widely and irrationally use antibiotics. The study recommended that to put new guidelines and studies about the growing of resistant to antibiotics.
Keywords: H. Pylori; Protocol; Treatment; Antibiotic; Amoxicillin; Resistance; New Guidelines
Introduction
Background
Peptic ulcer disease (PUD) occurs when there is mucosal erosion within the gastrointestinal tract. The ulcer in PUD extend deeper into mucosa. The three-common cause of PUD are H. pylori, Non-steroidal anti-inflammatory drug (NSAIDs) induced ulcer and stress ulcer, which across in the presence of mechanically ventilated patient and critical illness [1].
Helicobacter pylori is found primarily in gastric antrum of the humane stomach, gram-negative microaerophilic and lived in acidic media. H. pylori represent (80-85%) of gastric ulcers. Pathophysiology associated with H. pylori involves the production of cytotoxins associated with gen A (CagA) proteins and vacuolating cytotoxin, such as vac A, which activate the inflammatory cascade. Cag A status are predictors of ulcerogenic capacity of strain. H. pylori produced number of enzymes causing tissue damage and include urease, hemolysis and neuraminidase. The main hormone involved in stimulating gastric acid secretion is gastrin. The hyperacidity in duodenal ulcer may result from hypergastrinemia caused by H. pylori. Consequence of bacterially mediated decrease of antral D cells that secrete somatostatin result from elevation of gastrin, those losing the inhibitory modulation of somatostatin on gastrin, or by the inflammatory process. The inflammatory process is across by direct stimulation of gastrin cells. Increased partial cell mass cause long standing hypergastrinemia [1,2].
The symptoms and clinical manifestations
Peptic ulcer disease are dyspepsia, nausea, vomiting, anorexia, heartburn, cramping, bloating, abdominal pain is most frequent symptom of PUD burning and precipitate of ulcer pain with food [1].
The diagnosis
H. pylori infection by using endoscopic and non-endoscopic tests. The endoscopic test is costly, awkward and ordinarily require a mucosal biopsy for culture, histology, and location of urease movement while the non-endoscopic tests contain serologic counteracting agent location tests for identity circulating immunoglobulin G coordinated agonist H. pylori, the urea breath test utilized for location urease generation by H. pylori, and stool antigen test. The hemoglobin, hematocrit and stool hemoccult tests are utilized to identify dying) [3].
Complication of peptic ulcer
The urea breath test utilized for location urease generation by H. pylori, and stool antigen test. The hemoglobin, hematocrit and stool hemoccult tests are utilized to identify bleeding. Perforation is happening as a sudden, sharp, starting to begin with within the epigastrium but quickly spread over the complete midriff and serious pine [3].
Epidemiology Saudi Arabia
Saudi Arabia is a developing country have good socioeconomic status. The prevalence rate in Saudi Arabia is 40% in age group of 5-10 years and 70% in people older than 20 years of age H. pylori infection it’s makes of highest endemic areas in world [4].
Goals of treatment
To healing the ulcer, relieving ulcer pain, preventing recurrence ulcer and redaction complication of ulcer. In patient have H. pylori positive an dynamic ulcer, a history of ulcer or an already recorded ulcer, the objective for this condition are destruction of living being case ulcer, mend the ulcer after killed life form and remedy malady agreeing taken a toll and compelling sedate regimen [3].
The treatment of H. pylori
According American guideline in Saudi Arabia by triple thereby and by fifth therapy (sequential). Triple thereby is amoxicillin, protein pump inhibitor (PPI) and Clarithromycin. And sequential is protein pump inhibitor (PPI) + amoxicillin (1g), protein pump inhibitor (PPI) + Clarithromycin (500 mg) + metronidazole (500 mg) [5]. In the other country like Asia in 2015 not have any alternative treatment to avoid resistance to antibiotics just increase dose of PPI [6]. And in the study doing in Iran levofloxacin is more preferred than clarithromycin if used in sequential therapy, vonoprazan is potassium-competitive acid blocker (P-CAB), vonoprazin orally available and cheaper than PPI and used in place of PPI in triple therapy in Japan [7]. But in Korea prevalence no resistance to metronidazole but increase prevalence of resistance with clarithromycin in dual therapy and need to antibiotics susceptibility test is necessary for prepatient [8]. In Bangladesh and in Africa therapy resistant to first line treatment of H. pylori the first line is metronidazole, amoxicillin and clarithromycin and have resistant to levofloxacin for patient in Bangladesh [9,10]. And in 2014 in Saudi Arabia the prevalence of resistant to antibiotics used in treatment of H. pylori is high for first line is 4% clarithromycin, 1% amoxicillin and metronidazole 80% and the alternative is tetracycline, amoxicillin and levofloxacin [4]. And in 2015 the effective of triple therapy and sequential thereby is similar in treatment of H. pylori and prevalence to resistance to clarithromycin 23.3%, amoxicillin 14.8% and 48.5% in metronidazole [11].
