Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5760
Research Article(ISSN: 2690-5760) 
Evaluate the Effectiveness of Pongamia pinnata Seed Powder on Pityriasis Versicolor (themal) Volume 2 - Issue 3
Shyamala Wijerathne RM1, Piratheepkumar R2 and Paheerathan V3*
- 1Intern Medical Officer, Bandaranaike Memorial Ayurvedic Research Institute, Nawinna
- 2Unit of Siddha Medicine, Trincomalee Campus, Eastern University Sri Lanka
- 3Unit of Siddha Medicine, Trincomalee Campus, Eastern University, Sri Lanka
Received: July 21, 2020 Published: August 27, 2020
Corresponding author: Paheerathan V, Senior Lecturer, Unit of Siddha Medicine, Trincomalee Campus, Eastern University, Sri Lanka
DOI: 10.32474/JCCM.2020.02.000139
Abstract
A single blind comparative clinical study was done in order to evaluate the effectiveness of an external application of ointment which was prepared from seed powder of Pongamia pinnata. Two different concentrations, 5% and 10%, of the drug were prepared. Patients were selected from the outdoor patient division, Rural Siddha Ayurvedic Hospital, Kobalapuram. Thirty patients with bilateral involvement of the lesions were selected for the survey and categorized each to the Test1, Test2, Standard and Control groups respectively, such that 15 lesions were included in each group. Ointment prepared from the seed power of P. pinnata was given to apply twice a day on the selected lesion in the test groups. Observation was done after two weeks and follow up week. At the end of the treatment, P- value for skin pigmentation reduction T1 and T2 were 0.003 and 0.000 respectively indicating that significant improvement was achieved compared to the control group (P-value of 0.104). The P- values for the area size difference of the two groups were 0.001 and 0.001 respectively. It shows the effectiveness of the area reduction of both groups were significant and same. But the P-value for the control group was 0.153 and it implies an increase of the lesion area. So the improvement of the pigmentation reduction of the lesion and reduction of area size can be seen with the external application of the ointment prepared from the seed powder of P. pinnata.
Keywords: Themal, Ptyriasis Versicolor, Pongamia Pinnata
Introduction & Literature Review
This is a single blind comparative clinical study to determine the effectiveness of external application of the Pongamia pinnata seed powder in the management of Themal. The effectiveness of the drug will be assessed with two different concentrations on Themal, and the associated factors such as skin hypo/hyper pigmentation and size that affect the lesion will be ascertained. Fungal skin infections are the most common skin disease condition within Sri Lanka as per the statistics, out of which the majority is Pityriasis versicolor which accounts for a prevalence of 10.5% Perera et al. [1]. Themal is one of the kuttam in Siddha comparable to Pityriasis versicolor in Allopathic Medicine. It occurs on the upper trunk and extends on to the upper arms finally scaling, guttate or nummular patches appear, particularly on young adults who perspire freely Anandhan [2]. In siddha system of medicine many plants are documented for the treatment of skin diseases. Among those the P. pinnata seed has been selected by the researcher for the study. Also there are limited studies done to identify the effectiveness of P. pinnata toward its anti-fungal activity. The P. pinnata is widely used as a traditional medicine commonly known as ‘pungai’ in Tamil. It is a source of biomedicines and used as a crude drug for the treatment of tumours, piles, skin diseases, itches, abscess, painful rheumatic joints wounds, ulcers, and diarrhoea Kumar et al. [3]. According to the Siddha literature, the stanza postulates that the P. pinnata seed has the potency to cure the Themal Murugesamudaliyar [4]. Fungal skin infections are the most common skin disease condition in Sri Lanka as per the statistics, out of which the majority is Tinea vesicolor which accounts for a prevalence of 10.5% Perera et al. [1]. On the other hand, limited studies have been done to identify the effectiveness of P. pinnata toward its anti-fungal activity. Hence, the present study will be an initiative to find out the anti-fungal activity of its seeds such that it could be effectively used for the Tinea versicolor condition.
Review of P. pinnata
Scientific name : Pongamia pinnata (Linn.) Pierre, Syn.
Pongamia glabra Vent.
