Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Research ArticleOpen Access 
Functional to 12 Months of Surgery of Coverage and Results Acetabular Reorientation Displasia Development in the Hip Volume 2 - Issue 1
Segura Martínez José Guadalupe* and Cervantes Gudiño Jorge
- Centenario Hospital Miguel Hidalgo CHMH, Aguascalientes, México
Received: March 03, 2020 Published: April 06, 2020
Corresponding author: Segura Martínez José Guadalupe, Centenario Hospital Miguel Hidalgo CHMH, Aguascalientes, México
Abstract
Introduction: DDH progressive disorder of the acetabulum, joint capsule and proximal femur with muscles and ligaments, altered. Treatment depends on age and stage of diagnosis, acetabular osteotomy maintained after 18 months as articular cartilage contact surface between the acetabulum and the femoral head.
Objective: To determine functional outcomes to 12 months of surgery coverage and acetabular reorientation in developmental dysplasia of the hip.
Methods: Included patients with type Pelvic osteotomy Pemberton and Pelvic osteotomy type Salter, follow up of 12 months, variables were age, sex, acetabular congruency, CE Wiberg angle, acetabular index, functional scale of Harris and Severin, Tönnis Rating Scale satisfaction postoperative SF-36, running, cross-type cross-over study, observational, descriptive, crosssectional, analytical, review of medical records, clinical examinations, preoperative and postoperative radiographs.
Results: 17 patients, 19 hips, DDH diagnosed with acetabular reorientation osteotomy group I and group II acetabular coverage, 16 patients, 9 patients, 12 hips with Salter osteotomy, primary care average 15.75 months, Severin preoperative functional class IV B 12 hips (100%), postoperative functional class IA 4 hips (33.33%), IIA 4 hip (33.33%), Harris points preoperatively to 75.29 regular function 100%, postoperative 89.66 points, good functional results 9 patients 75% (86- 89 points), excellent results 25% (93-97 points), patient satisfaction excellent 50% 6 patients, 5 hips good 41.66% satisfaction. 11 Group II 7 hips acetabular osteotomy coverage, primary health 33.57 months, Severin classification presurgical functional class III 4 hips (57.14%), postoperative functional class IA one hips (14.28%), IIA 2 hip (28.57%), IB three hip 42.85%, ranking Harris were found in pre-surgical regular function with 73.21 points 5 patients the 71.42%, 87.65 points postsurgical, good functional outcome 6 patients 85.71% (84.6-88 points), patient satisfaction 42.85% 3 patients excellent, 4 good satisfaction hips 57.14%, 5 hips 71%.
Conclusion: Patients treated of DDH with surgery coverage and acetabular reorientation in developmental dysplasia of the hip have good functional results.
Keywords: Developmental dysplasia of the hip (DDH)
Introduction
Developmental dysplasia of the hip (DDH) occupies great attention in our hospital environment, since in the current literature we find an incidence 1.5 worldwide, and 2 to 6 per 1000 (Statistics in Mexico) due to the low reporting of results of the management of developmental dysplasia of the hip in our country Untreated developmental dysplasia of the hip (DDH) in the older child has become uncommon in the first world, but it is still seen in developing Countries [1].
Developmental Dysplasia of the Hip
It is defined as a progressive disorder, in which the acetabulum, the joint capsule and the proximal femur, together with their muscles and ligaments, are altered. It comprises a spectrum of disorders characterized by an abnormal relationship and/or anatomy of the acetabulum and the proximal portion of the femur [2-5]. This spectrum ranges from the unstable hip of the newborn to its dislocation, including subluxation and isolated malformation or insufficiency of the acetabulum.
Etiology
For a proper development of the hip to occur, the femoral head must be correctly centered in the acetabulum and there must be a balance between the growth of the triradiated and acetabular cartilages, any alteration in this balance, either in the period intrauterine or postnatal, will lead to altered development of the hip, it is multifactorial and hormonal, mechanical and genetic factors have been related [6-14].