One of the reasons for the expanded resistance of H. pylori bacteria in Saudi Arabia is the irrational use of antibiotics. For example, amoxicillin is effective in America while it is resistant in Saudi Arabia as well as unlimited sales of antibiotics in Saudi Arabia and empirical treatment of the disease before sampling and testing Non-adherence to the specific treatment period for this drug occurs frequently in patients with stomach ulcers [12].
Antibiotics resistant mechanism for H. pylori
Bacteria are developing resistance to various antibiotics that Enables them to withstand the harsh environment and multiply. The ways bacteria antimicrobial resistance is mutagenesis Disable the binding site of antibiotics, pump, and flow Horizontal gene transfer has been proposed. For example, resistance to Metronidazole mainly related to mutagenesis Inhibition of gene associated with reduction and oxidation (frxA and rdxA) [4].
The frxA gene may sometimes act indirectly by affecting cellularity. Low potential at low levels of metronidazole insulation resistance. Modifications in the rdxA gene such as deletion in the gene the pump flow system is also of great importance it was not possible to choose a clear board from this point mutations that can explain this phenomenon. In short, modification or loss of these genes may lead to metronidazole resistance. Quite the opposite. For clarithromycin, resistance the mechanism of convergence between ribosomes and clarithromycin is reduced. That’s because the boom 23S rRNA gene in 2143 and 2144 function. In India, the result of a mutation in the nitrogen chromosome rdxA the gene, while in Bangladesh, is resistant to metronidazole inhibiting the rdxA gene to give the metronidazole phenotype. Saudi Arabia also suffers from pylori resistance [4].
The aim of this study is to set up a new standard and regimen within the treatment of stomach ulcers caused by H. pylori [4].
Microbiological Test
Microbiological test was done on isolated of H. pylori to study the effectiveness of antibiotics use in American guideline, also the test was done by other antibiotics to see their effect on this microorganism. Amoxicillin, Clarithromycin, and Amoxiclav acid Sensitivity Test using Disc diffusion Kirby-Bauer Sensitivity Test to study the effect of the antibiotics in the triple treatment of the Helicobacter Pylori and other antibiotics not present in the guideline.
Antibiotic disc preparation
A. The filter paper was cut to a diameter of 4 mm and then placed in a sealed container and then sterilized the filter paper in the oven.
B. The disks were impregnated with antibiotics (Amoxicillin and Clarithromycin and co-Amoxiclav) test suspensions in the oven at 60°C for minutes then serial dilution was carried out to obtain the concentration 10μg/ml as below equation: (Dissolve 1mg in 10ml and then the serial dilution was done according to the below equation):
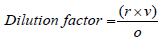
Where:
o: is the original concentration
r: is the needed concentration
v: is the needed volume
Inoculums was done from isolated bacteria under test.
H.pylori. Inocula are prepared by the direct inoculating colonies which grown overnight on Mueller Hinton agar, into the broth media. Then the H. Pylori tested was standardized by using McFarland turbidity test standard, Inoculums preparation is the most critical step in the any susceptibility test.
McFarland turbidity standards
The McFarland 0.5 standard is prepared and was used in this experiment, which consist of 99.5 ml of 1% sulfuric acid and 0.5 ml of 1.175% barium chloride, this solution is transferred into tubes comparable to those used for the inoculum’s preparation.
The McFarland 0.5 standard gives the turbidity comparable to that turbidity of the bacterial suspension containing 1.5×108CFU/ ml.
Inoculation and incubation
After making the standard inoculums suspension, a sterile cotton swab was dipped into a turbid suspension, squeezed to remove the excess suspension, and then swabbed gently across surface of a agar plate (plates of 9mm are used) which Mueller Hinton agar was used. (Each the inoculum suspension was inoculated into two media labeled test (T) and control(C)).
a) Within quarter an hour the inoculation, of the Amoxicillin, Clarithromycin, and Amoxiclav disks are applied to selected agar media with forceps and smoothly pressed to ensure contact with the surface of the agar.
b) The Amoxicillin, Clarithromycin and amoxicillin/ Clavulanic acid Test disks are applied in plates labeled (T)
c) While another plate’s labeled (c) without any antibiotic disks for control microbial growth.
d) Within quarter an hour of the disk’s placement, the plates are inverted and placed into oven at 37°C for 19 hours.
e) After incubation, the plates were tested, to ensure test organisms have grown satisfactory, the diameter of each inhibition zone was measured using ruler or calipers.
f) then zone of inhibition was measured in millimeters for each drug from Amoxicillin, Clarithromycin, and amoxicillin/ Clavulanic acid compared with that found in the standard tables of the NCCLS documents (The national committee for clinical laboratory standards) [13].