Plant family : Fabaceae
Tamil name : Pungam-maram
Sanskrit name : karanja
English name : Indian beech
Sinhala name : Karanda [5]
pinnata is a medium sized evergreen or briefly deciduous glabrous tree, 15-25m high, with straight or crooked trunk 50-80 cm or more diameter and broad crown of spreading or drooping branches. The bark is greyish green or brown, smooth or covered with tubercles, leaves compound, imparipinnate, leaflets opposite, 5-9 in number ovate or elliptic. Flowers white tinged with pink or violet, fragrant, in axillary racemes pods are compressed woody, elliptic to obliquely oblong pointed at both ends, Indehiscent, yellowish gray when ripe, varying in size and shape, 4.0-7.5 cm long and 1.7-3.2 cm broad, seeds usually one, rarely two, elliptical or reniform, 1.7-2.0 cm long and 1.2-1.8cm broad, wrinkled with reddish brown leathery testa Warrier et al. [6]
Objective of the study
a. To identify the effectiveness of seed powder of pinnata on Pityriasis versicolor (Themal).
b. To determine the optimum effectiveness of the drug among two different concentrations based on Skin pigmentation reduction, Area size difference of the selected macular lesion, and Age and sex distribution of patients with Pityriasis versicolor, Lesion distribution in the patient’s body.
Methodology
Study Design
This is a single blind comparative clinical study in order to evaluate the effectiveness of seed powder of P. pinnata on Pityriasis versicolor (Themal). Thirty patients were selected for the study by systematic randomization. The patients with bilateral involvement of the lesions were selected and categorized each to the Test 1(T1), Test 2(T2), Standard(S) and Control(C) groups respectively, such that 15 lesions were included in each group. Altogether 60 lesions were selected for the study. This study was conducted after the selection of patients, for a period of one month from 02/03/2019 to 02/04/2019.
Selection of patients
Patients were selected according to the inclusion and exclusion criteria from the outpatient department of the Rural Siddha Ayurveda Hospital, Kobalapuram. The purpose of trial was explained to the patients and got their consent. All the selected patients were interviewed by the researcher in first visit to the OPD.
Plant material
The plant P. pinnata was selected from the quotation of general character of P. pinnata which is mentioned in the text book of Kunapadam (Part 1) Porutpanpu nool written by Murugesa Muthaliyar [4]. The seeds of P. pinnata were collected from the local area of Trincomalee district. The seeds of P. pinnata were authenticated.
Preparation of the medicine
The seeds were collected and it will be cleaned, de-shelled naturally and dried. Then seeds were finely powdered using the grinder. The prepared powder was mixed with the emulsifying ointment and 5% and 10% ointment was prepared.
Methodology
Thirty patients with bilateral involvement of the lesions were selected. The assessment of the disease was done through history taking, general examination and the systemic examination. The prepared ointment of two concentrations 5% and 10% were given to test 1 (T1) and test2 (T2) respectively. It was given to be applied externally twice a day for a period of 2 weeks with a follow up period of 1 week. The ketoconazole cream was given as the standard drug for the standard group (S). The control group (C) was treated with emulsifying ointment. The clinical evaluation of the patients was performed at week 1, week 2 and week 3. In the first day at baseline, a target area was identified and clinical assessment was done in each subject. The evaluation of the skin pigmentation and size of the lesion were done according to the following criteria.
Clinical evaluation
Clinical evaluation visits were made at baseline, week 1, week 2 and week 3. Effect of treatment was evaluated on the basis of the clinical parameters; reduction in the skin pigmentation and affected area size difference were recorded at every visit. Hyperpigmentation/ erythema and hypopigmentation was evaluated by using IGA scale for hyperpigmentation. The affected area of the lesion, the efficacy of the drug, effectiveness of the drug by the skin hypopigmentation, overall effectiveness of the drug was calculated.
Results and Observations
This was a single blind comparative clinical study carried out at Rural Siddha Ayurveda Hospital, Kobalapuram. Thirty patients were selected with hypo-pigmented/ hyper-pigmented and mixed type of macular lesions with normal sensation.
Age and sex distribution
(Table 1) shows the age and sex distribution of the patients with Pityriasis versicolor. Among thirty patients, 63.33% were males and 36.67% were females. The highest number of patients (50%) was between the age group of 20-30, and out of them 33.33% were males while 15% were females. In the age groups 31-40, 41-50 and 51-60, the male sex distribution was 13.33%, 10% and 6.66% while female sex distribution was 10%, 6.66% and 3.33% respectively.