Pathophysiology
Variable magnitude changes occur in the dysplastic hip, both in the acetabulum and in the proximal femur and soft tissue [2- 6]. Modifications occur over time, due to age and load, and lead to adaptive changes in the joint. Pulvinar fat, teres ligament, labrum, and joint capsule hypertrophy; and the transverse ligament is reversed. The abnormal pressure of the dislocated or subluxated femoral head on the labrum causes hypertrophy of the fibrocartilage and forms fibrous tissue. This labrum can be everted and adhered to the internal face of the joint capsule.
Treatment
The Pavlik harness is the most used method in the treatment of DDH in children from birth to 6 months of age. Pavlik harness success reaches 95% (Figure 1) In case of failure with Pavlik harness Once the open or closed reduction has been achieved, it will be maintained by a pelvic plaster for 3 months. Femoral osteotomies, consisting of varicose and defeat osteotomies, are performed to stabilize hip reduction and to stimulate acetabulum development. Increased femoral anteversion is the most frequent cause of recurrence of subluxation, and therefore, derotatory femoral osteotomy is necessary in some cases to achieve articular consistency, an essential requirement to perform any osteotomy. The acetabular osteotomies described in the literature can be divided into 2 groups: osteotomies that maintain the articular cartilage as a contact surface between the acetabulum and the femoral head; and so-called salvage osteotomies, which do not. The former are divided, in turn, into osteotomies that alter orientation, Salter’s osteotomy (Figures 2-4.) Steel’s triple osteotomy and osteotomies that alter acetabular shape and coverage (Pemberton’s osteotomy, Dega’s osteotomy).
Objective
To find out the radiographic results, and compare them with the functional results 12 months after surgery. Predict the postsurgical radiographic and functional results. Compare results with world literature.
Methods
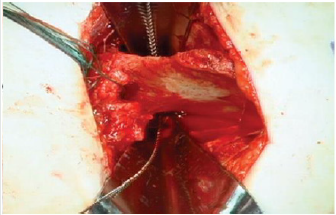
Follow-up of all patients with a diagnosis of developmental dysplasia of the hip who underwent coverage osteotomy and acetabular reorientation, and with a 1-year follow-up of postsurgical patients in CHMH where clinical records, hip functionality table were analyzed , Harris Hip Score, Severin’s functionality table, Surgical technique: Salter-type acetabular reorientation osteotomy; Surgical protocol is performed by performing adductor and iliopsoas myotenotomy (MAP) (Figure 2). Smith Peterson-type approach is performed, hip reduction is verified (Figure 3), and an acetabular osteotomy is performed, which is performed by lifting with The periosteum and gauze elevator is bluntly dissected until reaching the minor sciatic notch, and a Gigli-type saw cut is made between the anterior superior iliac spine and a transverse cut is made in the uninominated bone (Figure 4), proceed to make an iliac bone wedge in a triangular shape, with a forceps proceed to place skin and field forceps, acetabular reorientation is performed by performing anterior, lateral and caudal displacement (Figure 5) by placing an autologous graft in the area osteotomy, placing 2 Kirschnner 0.062 nails to maintain graft, hip reduction is performed, kirschnner 2.0 transcervical nail is placed which maintains reduction (Figure 6), capsulorrhaphy is performed.
The Acetabular Cover Osteotomy: Pemberton type, the same approach is performed, an osteotomy with a curved chisel is performed (Figures 7-9), taking as reference the anterior superior iliac spine and the inferior one at its midpoint, periacetabular with inclination of 15oC directed towards the triradiated cartilage, where the fulcrum and maintained with autologous bone graft; placing nails according to osteotomy stability.
