
Lupine Publishers Group
Lupine Publishers
Menu
Mini Review(ISSN: 2641-6875) 
Review of Bone Scan in Staging of Breast Cancer Patients (Milton Keynes University Teaching Hospital NHS Trust 2020-2021) Volume 2 - Issue 4
Olawunmi Olayiwola1*, Taiwo O. Aremu2,3,4, Oluwafemi A Ajibola5, Oluwatosin E Oluwole6 and Kehinde O Adeyinka7
- 1Department of Medicine, Milton Keynes University Hospital, UK
- 2Masonic Cancer Center, University of Minnesota Masonic Children’s Hospital 420 Delaware St. SE - Mayo MMC 484, USA
- 3Department of Pharmaceutical Care & Health Systems (PCHS), College of Pharmacy, University of Minnesota, USA
- 4Division of Environmental Health Sciences, School of Public Health, University of Minnesota, USA
- 5Department of Medicine, Nuvance Health, Vassar Brothers Medical Center, USA
- 6Division of Epidemiology & Community Health, School of Public Health, University of Minnesota, USA
- 7Department of Radiation Oncology, University College Hospital (UCH), Nigeria
Received:December 03, 2021; Published:December 09, 2021
*Corresponding author: Olawunmi Olayiwola, Department of Medicine, Milton Keynes University Hospital, UK
DOI: 10.32474/CTBM.2021.02.000144
Abstract
We conducted a review of the Milton Keynes University Teaching Hospital NHS Trust’s modality of staging breast cancer to assess compliance with the Royal College of Radiology (RCR) guidelines in the use of bone scan for breast cancer staging. We noticed that a bone scan was required for all breast cancer patients, most of whom did not meet the RCR criteria for a bone scan. We found that a bone scan done on all 89 breast cancer patients seen from June 2020 to May 2021 was ineffective in confirming all cases with bone metastasis, hence not contributing to management and outcomes. We recommend that bone scans should not be routinely done on breast cancer patients, as it is not cost-effective and cost-saving.
Keywords: Breast Cancer; Bone Scan; Whole Body Staging; CT scan; Bone Metastasis
Abbreviations: CT: Computerized Tomography; MRI: Magnetic Resonance Imaging; RCR: Royal College of Radiology; T3: Tumour >4cm but not extending beyond the thyroid gland; T4: Tumour of any size extending beyond the thyroid gland; N1: metastasis to 1 - 3 axillary lymph node or the internal mammary lymph nodes; NHS: National Health Service; USS: Ultrasonography; PET: Positron emission tomography; GBP: British pound sterling
Introduction
Breast cancer is the most common cancer in the United Kingdom (UK), with about 56,000 new cases every year and about 150 cases every day [1]. The risk of developing breast cancer is more in women, with an estimated lifetime risk of 1 in 7 women born after 1960 and living in the UK [1]. Approximately 11,500 women and 85 men die of breast cancer every year in the UK, making it the fourth most common cause of death in the UK and the second most common cause of death in women [1]. Early diagnosis is essential to improving the already high survival rates. Although positive family history is a non-modifiable risk factor for breast cancers, lifestyle modification can help prevent it or slow down its occurrence. The need to adequately stage and identify the extent of distant metastasis from breast cancer is essential to improving patients’ quality of life. Some of the radio-diagnostic measures used for staging breast cancers include Computerized Tomography (CT) scan, Magnetic Resonance Imaging (MRI), Bone scintigraphy (bone scan), etc. A bone scan can also be referred to as nuclear medicine bone scan or radionuclide scan. The presence of distant metastasis at presentation occurs in about 4 - 6% of patients; as a result, whole-body staging is not required in the vast majority of cases [2]. According to the Royal College of Radiology (RCR) guidelines, the criteria for whole body staging in patients with breast cancer include T3 and T4 primary cancers, greater or equal to four abnormal nodes at axillary ultrasonography (USS) or greater or equal to four macro metastatic nodes at axillary surgery, and if symptoms raise the suspicion of metastatic disease [2]. At present, there is no evidence for carrying out staging prior to neoadjuvant chemotherapy in patients with T2 or less tumors with N1 or less disease [3]. The contrast-enhanced CT of the chest, abdomen, and pelvis, incorporating the supraclavicular fossae and proximal femora, is the modality of choice in most cases. The bone scintigraphy is not routinely indicated in addition to CT scan in the absence of bone symptoms. This review aims to identify the current level of compliance of the Milton Keynes University Teaching Hospital National Health Service (NHS) Trust with the RCR guideline in the use of bone scan for breast cancer staging and make appropriate recommendations for improving patient selection for a bone scan in breast cancer staging.