Distribution of Ptyriasis versicolor patients according to the color of lesions
Hypo-pigmented macules were seen in 25 patients (83.3%) followed by either mixed hypo and hyper-pigmented in 2 patients (6.67%) and hyper-pigmented in 3 patients (10%). The results are shown in Table 2.
Distribution of Pityriasis versicolor lesions in the patient’s body
The prominent distribution of lesion on the patient’s body was observed in the neck (38.3%), back (16.8%) and chest (11.7%). Table 3 shows the lesion distribution on the patient’s body.
Variation of skin pigmentation
According to the evaluation criteria, the skin pigmentation of each and every patient in all groups was noted as follows. According to the (Table 4), in 6.7% of the patients almost clear hyperpigmentation was noted in the test group 1 while 20% showed clear hyperpigmentation in the test group 2 (Table 5). According to the table 5-6 table, 26.7% of clear of hyperpigmentation was noted in the standard group and no reduction in hyperpigmentation was recorded in the control group as indicated in (Table 6)
Skin pigmentation variation before and after the treatment in Test 1 group
According to (Table 4), among the 15 lesions of Pityriasis versiolor, 6.7% was noted as almost clear of pigmentation while in 6.7% mild pigmentation was noted. Further 46.6% and 40% were noted as moderate and severe pigmentation respectively (Figures 1.a, 1.b).
Skin pigmentation variation before and after the treatment in Test 2 group
Clear pigmentation was observed in 20 of the lesions while 26.7%, 20% and 33.3% were noted as almost clear, mild and moderate pigmentation respectively (Table 5) (Figures 2.a, 2.b).
Skin pigmentation variation before and after the treatment in Standard group
Clear of pigmentation was noted in 26.7% of the lesions and almost clear, mild and moderate pigmentation were noted in 20%, 46.6%, 6.7% respectively (Table 6).
Skin pigmentation variation before and after the treatment in Control group
Moderate, severe and very severe pigmentation were recorded in 13.3%, 46.7% and 40% respectively of the control group after the treatment (Table 7).
Evaluation of effectiveness of the test drug compared with the control
(Table 5-8) shows the mean values of skin hyperpigmentation before and after treatment of the test group 1(T1) as 4.07 and 3.20 and for test group 2 (T2) as 4.13 and 1.67 respectively while for the standard group (S) the mean was 4.27 and 1.6 before and after the treatment. And for the control group (C) was 4.00 and 4.27 respectively. The P-value for the T1, T2, standard and the control were 0 .003, 0.000,0 .000 and 0.104 respectively.
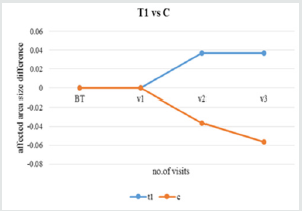
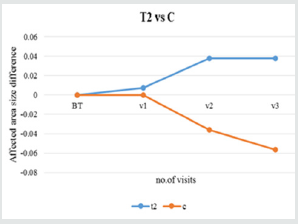
The mean difference of the T1 is 0.867 while in T2 is 2.467. So the skin pigmentation reduction has increased in the T2. The mean difference of the standard group was 2.933. So it shows skin pigmentation reduction was higher compared to T2. The mean difference in the control group is -0.267 and it shows that there is an increase in the pigmentation in the control group. The P-value of T1 is 0.003 and T2 is 0.000 (Figure 3).