Results
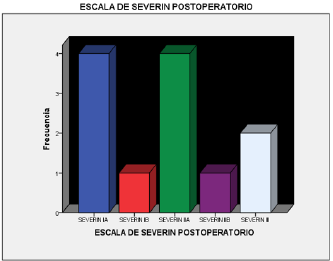
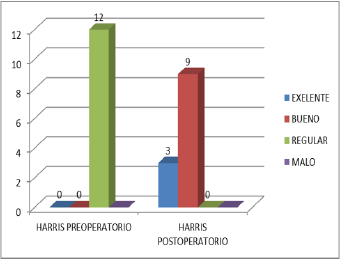
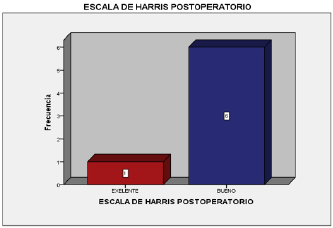
An observational study of 17 patients, 19 hips, with a diagnosis of developmental dysplasia of the hip, who underwent surgical treatment with group I acetabular reorientation osteotomy and group II acetabular coverage, was performed. Only 16 patients were included. Due to the diagnosis of PCI, 9 patients, 12 hips, a Salter-type acetabular reorientation osteotomy was performed where 8 patients (88.8%) had a diagnosis of bilateral CDD and 1 patient (11.11%), with a diagnosis of left DDH, had been performed in 2 patients. previous MAP surgeries plus open reduction in 2 patients (22.22%) and in 7 where no previous procedures had been performed (77.77%), the age of primary care was 17.3 months, (5- 28 months), the age at that surgery was performed was on average 21.5 months, (8-31 months), average follow-up of 20.8 months (15- 26 months), in total there were 6 female patients (66.66%) and 3 male patients (33.33%), with a pre-surgical Tönis classification of 6 type III hips (50%) and 6 type IV hips (50%), in the postoperative period 4 hips with Tönnis I (33.33%), 6 hips Tónnis II (50%), 2 hips Tönnis III (16.66%), with CE angle pre-surgical Wiberg average -20 C, (-8, -54°C), in the postoperative average of 24.1°C (13- 30°C), with a correction of 43.25°C (30-54°C), with a preoperative acetabular index of 41.5°C (22°C -42°C), postsurgical of 21.3°C (20-24°C) average correction of 20 °C, the Calve and Shenton lines in the preoperative were found inconsistent in 11 hips (91.66%), and congruent in 1 patient 8.44%, in the postoperative period. 10 hips were found congruent (83.33%), incongruous in 2 patients (16.66%), in the pre-surgical Severin classification, we found 12 hips (100%) in functional class IV B, in the postqu surgical functional class IA 4 hips (33.33%), IIA 4 hip (33.33%), IB 1 hip 8.33%, IIB 1 hip 8.33%, III 2 hips 16.66%, in the Harris functional classification they were found in the preoperative with 75.29 points on average with 100% regular function of the hips, in the postoperative period 89.66 points average, with good functional result 9 patients 75% (86-89 points), excellent result 25% (93- 97 points), patient satisfaction was classified as according to the current postoperative period, it was 50% 6 patients excellent, 5 hips with good satisfaction 41.66%, 1 patient with regular satisfaction 8.33%, 6 hips 50% currently have a positive Trendelemburg gait, 2 complications were observed, 1 leak of the cervical nail and hip subluxation.