Results and Discussion
The result of study shown that clear resistant to Clarithromycin and weak inhibition zone to Amoxicillin that result in agreement with Yoshio Yamaoka et al. [6] which summarize that In the other country like Asia in 2015 not have any alternative treatment to avoid resistance to antibiotics just increase dose of PPI [6]. same result by Anthony O’Connor et al. [7] which concluded that in study done in Iran levofloxacin is more preferred than clarithromycin if used in sequential therapy. Another finding by O’Connor that vonoprazan is potassium-competitive acid blocker (P-CAB), vonoprazin orally available and cheaper than PPI and used in place of PPI in triple therapy in Japan Eun CS et al. [8]. Another resemblance study by Eun et al. [8] in Korea that prevalence no resistance to metronidazole but increase prevalence of resistance with clarithromycin in dual therapy and need to antibiotics susceptibility test is necessary for prepatient Eun, et al. [8]. Those results in same matching with Hafeza A et al. [9] In Bangladesh and in Africa that the therapy resistant grown to treatment of H. pylori the first line is the metronidazole, amoxicillin and clarithromycin and have resistant to levofloxacin for patient in Bangladesh [9, 10]. Also in 2014 in Saudi Arabia the prevalence of resistant to antibiotics used in treatment of H. pylori is high for first line is 4% clarithromycin, 1% amoxicillin and metronidazole 80% and the alternative is tetracycline, amoxicillin and levofloxacin by Mohammed R et al. [4] which agree with finding of this study also another same results by Fahad A et al. [11] which reflect that the effective of triple therapy and sequential thereby is similar in treatment of H. pylori and prevalence to resistance to clarithromycin 23.3%, Amoxicillin 14.8% and 48.5% in metronidazole [11,14,15].
Conclusion
The study found that high percentage of resistant to triple treatment protocol for H. Pylori due to might be for irrational use of antibiotics in Middle East countries and Africa compared to America and Europe.
Recommendations
This research recommend to distribute this study to make survey for the same drugs used in the triple treatment of H. Pylori and connected with this study furthermore to change the guidelines of triple treatment by using different antibiotics instead of macrolide with amoxicillin like Amoxicillin/Clavulanic acid for instance, due to the sensitivity to antibiotics in middle East countries and Africa not like America and Europe in restrictions laws for dispensing antibiotics.
The study invites all health practitioner to be restricted in dispensing the antibiotics and after ensure by making culture media.
Ethical clearance
Taken from College of Pharmacy Taif University and Alneelain University.
References
- Cameron LEAJ, Bonin RP (2019) AACP REPORT. American Journal of Pharmaceutical Education 83(5): 7654.
- Walker R (2011) Clinical Pharmacy and Therapeutics E-Book. Elsevier Health Sciences, Netherland.
- Di Piro, BGWJT, DiPiro, TLSCV (2015) Pharmacotherapy Handbook. (9th ) Barbara G Wells (Ed.) by McGraw-Hill Education, USA.
- Mohammed Rizwan NF, Alvi A (2014) Epidemiology and pattern of antibiotic resistance in Helicobacter pylori: Scenario from Saudi Arabia. Saudi journal of gastroenterology 20(2): 212-218.
- Chey WD, Leontiadis GI, Howden CW, Moss SF (2017) ACG clinical guideline: Treatment of Helicobacter pylori The American journal of gastroenterology 112(2): 212-239.
- Miftahussurur M, Yamaoka Y (2015) Appropriate first-line regimens to combat Helicobacter pylori antibiotic resistance: An Asian perspective. Molecules 20(4): 6068-6092.
- O'Connor A, Lamarque D, Gisbert JP, O'Morain C (2017) Treatment of Helicobacter pylori infection 2017. Helicobacter 22(1): e12410.
- Eun CS, Han DS, Park JY, Jeon YC, Hahm JS, et al. (2003) Changing pattern of antimicrobial resistance of Helicobacter pylori in Korean patients with peptic ulcer diseases. Journal of gastroenterology 38(5): 436-441.
- Aftab H, Miftahussurur M, Subsomwong P, Ahmed F, Khan, et al. (2016) Helicobacter pylori antibiotic susceptibility patterns in Bangladesh: Emerging levofloxacin resistance. The Journal of Infection in Developing Countries 10(03): 245-253.
- Jaka H, Rhee J A, Östlundh L, Smart L, Peck R, et al. (2018) The magnitude of antibiotic resistance to Helicobacter pylori in Africa and identified mutations which confer resistance to antibiotics: Systematic review and meta-analysis. BMC infectious diseases 18(1): 193.
- Alsohaibani F, Al Ashgar H, Al Kahtani K, Kagevi I, Peedikayil M, Alfadda, et al. (2015) Prospective trial in Saudi Arabia comparing the 14-day standard triple therapy with the 10-day sequential therapy for treatment of Helicobacter pylori Saudi journal of gastroenterology21(4): 220-225.
- Alhomoud F, Almahasnah R, Alhomoud FK (2018) “You could lose when you misuse”-factors affecting over-the-counter sale of antibiotics in community pharmacies in Saudi Arabia: A qualitative study. BMC health services research 18(1): 915.
- Koletar SL (2000) Concepts in Antimicrobial Therapy. In: Textbook of Diagnostic Microbiology (2nd) by WB Saunders, USA.
- Ang TL, Almadi MA (2015) Selecting the optimum first-line treatment for pylori eradication. Saudi journal of gastroenterology 21(4): 183-184.
- Littmann J, Rid A, Buyx A (2017) Tackling anti-microbial resistance: Ethical framework for rational antibiotic use. The European Journal of Public Health 28(2): 359-363.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...