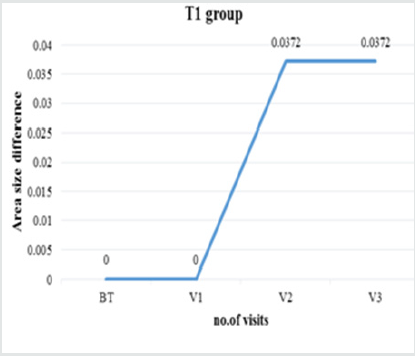
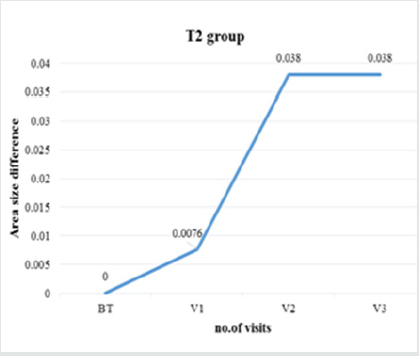
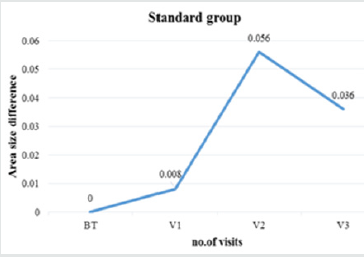
Evaluation of area size difference in each group
Area size difference in test group
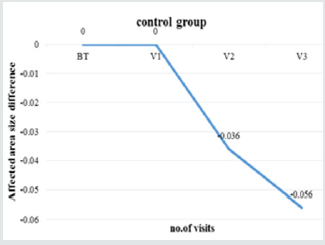
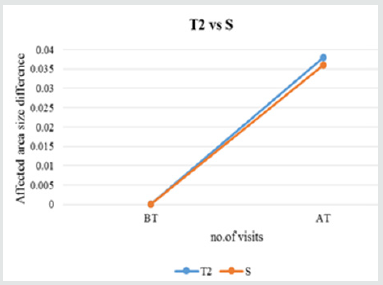
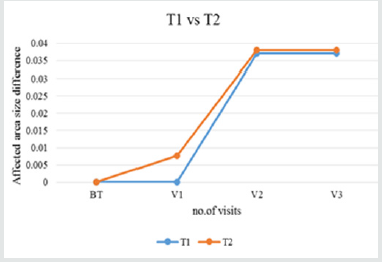
No changes was observed in visit 1 (Figures 4-12) and in visit 2 and visit 3 the mean area size difference was identical (0.0372).
Discussion
Pityriasis (tinea) versicolor is a common disorder that affects people of all age groups, but is most commonly seen in adults. Infants and children can also be affected, but often have an atypical presentation. This disease is typically worse in geographic areas with tropical ambient temperatures. Multiple factors are known to contribute to its pathogenesis Elewski et al. [7]. It is a mild, chronic infection of skin caused by Malassezia yeasts and characterized by discrete confluent, scaly, discolored or de-pigmented areas, mainly on the upper trunk. Colonization by these species is especially dense in the scalp, the upper trunk and flexures, areas rich in sebaceous glands and their secretions. The characteristic changes include hyperkeratosis, parakeratosis, acanthosis and a mild inflammatory infiltrate Pramanik et al. [8].
Yeasts of the Malassezia genus usually start colonization at puberty. Through androgen stimulation, sebaceous glands, peak at this stage and this would explain the higher incidence of Pityriasis versicolor in adolescence and adulthood. This incidence significantly drops at age extremes Framil et al. [9] in the present study; the most common affected group was 20-30 years followed by 31-40 years. Similar findings were given by Kaur et al. [10] (age group 20- 30 years), Shah et al. [11] (age group 21-30 years). There were 19 (63.33%) males and 11 (36.67%) females who were clinically suspected of having pityriasis versicolor which is in agreement with studies by Ghosh et al. [12], Krishnan et al. [13], Rao et al. [14]. This may be due to major involvement of males in outdoor activities with maximum exposure to high temperature and humidity Nazeema et al. [15]. Kaur et al. [10] showed both sexes are equally prone to develop Pityriasis versicolor.
The lesions of the Pityriasis versicolor can be hypo-pigmented, hyper-pigmented, both or erythematous Shah et al. [16]. The type of lesions seen in the study were more of hypo-pigmented followed by hyper-pigmented and mixed types in 83.33%, 10% and 6.67% respectively, which correlated with the findings made by Shah et al. [16] ( hypo-pigmented (84.17%), hyper-pigmented (8.63%), mixed (7.19%), Krishnan et al. [13] (Hypo-pigmented (84%), hyperpigmented (9%), mixed (6%)), Kabbin et al. [17] (hypo-pigmented (67%), hyper-pigmented (31%), mixed (2%), while Rao et al. [14] observed mixed variety in 16.6%, hyper-pigmented in 8.30%. This variation in the morphological appearance of lesions may be due to differences in climatic conditions and different study population.
The most common involvement was neck, back and chest followed by arm and axilla. Similar findings are also noted by Dutta et al. [18], Rao et al. [14] and Tarazooie et al. [19] with chest, back and neck as most commonly involved sites. The distribution of lesions coincides with the density of sebaceous glands distribution with highest occurrence on chest and back Nazeema et al. [15].
