Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4579
Research Article(ISSN: 2637-4579) 
Evaluation of Knee Kinematics in Single Radius versus Multi-Radii Total Knee Arthroplasty in India Population : A Randomized Control Trial Volume 1 - Issue 3
Lalit Maini1, Ankur Sharma*1, Anshul Goel2, Amit Sharma1, Surabhi Rohilla1, Sunil Jha3, Ashish Indani4 and Srinivas Reddy Boreddy4
- 1Department of Orthopaedics, LokNayak Hospital, India
- 2Department of Orthopedics, Wrightington Hospital, UK
- 3Biomedical Engineering, Indian Institute of Technology, India
- 4Medical Writing Domain, TATA Consultancy Services, India
Received: February 20, 2018; Published: February 28, 2018
Corresponding author: Ankur Sharma, LokNayak Hospital, orthopaedics, Bahadur Shah Zafar Marg, New Delhi, IN 110006,Tel: 01123232400; Email: lalit_maini@rediifmail.com
DOI: 10.32474/OAJBEB.2018.01.000112
Abstract
Purpose: Single radius (SR) TKA implant designs are theoretically claimed to overcome "mid-flexion instability" and decrease quadriceps loading encountered in multiple radii (MR) designs. However, limited/no data is available to support SR over MR designs especially in Indian population.
Methods: The present study is a randomized controlled trial, comparing SR (n=17) and MR (n=13) knee kinematics based on clinical scores (Knee Society Score; KSS), radiological (Lotke score), fluoroscopic, and electro-goniometric data in patients. Fluoroscopic evaluation was done by contour based (2D/3D) registration technique.
Results: Patients demographics, KSS, radiological and electro-goniometric data were comparable between SR and MR TKA groups. Anatomically, axial rotation and condylar lift-off data showed insignificant differences. However, MR TKA knees showed higher (P < 0.05) antero-posterior translation compared to SR TKA knees. Similarly, electro-goniometry data has shown no statistical significant difference between both the groups in terms of unloaded flexion-extension, internal-external rotations, walking, and sit- to-stand flexion/rotation.
Conclusion: The study showed no statistical significant difference between the two knee implant designs based on clinical, radiological and goniometric data except antero-posterior translation. Mid-flexion instability was not seen with MR TKA which was projected as the major problem with these designs.
Keywords: Electrogoniometry; Fluoroscopy; Knee Society Score; TKA; 2D over 3D registration.
Introduction
Total Knee Arthroplasty (TKA) is an established procedure for end-stage osteoarthritis of knee joint which relieves patients' pain and improves the quality of life [1-3]. A successful TKA demands precise surgical technique, appropriate materials, sound implant design and kinematics, and patient compliance with rehabilitation [4]. Implant design has undergone tremendous changes in the past few years. Initially, multi radii (MR) TKA knee implant was designed based on the hypothesis that normal knee joints have multiple instantaneous centres of flexion-extension [5,6]. However, the concept has been challenged by recent studies which propose a constant centre of rotation, hence the basis of newly introduced single radius (SR) implant designs [7-9]. An important aim of TKA is in replicating the normal knee kinematics [4,10,11], which helps in increasing the longevity of implant and eventually patient satisfaction.
Mid-flexion instability and quadriceps loading were the primary hurdles which were proposed to be averted with new SR implants [11-13]. Other proposed biomechanical advantage with the SR design was that the knee flexion-extension axis is situated more posteriorly in the SR design than the MR TKA design that leads to longer quadriceps moment arm and hence making it biomechanically more efficient [11]. The SR TKA has also been reported to improve anterior knee function, stability, and flexion with greater proprioception than MR implants [12,13]. However, limited or no data is available on the head-on comparison of SR and MR implant's kinematics in TKA patients post-surgery especially in Indian population. In the present randomized control trial, we compared SR and MR implant designs using clinical, radiological and goniometric analysis in Indian patients who were undergone TKA. We used 2D fluoroscopy over implant 3D registration technique (Mimics 17.0 software, Materialise NV, Leuvan, Belgium) to visualize implants structures and relative position and electro-goniometry to analysis functional parameters of knees.
Material and Methods
Patients
Patients (age 50-70 years) who were undergoing TKA due to the primary osteoarthritis of the knee between October 2013 and December 2014 were included in the trial. Patients were initially randomized patient-wise to either SR or MR groups until each group had at least 12 knees. If a patient was undergoing a bilateral TKA, then both knees were implanted with same type of implant (SR/MR) and counted as two individual knees. The key inclusion criteria were patients with primary osteoarthritis of single or both knee with Kellgren Lawrence classification grade ≥ 3; at least 3 to 4 months follow-up post TKR; Knee Society Score (KSS) > 70 and Lotke radiological score > 80, 3 months post TKR; at least 3 months gap post TKA for sequential bilateral TKA. The key exclusion criteria were patients with secondary osteoarthritis; hip arthritis and previously operated hip conditions; any deformity of foot or ankle; lost to follow-up; dementia; neuropathic joints; revision knee Arthroplasty; and history of septic arthritis in the same knee.