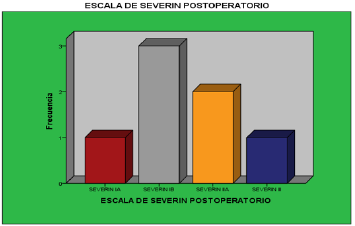
In group II, acetabular covering osteotomy was performed in 7 hips, where 5 patients (71.5%) had a diagnosis of bilateral DDH and 2 patient (28.57%), with a diagnosis of right DDH, had undergone 3 previous MAP surgeries. more open reduction in (42.85%) and in 3 patients Myotenotomy for adductors and iliopsoas(MAP) more open reduction plus osteotomy for varicose veins, 1 hip where no previous procedures had been performed (14.28%), Myotenotomy for adductors and iliopsoas plus open reduction plus Salter-type osteotomy 1 patient (14.28%) the age of primary care was 31.1 months, (13-60 months), the age at which surgery was performed was on average 45 months, (31-120 months), average followup of 20.5 months ( 23-26 months), in total there were 6 female patients (100%), with a pre-surgical Tönis classification of 4 hips type II, (57.14%) and 3 hips type III, (42.85%), and 1 hip with type IV 14.28%, in the postoperative 4 hip s with Tönnis I (57.14%), 3 hips Tónnis II (42.85%), with CE angle pre-surgical Wiberg average 7°C, (-34 C, 20°C), in the postoperative average of 38.14°C (29- 52°C), with a correction of 25.14°C (12-63°C), with a preoperative acetabular index of 31.85°C (20°C -43°C), postsurgical 23.3°C(20- 28°C) average correction of 8.8°C, the Calve and Shenton lines In the pre-surgical period, incongruous were found in 6 hips (85.71%), and in 1 patient, 14.28% were congruent. , we found functional class III 4 hips (57.14%), 1 patient IV A (14.28%) and IVB 2 hips (28.57%), in the postoperative functional class IA 1 hips (14.28%), IIA 2 hip (28.57%), IB 3 hip 42.85%, III 1 hip 14.28% in the Harris functional classification, 73.21 points on average with regular function were found in the preoperative with 5 patients, 71.42% of the hips, 1 poor result 14.28 %, and 1 good result 14.28%, in the postoperative period 87.65 average points, with good functional result 6 patients 85.71% (84.6-88 points), excellent result 1 patient 14.28% (92.2 points),
patient satisfaction was classified as according at the current postoperative period it was 42.85% 3 patients excellent, 4 hips with good satisfaction 57.14%, 5 hips 71% currently have a positive Trendelemburg gait, limitation of arches of mobility was observed in 1 patient who did not undergo rehabilitation.
Discussion
The efficacy of conservative methods decreases after the first 18 months of life, continuing with instability after treatments, this residual instability is caused by frontal inclination of the acetabulum, with a decrease in lateral and anterior orientation, this causes head coverage. Femoral, this combination with excessive femoral anteversion increases acetabular dislocation, and causes the failure of conservative treatments and open hip reductions [15-17]. The age of primary care was 17.3 months, the age at which surgery was performed was 21.5 months, the age of primary care was late, and the age at which we performed the procedures are consistent with the surgical indications established by the authors of the Surgical techniques published after 18 months and before 9 years [6, 9]. The 20-month follow-up obtained for group I in the postoperative Severin classification according to the Severin criteria [2] excellent and good results in 75% greater than those found in other Vengust series 73% [11], and it is variable according to other authors, from 41 to 100% (6,10,11,15,16,18) in Harris functional classification, in the postoperative period 89.66, with good functional result 75% (86-89 points), excellent result 25%, patient satisfaction was classified as according to the final postoperative period was good and excellent 91.66%, results obtained by Salter 93.6% in his series, in another series [10] 78.9% obtained good radiographic and functional results, very consistent with those obtained in this study, who followed the same surgical technique and with an average 13-year follow-up.
It is important to mention that after the Salter type osteotomy, the acetabular coverage and the growth of the proximal femur are the most important factors in the prognosis, it is the CE angle of Wiberg that determines this factor, in our sample consistent with the results obtained was 24.1°C (13-30°C), with a correction of 43.25°C (30-54°C) consistent with other studies [8-10] lateral acetabular coverage of the femoral head where it is said that the correction that can be performed with this osteotomy it is from 10 ° to 21°C Utterback and Mc Ewen (11,22), Morscher 6°C -12°C* 10 [12] our acetabular index obtained preoperatively from 41.5°C (22°C -42°C), postsurgical from 21.3°C (20-24°C) average correction of 20 ° this difference can be explained by the poor results obtained in hip reduction, or errors in measuring the acetabular index when obtaining poor radiographs [10], It is difficult to compare the results of different series why the results Post-surgical years change according to the period of time in which they are performed, surgical age is associated with better postsurgical results, some authors exclude patients with femoral head necrosis data prior to surgery [18,19].