P. pinnata is a medicinal plant used for treating many diseases. According to Murugesa Mudaliyar, the seeds of P. pinnata can be used in the management of Pityriasis versicolor. It possesses Karangin which has the antiseptic and insecticide properties. So it can be used for the skin conditions such as chronic eczema, psoriasis, scabies, ringworm and pityriasis Jayaweera [5]. In the present study, change of skin pigmentation was observed in the two different concentrations of the test drug. According to the (table 4), almost clear pigmentation was observed in 6.7% of the patients in the test group 1 (T1) and 20% clear pigmentation in the test group 2 (T2) (Table 5). Clear pigmentation in 26.7% and 20% almost clear pigmentation in standard group (S) was observed (Table 6). There was no pigmentation reduction in the control group while increase density of the pigmentation was noted (Table 7). The P-value for pigmentation variation of the test group 1 was 0.003 and it was 0.000 for the test group 2 and standard group while P-value of the control group was 0.104. It showed that the pigmentation reduction in both test groups was significant and it is highly significant in the test group 2. The T2 and S group’s P value are same and it shows similar reduction. But in the control group instead of the reduction, there was an increase of the skin pigmentation during the treatment period.
The mean values of the affected area size difference of the test group 1 and test group 2 increased (Table 9). Hence the reduction of pigmentation has increased along with the area size reduction. A negative mean value of the area reduction of control group implies that the affected area size is getting increased (Table 9). The P-values for the test1, test 2, standard and control are 0.001, 0.001, 0.000 and 0.153. So the area size reduction of the two test groups is similar and more effect on standard while increase of the size of the lesion was present in the control group.
According to the siddha text by Kuppusami Muthliyar [20] the Kapha become prominent in the pundareeka kuttam. Additionally it is also mentioned in Kanthasami Muthaliyar [21] that at the severe stage of the disease condition the body becomes oedematous. The seed of P. pinnata posseses the suvai (taste) astringent and bitter, viriyum (potency) hot and vipakam (output) pungent. The panchaboothic composition of Kapha dosha is Earth and water and that of astringent and bitter taste is, air + earth and air + space respectively. Hence, the seed part of the P.pinnta can be used in the management of Pityriasis versicolor (themal) by balancing the vitiated Kapha dosha. The (Table 9) shows the effectiveness of the drug before and after the treatment which was calculated based on the skin pigmentation reduction and area size difference. Based on the skin pigmentation, effectiveness can be shown as from the total patients in the group how many patients has reduced the pigmentation. So it is 6.66 % in T1 and 20% in T2. Based on affected area size difference, drug effectiveness can be taken as how much of the pigmentation was reduced by comparing the mean values before and after the treatment. . So it is 22.4 % in T1 and 27.5% in T2. According to the (Table 1) mild to moderate effectiveness of action of the drug could be seen. The overall effectiveness of the drug is good [22-45].
Table 9: Drug effectiveness. (BT- Before Treatment, AT- After Treatment, M- Mean, DE-Drug Effectiveness, SPR- Skin Pigmentation Reduction, ASD- Affected Size Difference.

Conclusion
Drug effectiveness based on skin pigmentation reduction in T1 is 6.7% and T2 is 20%. Effectiveness based on area size difference of T1 is 22.4% and T2 is 27.5%. Therefore the overall effectiveness of the drug is good. And 10% ointment is better than the 5% ointment in the skin pigmentation reduction and area size difference of the lesion. Hence the seed powder of P. pinnata shows effectiveness on Pityriasis versicolor.
References
- Perera A, Atukorale DN, Sivayogan S, Ariyaratne VS, Karunaratne L A, et al. (2000) prevalence of skin diseases in suburban srilanka. Ceylon Med journal 45(3): 123-128.
- Anandan AR (2009) Special medicine in Siddha. First edition. Department of Indian Medicine and Homeopathy, Chennai, India pp. 240.
- Kumar RSAS, Rajeswari R, Selvakumar M, Karthikraja N, Hariharan N, et al. (2016) study of Pongamia pinnata flower and seed extracts for their antioxidant and antibacterial activity. INDO American Journal of Pharmaceutical Research 6(10): 6618-6621.
- Murugesamudaliyar KS (2013) Siddha Materia Medica (Medicinal Plants Division). 9th Indian Maruthuvam Homeopathy 106: 691-693.