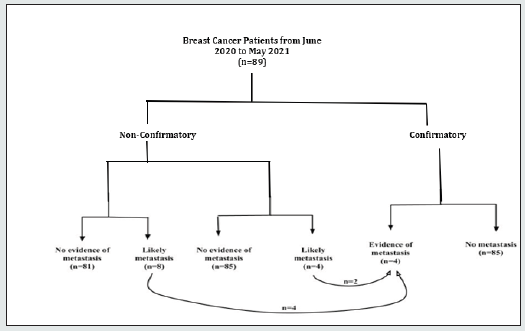
Review Outcome
In the Milton Keynes University Teaching Hospital NHS Trust (referred to as the Trust), a bone scan and CT scan are requested for all breast cancer staging. CT scans are also done for patients before commencing neoadjuvant chemotherapy. A sample size of 89 included all patients who had a staging CT scan between June 2020 to May 2021. Signs of likely metastasis were seen in 8 (9%) of the 89 patients on CT scan, with no evidence of metastasis in 81 (91%) cases. The 89 patients equally had a bone scan, a form of nuclear medicine, with 4 (4.5%) of the 89 patients showing signs of likely bone metastasis. Of all the 89 patients, only 4 were eventually confirmed to have bone metastasis, and this was confirmed by either MRI or a positron emission tomography (PET) scan. It is worthy of note that all 4 confirmed cases were among the 8 patients initially detected by CT to have likely bone metastasis, while only 2 of these confirmed bone metastasis patients were picked up by a bone scan (Figure 1). This translates to the fact that the bone scan had a 50% failure rate in detecting bone metastasis, as it failed to pick up 2 patients that were eventually confirmed to have bone metastasis.
Figure 1: Distribution of patients in the staging of breast cancer at the Trust from June 2020 to May 2021.
Discussion:
Bone scans are not routinely indicated in addition to CT scans in the absence of bone symptoms [4]. However, a bone scan was requested alongside a CT scan for all patients at the Trust, despite not meeting the RCR criteria for a bone scan. Findings from the review showed that bone scan did not add to the staging of these patients and was not needed at all by the other 87 patients as only two benefited from it. It has only contributed to prolonging the commencement of treatment and added to the already long list of care and follow-up appointments these patients already have. Besides, because not all centres have the facilities to provide a bone scan, patients have had to travel to other hospitals to have this investigation done. The routine use of bone scans to determine the presence of bone metastasis in breast cancer patients has health implications, including poor outcomes from a false negative result where treatments may have been delayed and the psychological stress of visiting distant hospitals for a timely schedule of the investigation. The economic implication is significant, with a national average (median) cost of 103 GBP per bone scan [5].
Conclusion
Our findings suggest that bone scan’s use in the staging of breast cancer patients does not improve their management modality. Therefore, we recommend that a bone scan should not be routinely required to determine bone metastasis in breast cancer patients. Also, we recommend following the RCR guideline that discourages the routine use of bone scintigraphy in addition to CT in the absence of bone symptoms to the staging of breast cancer. These may help save cost, reduce possible delays in commencing the proper treatment, and reduce the stress of partaking in a less cost-effective procedure. Finally, we do recommend that more observational studies be carried out to elicit our findings further.
Ethics Approval:
The audit was logged with the institution (Audit number: 844)
Consent for Publication
Not applicable
Availability Of Data and Materials
Not applicable
Competing Interests:
The authors declare that they have no competing interests.
Funding
No funding reported.
Authors Contributions
Conceptualization, O.O.; methodology, O.O., T.O.A., and O.A.A.; writing-original draft preparation, O.O.; writing—review and editing, O.O., T.O.A., O.A.A., O.E.O., and K.O.A. All authors have read and agreed to the published version of the manuscript.
Acknowledgment
We acknowledge Dr. Sheeba Taneja, MBBS, MD (Radiology), MSc, FRCR, and Dr. Oluwaseun E Olayiwola, MBBS, MRCGP, DRCOG, for their guidance and technical support.
References
- (2021) UK Breast Cancer Statistics. Breast Cancer UK.
- (2021) Guidance on screening and symptomatic breast imaging, Fourth edition | The Royal College of Radiologists.
- Roszkowski N, Lam SS, Copson E, Cutress RI, Oeppen R (2021) Expanded criteria for pretreatment staging CT in breast cancer. BJS Open 5(2):
- Bansal GJ, Vinayan Changaradil D (2018) Planar Bone Scan Versus Computerized Tomography in Staging Locally Advanced Breast Cancer in Asymptomatic Patients: Does Bone Scan Change Patient Management Over Computerized Tomography? Journal of computer assisted tomography 42(1): 19-24.
- (2021) How much does a private dexa bone scan cost in the UK? | Private Healthcare UK.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





