Lupine Publishers Group
Lupine Publishers
Menu
Review Article(ISSN: 2641-6875) 
FGFR Gene Mutation and Pfeiffer Syndrome Volume 2 - Issue 5
Walaa Fikry Elbossaty*
- Department of Biochemistry, Damietta University, Egypt
Received: June 23, 2022; Published: July 08, 2022
*Corresponding author: Walaa Fikry Elbossaty, Department of Biochemistry, Damietta University, Egypt
DOI: 10.32474/CTBM.2022.02.000150
Abstract
Pfeiffer syndrome is a genetic disease caused by a defect in the FGFR-1 or FGFR-2 genes. This syndrome affects the skeleton, whether it is a protrusion of the skull bone or problems in the limbs. Not only this, but also affects the eyes, leading to their protrusion, in addition to the possibility of hydrocephalus, and internal viscera imbalance. There are 3 types of the syndrome classified according to the clinical examination of the case, where the symptoms range from mild to severe, which requires surgical intervention. It is easy to diagnose the fetus early through ultrasound examination, which shows ossification in the bones of the skull and deformities of the fingers. The incidence of Pfeiffer syndrome is limited, as it affects one child in 100,000 cases. Genetic testing facilitates early diagnosis and thus helps in rapid treatment and prevention of deterioration of the condition.
Keywords: Pfeiffer Syndrome; Genetic Mutation; FGFR-1; FGFR-2; Craniosynostosis
Introduction
Pfeiffer syndrome is a rare genetic disorder characterized by premature fusion of the bones of the skull, which causes Craniosynostosis. There are also changes in the shape of the fingers and toes, especially the thumb, where curves and length of these limbs are observed compared to normal people. In addition, in some cases, protrusion of the eyes occurs with Hearing loss.it occur in 1 per 100.000 newborn in world [1] (Figure 1).
Causes
The main cause of this disease is considered to be a genetic defect in fibroblast growth factor receptor-1 (FGFR1) at chromosome 8p11.22-p12 and fibroblast growth factor receptor-2 (FGFR2) at chromosome 10q25-q26 [2]. Pfeiffer syndrome is a series of genetic disorders caused by mutations in the FGFR1 and FGFR2 genes [3]. The genetic mutation may be a result of injury to one of the parents or the result of genetic changes in the patient as a result of a genetic mutation [4].
It was noted that the main cause of cases of Pfeiffer syndrome type II and type III is the occurrence of recent genetic mutations. It was also noted that the advanced age of the parents may be the cause of these recent genetic mutations [5]. Scientific research has proven that the probability of infection with Pfeiffer syndrome may reach 50% in the case if one of the parents is a carrier of genetic mutations. It was also found that the main cause in Pfeiffer syndrome type I is the occurrence of genetic mutations in FGFR1, while the main cause in both Pfeiffer syndrome type II and type III is the occurrence of genetic mutations in FGFR2 [6]. The prevalence of this phenomenon occurs for each case out of 100,000 cases on average [7].
Symptoms
Pfeiffer syndrome is a complex genetic disorder that affects a child’s head, face, hands and feet, where the severity of symptoms ranges from mild to severe. The most important symptoms are [1]:
Craniosynostosis
In which early closure of the skull occurs without complete brain development and appear hydrocephalus, as it is normal for the skull to close during the first few months, but in these children, the skull is closed before that and often in the first weeks of birth, and this causes the skull to lengthen, which affects the normal shape of the brain [8] (Figure 2).
Midfacial hypoplasia
This causes the presence of sunken places in the face, which may affect the airway, causing sleep apnea [9].
Proptosis:
It has wide, unprotected eyes. In addition to other different symptom according to the stage of patients, these symptoms may be included:
a) Short in limbs and enlargement of toe
b) high forehead
c) beaked nose
d) underdevelopment or overdevelopment of the jaws
e) dental problems
f) hearing loss (Figure 3).
g) problems with brain development and other neurological deficits in types 2 and 3
h) developmental delays in types 2 and 3
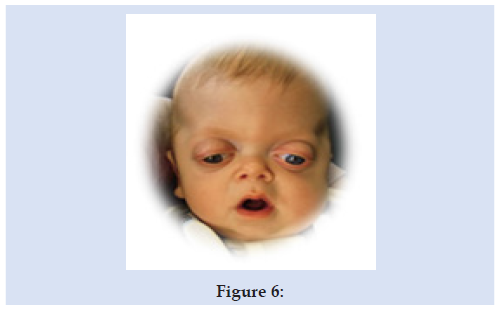
Types of Pfeiffer Syndrome
There are 3 types of Pfeiffer syndrome, with type 1 being the mildest in terms of symptoms, but type 2 and 3 being the most harmful and dangerous [1]. We find that children suffering from Pfeiffer syndrome type I have Craniosynostosis, which makes the bones, looked longer and shorter. In addition to facial dysplasia and the separation of the eyes and protrusion in them, the upper jaw is usually incomplete and the teeth are deformed [10]. As for Pfeiffer syndrome type II, it is characterized by a larger protrusion in the Cloverleaf skull and deformities in the extremities of the hands and feet, and the early closure of the bones of the skull usually leads to the appearance of a three-lobed shape in the skull (Figures 4-6). In addition to severe protrusion of the eyes, hypoplasia of the middle of the face, a nose in the form of a beak the ears of the displaced, in addition to deformities in the joints, deformities in some internal organs such as the abdomen, and this type is often accompanied by lack of oxygen and poor mental development, and if the case was not subjected to early treatment, this led to death. We also find that individuals with type 3 Pfeiffer syndrome have the same symptoms as those with type 2 except for skull cloverleaf deformity. These are characterized by a short skull size, exophthalmos in the eyes, the appearance of some teeth during childbirth, visceral abnormalities in the abdomen, and neurological problems that may threaten life if treatment is not done early [11].