- Jayaweera DMA (2006) Medicinal Plants (Indigenous and Exotic) used in Ceylon. Part III. Colombo: M.D.Gunasena & Co. (Printers) Ltd 228-229.
- Warrier PK, Nambiar VPK, Ramankutty C (1995) Indian Medicinal Plants: A Compendium of 500 species. Hyderabad: Orient Longman Private Limited 4: 339-344.
- Elewski BE, Chairman Elgart ML, Jacobs PH, Lesher JL, Scher RK (1993) Guidelines of care for superficial mycotic infections of the skin: Pityriasis (tinea) versicolor.
- Pramanik SB, Bandopadhyay M, Nandi A, Maitrayee B, Rina G, et al. (2014) A Study of Prevalence of Different Species of Malassezia Causing pityriasis versicolor and Sites of distribution of lesion in a tertiary Care Hospital in kolkata, India. IJCMAG 4(3): 471-478.
- Framil VMS, Melhem MSC, Szeszs MW, Zaitz C (2011) New aspects in the clinical course of pityriasis versicolor 86(6): 1135-1140.
- Kaur M, Narang T, Bala M, Gupte S, Aggarwal P, et al. (2013) Study of distribution of malassezia species in pityriasis versicolor and healthy individuals in tertiary care hospital, Punjab.
Indian J Med Microbiol 31(3): 270-274. - Kazemi A, Mousavi SAA, Jafari AA, Mahmoudabadi AZ, Alikhah H (2013) Study on Pityriasis versicolor in patients referred to Clinics in Tabriz. Jundishapur J Microbiol 6(8): e7211.
- Ghosh SK, Dey SK, Saha I, Barbhuiya JN, Ghosh A, et al. (2008) Pityriasis versicolor:a clinicomycological and epidemiological study from a tertiary care hospital. India J Dermatol 53(4): 182-185.
- Krishnan A ,Thapa DM (2003) Morphological and pigmentary variations of tinea versicolor in South Indian patients. Indian Journal of Dermatology 48(2)
- Rao GS, Kuruvilla M, Kumar P, Vinod V (2002) Clinicoepidemiological studies on tinea versicolor. Indian J Dermatol Venereol Leprol 68(4): 208-209.
- Nazeema T, Nischal K, Swaroop MR (2014) Clinico-epidemiological study of pityriasis versicolor in a rural tertiary care hospital. IJRMS 2(4): 1438-1440.
- Shah A, koticha A, Ubale M, Wanjare S, Mehta P, et al. (2013) Identification and speciation of Malassezia in patients clinically suspected of having pityriasis versicolor. Indian j Dematol 58(3): pp. 239.
- Kabbin JS, Vijaya D, Meundi MD, Leelavathy B (2011) Clinicomycological Study of Pityriasis versicolor with a special reference to the Calco flour White. Journal of Clinical and Diagnostic Research 5(7): 1356-1358.
- Dutta S, Bajaj AK, Basu S, Dikshit A (2002) Pityriasis versicolor: Socioeconomic and clinico-mycologic study in India. Int J Dematol 41(11): 823-824.
- Tarazooie B, Kordbacheh P, Zaini F, Zomorodian K, Saadat F, et al. (2004) Study of the distribution of Malassezia species in patients with pityriasis versicolor and healthy individuals in Tehran, Iran. BMC Dermatol 4: 5.
- Kuppusami muthliyar KN (2016) Siddha Maruthuvam (pothu), 8th edition, India Maruthuvam Homeopathy thurai 686 -687.
- Kanthasamy Mudaliyar K (2012) Pathinen Siththar Arulich Seitha Nadi Saththiram. B. Rathnayaka & sons Chennai, India 6.
- M Elanchezhiyan, S Rajarajan, P Rajendran, S Subramanian, S P Thyagarajan et al. (1993) Antiviral properties of the seed extract of an Indian medicinal plant, Pongamia pinnata, Linn., against herpes simplex viruses: In-vitro studies on Vero cells. J Med Microbiol 38(4): 262-264.
- Bannister B, Gillespie S, Jones J (2006) Infection Microbiology & Management. Third edition. Blackwell publishing Ltd., Carlton pp.113.