Conclusion
Patients with DDH treated at Centenario Hospital Miguel Hidalgo with coverage surgery and acetabular reorientation in developmental dysplasia of the hip have good functional results.
References
- Robert Bruce Salter (2010) J Bone Joint Surg Am 92: 2139.
- Dra Anabel Flores, Pablo Castañeda Leeder (2010) Tratamiento De La Displasia Del Desarrollo De La Cadera Tipo Graf II Y IV Con El Arnés De Pavlik. Rev Mex Ortop Ped 12(1): 19-23.
- Tymothy Wardm W, Molly Voghtph D, Pittsburgh Severin D (1997) Classification System For Evaluation Of The Results Of Operative Treatment Of Congenital Dislocation Of The Hip. J Bone Joint Surg 79(5).
- Moraleda J, Albi˜nana M, Salcedo G (2012) Displasia Del Desarrollo De La Cadera L. Rev Esp Cir Ortop Traumatol 10: 1-11.
- Juan Ricardo Benavides Molineros, Dra Claudia Liliana Figueroa Gómez (2012) Revisión De Conceptos Actuales Displasia De La Cadera En Desarrollo. Rev Col Or Tra 26(1): 50-60.
- Stuart L Weinstein Md, Scott J Mubarak Md, Dennis R Wenger (2003) Development Hip Dysplasia And Dislocation Part I. The Journal of Bone & Joint Surgery 85(9).
- Simon R Thomas, Ma Frcs(Tr&Orth), Robert B Salter (2007) Frcs(C) Outcome At Forty-Five Years After Open Reduction And Innominate Osteotomy For Late-Presenting Developmental Dislocation. The Hip Surgical Technique Jbjs 89: 2341-2350,
- GeorgeT Rab (1978) Biomechanical Aspects Of Salter Osteotomy Gerrget. Clinical Orthopedics And Related Research 130(1).
- Paul A Pemberton (1965) MDT Pericapsular Osteotomy Of The Ilium For Treatment Of Congenital Subluxation And Dislocation Of The Hip Journal Of Bone & Joint Surgery 47(1).
- Birol Gulman (1994) Md Ismail Cengiz Salter Innominated Osteotomy In: The Treatment Of Congenital Hip Dislocation A Long Term Review Journal Of Orthopedics 14(5): 670-674.
- Rok Vengust Md, Vane Antolic (2001) Franc Srakar Salter Osteotomy For The Treatment Of Acetabular Dysplasia In Delopmental Dysplasia Of The Hip In Patients Under 10 Years. Journal Of Pediatric Orthopedics 10(1).
- Akifusa Wada, Toshio Fujii (2003) Pemberton Osteotomy For Development Dysplasia In Older Children. Journal Of Pediatric Orthopedics 23(4).
- Francois D, Lalonde Stevenl (2002) Frick Surgical Correction Of Residual Hip Dysplasia In Two Pediatric Age Group. The Journal Of Bone And Joint Surgery 84(7).
- Cymet-Ramírez J, Álvarez-Martínez MM (2011) El diagnóstico oportuno de la displasia de cadera.Consenso del Colegio Mexicano de Ortopedia y Traumatología Acta Ortopédica Mexicana 25(5): 313-322.
- Yamamuro T, Hama H, Takeda T (1977) biomechanical and hormonal factors en the etiology ofcongenital dislocation of the hip joint. Internal Orthopedics (SICOT) 1: 231-236.
- Randall T Loder, Elaine N Skopelja (2011) The Epidemiology and Demographics of Hip Dysplasia. International Scholarly Research Network ISRN Orthopedics p. 46-74.
- Salter R (1960) The effects of continues compression on living articular cartilage 42: 20-31.
- Salter RB (1968) Etiology and pathogenesis and possible prevention of congenital dislocation of the hip. Can Med Assoc J 9: 933-945.
- Dunn PM (1992) Perinatal observations on the etiology of congenital dislocation of the hip. Mapfree Medicina 3: 14-23.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...