Diagnosis
Diagnosis depends on the clinical examination through the size of the head, the shape of the skull, and length of the limbs, especially the thumb, the shape of the eyes and jaw, and the confirmation of the sense of hearing. In addition to X-rays or CT scan, to check the skull [12]. In the event that there is not enough clinical information to diagnose and classify the condition, genetic analyzes for FGFR1 and FGFR2 are used, using the polymerase chain reaction technique [13].
Treatment
The treatment strategy, of course, varies according to the case of individuals, but the treatment process requires a consultation of doctors in many specialties, including pediatrics, audiologists, surgery specialists, and ear and nose specialists. There are many stages of treatment according to the condition of the child, including:
First Treatment
One of the most important problems that affected children face is difficulty breathing, which may be accompanied by interruption of breathing, the possibility of the child going blind. Therefore, one of the first steps of treatment is a sleep study to see if the breath stops during sleep. This is in addition to the necessity of measuring the percentage of oxygen saturation to ensure that the amount of oxygen is sufficient for brain growth [14].
Brain Surgery
It is usually preferable to do it after 6 months, especially after 15 months, and they are usually given erythropoietin to adjust blood levels. Treatment strategies can be summarized in to the following points:
a. Surgery to release blockages of the mid-face.
b. Surgery to remove tonsils or adenoids (glands located in the roof of the mouth that protect against infection).
c. Continuous positive airway pressure (CPAP) therapy involving the use of a special mask while sleeping.
d. A tracheostomy is carried out in severe cases. A tracheostomy is a surgical opening through the front of the neck and into the trachea (windpipe).
Some cases may require surgical intervention, as the early sutures in the skull lead to high pressure inside the skull, which leads to leaks from the spinal cord, which causes hydrocephalus that requires inserting a tube to withdraw the CSF fluid and divert it away from the brain [15]. Some cases also require corrections in the deformities that may occur in the face and jaw. In addition to correcting the deformities that may occur in the extremities and ears and lead to deafness [16]. The faster the surgical intervention, the sooner we reach the desired goal in controlling this phenomenon and preserving the life of the child. Therefore, it is necessary to clinical examination of the parents to quickly discover the possibility of the emergence of genetic mutations that may cause the occurrence of these diseases in children [17].
Disclosure Statement
The authors have no conflict of interest.
References
- M Das J, Winters R (2022) Pfeiffer Syndrome. Stat Pearls Treasure Island (FL).
- Min Y, Ga W, Ji M, Beom S (2010) A case of Pfeiffer syndrome with c833_834GC>TG (Cys278Leu) mutation in the FGFR2 gene. Korean Journal of Pediatrics 53(7): 774-777.
- Yue S, Li Y, Chen X (2021) FGFR-TKI resistance in cancer: current status and perspectives. J Hematol Oncol 14(1).
- Jackson M, Marks L, May GHW, Wilson JB (2018) the genetic basis of disease. Essays Biochem 62(5): 643-723.
- Glaser RL, Jiang W, Boyadjiev SA, Tran AK, Zachary AA, Van Maldergem L, et al. (2000) Paternal origin of FGFR2 mutations in sporadic cases of Crouzon syndrome and Pfeiffer syndrome. Am J Hum Genet 66: 768-777.
- Torres-Canchala L , Castaño D, Silva N, Gómez AM , Victoria A , Pachajoa H (2020) Prenatal Diagnosis of Pfeiffer Syndrome Patient with FGFR2 C.940-1G>C Variant: A Case Report (13): 147-150.
- Das S, Dasari, A (2021) Epidemiology, Incidence, and Prevalence of Neuroendocrine Neoplasms: Are There Global Differences? Current oncology reports 23(4): 43.
- Lipsett BJ, Reddy V, Steanson K, Anatomy, Head, et al. (2021) Stat Pearls. Treasure Island (FL).
- Cielo CM, Marcus CL (2015) Obstructive sleep apnoea in children with craniofacial syndromes. Paediatr Respir Rev 16(3): 189-196.
- Wenger T, Miller D, Evans K (2020) FGFR Craniosynostosis Syndromes Overview.
- Luo E, Liu H, Zhao Q (2019) Dental-craniofacial manifestation and treatment of rare diseases. Int J Oral Sci 11: 9.
- Erly WK, Berger WG, Krupinski E, Seeger JF, Guisto JA (2002) Radiology resident evaluation of head CT scan orders in the emergency department. AJNR Am J Neuroradiol 23(1): 103-107.
- Qin J, Xie F, Wang F, Lu H (2020) mRNA Expression of FGFR1 as Potential Marker for Predicting Prognosis of Surgical Resection of Small Cell Lung Cancer may be better than Protein Expression and Gene Amplification. J Cancer 11(16): 4691-4699.
- Krook MA, Reeser JW, Ernst G (2021) Fibroblast growth factor receptors in cancer: genetic alterations, diagnostics, therapeutic targets and mechanisms of resistance. Br J Cancer 124: 880-892.
- Telano LN, Baker S (2021) Physiology, Cerebral Spinal Fluid. Stat Pearls. Treasure Island (FL).
- Farb R, Rovira À (2020) Hydrocephalus and CSF Disorders. Hodler J, Kubik-Huch RA, von Schulthess GK (Eds.), Diseases of the Brain, Head and Neck, Spine 2020-2023, Diagnostic Imaging Cham (CH), Springer, Chapter 2.
- Genetic Alliance District of Columbia Department of Health. Understanding Genetics: A District of Columbia Guide for Patients and Health Professionals. Genetic Alliance 2010 Feb 17. Chapter 2, Diagnosis of a Genetic Disease, Washington (DC), USA.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...