- Greenwood D, Slack RCB, Michael Barer Will Irving, (2012) Medical Microbiology. 16th (eds). Elsevier Germany pp.794.
- Gupta AK, Foley KA (2015) Antifungal treatment of Pityriasis versicolor. Journal Fungi (Basel) 1(1): 13-29.
- Inala MSR, Dayanand CD, Sivaraj N, Beena PM, Kutty AUM, et al. (2015) Antibacterial activity of Flavonoids Extracted from seeds of Pongamia pinnata Linn on Methicillin Resistant Staphylococcus aureus. British Microbiology Research 10(1): 1-8.
- Krishnamoorthy JR (2004) Siddha Maruthuvam Cirappiyal. First edition. Chennai: Tamil Valarchi kazhagam 162-163.
- Lunawat SR, Sabu NR (2016) Ayurvedic Approach in Fungal Infections of skin. World Journal of PHARAMACEUTICAL Research 5(4): 1757-1762.
- Meera G, Thilak S, Joshua J (2016) A study of 200 cases of pityriasis versicolor: The distribution of age, gender, blood group, lesion morphology, haemoglobin levels, cholesterol levels and diabetic status. Internatinal Jounal of Research in Dermatology 3(1): 20-23.
- Meera G, Thilak S, Joshua J (2017) A study of 200 cases of Pityriasis versicolor: The distribution of age, gender, blood group, lesion morphology, haemoglobin levels, cholesterol levels and diabetic status. Internatinal Jounal of Research in Dermatology 3(1): 20-23.
- Mohomoud YAG, Metwally MA, Mubarak HH, Zewawy NE (2014) Treatment of Tinea Versicolor caused by Malassezia furfur with Dill seed Extract: An experimental study. Int J Pharma Sci 7(2): 1-7.
- National Institude of Science Communication and Information Resources (2008) Siddha Pharmacopoeia of India. First edition. Government of India, New Delhi, India 1(1): 150-151.
- Oakley A(2003) What is Pityriasis Versicolor. Dermnet, Newzeland.
- Oakley A (2014) What is Pityriasis Versicolor. Dermnet, Newzeland.
- Paniker CKJ (2005) Ananthanarayan & Paniker’s Textbook of Microbiology. 7th Universities Press (India) Private Limited, India pp. 612.
- Pooja A, Arun N, Maninder K (2013) Screening of plant essential oils for Antifungal Activity against Malassezia furfur. International Journal of pharmacy and pharmaceutical sciences 5(2): 37-39.
- Rahman MS, Islam MB, Rouf MA, Jalil MA, Haque MZ, et al. (2011) Extraction of Alkaloids and oil from Karanja (Pongamia pinnata) seed. journal of scientific Research 3(3): 669-675.
- Reena Singh, RAM, Sinha BK (2012) Evaluation Of Pongamia pinnata seed extracts as an insecticide against American Bolloworm Helicoverpa armigera (HUBNER). International Journal of Argiculture Sciences 4(6): 257-261.
- Sambasivam Pillai TV (1936) Siddha Medical Dictionary. Part 2 2(eds) Sivakasi 2: 1344-1345.
- Sharma PC, Yelne MB, Dennis, T.J. (2005) Database on Medicinal Plants used-297. in Ayurveda. Pearl offset Press Pvt.Ltd., India 2: 292
- Sharma R, Chandra S, Singh, A (2012) Essential oils against Lipophilic Yeast like fungus. IJPBA 3(1): 63-68.
- Sharma Y, Jain S, Chandra K, Munegowda KC (2017) A Clinico-epidemiologic evaluation of pityriasis versicolor from a government hospital,India: Conventional methods- still a thumbs up?. Indian Journal of MedicalSciences 69(1): 40-43.
- Thiyagarajan R (2008) Siddha Maruthuvam Sirappu. Third edition. Chennai – 600 106: Commissionerate of Indian medicine & Homoeopathy, Arumbakkam pp. 197-199.
- Weerasekara S, Weerasekara KR(2014) Evaluate the efficacy of freshly prepared juice of “Cassia alata L.” leaves in the management of Sidma Kushta – A preliminary study. International Journal of Herbal Medicine 2(3): 37-88.
- Yadava RN, Archana C (2014) Chemical Examination of the seeds of Pongamia pinnata (L.) Pierre. International Journal of Pharmacognosy and Phytochemical Research 6(2): 282-283.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...