Use Of Surveillance, Epidemiology, And End Results
(SEER)-Medicare Data to Characterize the Demographics,
Disease Characteristics, Comorbidities, And Survival
of Elderly (≥65 Years) Patients with Human Epidermal
Growth Factor Receptor-2-Positive Breast Cancer as
Primary Cancer in the United States
Volume 4 - Issue 5
Nora Tu1*, Zahidul Islam1, Mackenzie Henderson1,2 and Maribel Salas1,3
- 1Global Epidemiology Department, Daiichi Sankyo, USA
- 2Rutgers Institute for Pharmaceutical Industry Fellowships, Rutgers University, USA
- 3Center for Clinical Epidemiology and Biostatistics (CCEB)/Center for Pharmacoepidemiology Research and Training (CPeRT), University
of Pennsylvania Perelman School of Medicine, USA
Received:August 5, 2021 Published: August 19, 2021
Corresponding author: Nora Tu, Global Epidemiology Department, Daiichi Sankyo, 211 Mount Airy Road, Basking Ridge, NJ, USA
DOI: 10.32474/OAJOM.2021.04.000198
 Fulltext
Fulltext
 PDF
PDF
To view the Full Article Peer-reviewed Article PDF
Abstract
Purpose: A retrospective cohort analysis to investigate comorbidities and 5-year survival in elderly patients (≥65 years)
with human epidermal growth factor receptor-2-positive (HER2-positive) breast cancer (BC) using data from the Surveillance,
Epidemiology, and End Results (SEER)-Medicare program
Methods: Female patients aged ≥65 years with a HER2-positive BC diagnosis as the first cancer diagnosis (between 1/1/2010–
12/31/2015) were eligible. Comorbidities and 5-year survival of HER2-positive BC patients (irrespective of stage) were compared
with age/race-matched non-cancer controls. Survival data (time-to-death) were unadjusted and adjusted by comorbidities and
region.
Results: Data from 8978 HER2-positive BC patients and 8978 controls were included. Mean age was 77.1 years (range: 66.0–
102.8 years). Most cancers were Stage I (35.1%) or II (33.2%) at diagnosis. Thirteen/24 predefined comorbidities were significantly
more prevalent in HER2-positive BC patients versus controls (P < 0.05). The most prevalent comorbidities in HER2-positive BC
patients were anemia, hypertension, and arthritis. Generally, comorbidities were more likely to be diagnosed before HER2-positive
BC diagnosis. The estimated probability of 5-year survival was 69.7% (95% CI: 68.6%, 70.7%) for BC patients compared to 82.4%
(95% CI: 81.5%, 83.3%) for controls. The risk of dying was higher among HER2-positive BC patients compared to non-cancer
controls, with an unadjusted hazard ratio (HR) of 1.843 (95% CI 1.734,1.960) and adjusted HR of 1.934 (95% CI 1.819,2.057).
Conclusions: Many comorbidities were more prevalent in elderly patients with HER2-positive BC compared with controls,
though few were more prevalent in controls. Comorbidities were generally more likely to be diagnosed prior to HER2-positive
BC diagnosis. Mortality risk in patients with HER2-positive BC was higher than controls even after adjusting by comorbidities,
suggesting that other factors are involved in the survival of elderly patients with HER2-positive BC. The clinical relevance of
comorbidities in HER2+ BC patients and controls requires further study.
Keywords: Comorbidity; Elderly; HER2-positive breast cancer; SEER-Medicare; Survival
Abbreviations: 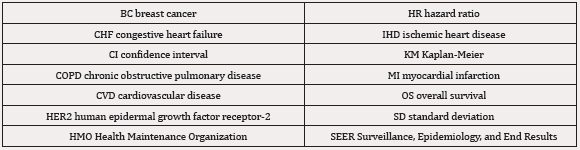
Abstract|
Introduction|
Materials and Methods|
Statistical analysis|
Results|
Discussion|
Conclusion|
Data Availability|
Compliance with Ethical Standards|
Ethical approval|
Informed Consent:|
Acknowledgements|
References|