Ethics
The studies were conducted in accordance with Good Clinical Practice, ISO 14155, Institutional Ethics Committee, and in compliance with the approved protocol and applicable regulatory requirements. All patients provided written informed consent before entering the study.
Study Design and Settings
The present study was a randomized controlled trial, comparing in vivo SR and MR knee kinematics based on clinical score, radiological scores, fluoroscopic, and electro-goniometric data. The study was conducted in tertiary care orthopaedic centres in India.
Study Treatments
Radiographs of bilateral knee antero-posterior and lateral views were taken for all the patients along with a standing scanogram to calculate the mechanical and anatomical axes. Grading of osteoarthritis was done according to Kellgren Lawrence classification [14]. All the eligible patients were randomized in to two groups, SR TKA and MR TKA. Knees in SR TKA group were implanted with Scorpio Single Axis implants (Stryker, Orthopaedics, USA), whereas knees in MR TKA group implanted with Genesis II implants (Smith &Nephew, USA).
All patients were operated by the same surgeon using standard medial parapatellar approach under tourniquet cover. On the day 1 of post-surgery, patients were mobilized with brace and knee range of motion exercises (flexion-extension) and quadriceps exercises were initiated. After 3 months of follow-up, post-TKA fresh radiographs and scanogram of knee were taken and patient were evaluated against the clinical (KSS) [15] and radiological score (Lotke) [16]. All the eligible patients with clinical score of ≥ 70 and radiological score of ≥ 80 were taken up for further assessments.
Study Assessments
We used earlier reported contour matching technique, also known as 2D/3D registration technique, to analyze the position of implants in vivo [17]. A library of computer aided design (CAD) models of silhouette was built on 3D images of prostheses obtained from digitized single-view fluorescence 2D images of prostheses (MIMICS software, Materialise NV, Leuvan, Belgium). The CAD generated silhouette images were superimposed on corresponding fluoroscopic image extracted silhouette to evaluate relative motion of femur and tibia as per the standard joint coordinate systems (Grood and Suntay)[18].
Figure 1: A representative lateral view fluoroscopic images of patient's knees at 90° (1A) and 0° (1B). A representative knee implants lateral view (1C) and antero-posterior view(1D) overlap images showing condylar lift-off.
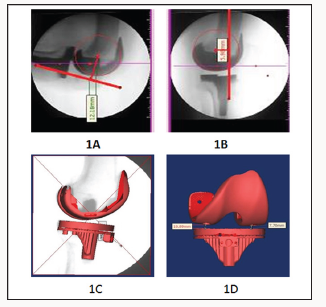
Antero-Posterior Translation: Antero-posterior translation of femoral component was evaluated by comparing the femoral component movement using lateral fluoroscopic views (0° and 90°) at a 90° flexion (Figures 1A & 1B). A circle was drawn to best fit the femoral component and the centre of circle position was analyzed in 0° and 90° with respect to the anterior margin of the tibial peg, a reference line.
Femoral Component Lift-Off: The femoral component lift-off was calculated as the distance between medial and lateral condyles from tibial plateau in the superimposed image. For calculations, the superimposed images were rotated by 90° to obtain the anteroposterior view (Figures 1C &1D), especially at 30° and 60° flexion to evaluate mid-flexion instability.
Figure 2: A representative image of femoral and tibial component 3D position at 0° (2A), 30° (2B), 45° (2C), 60° (2D), and 90° (2E).
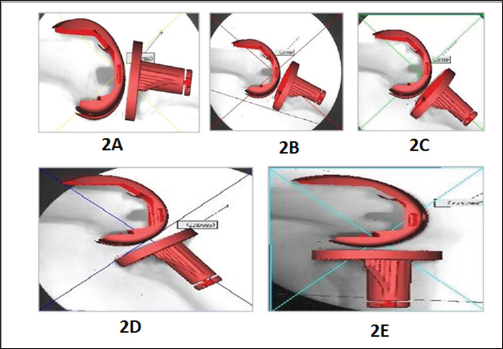
Tibio-Femoral Rotation: The rotation of femoral and tibial components along with internal-external rotation axis and varus/ valgus rotation axis was analyzed by calculating Tibio-femoral relation. The superimposed images were analyzed to find out the 3D position of implants in space. The final 3D position of the femoral and tibial component were analyzed with respect to their base value and then finally with respect to each other at 0°, 30°, 45°,60° and 90° (Figures 2A-2E).
Flexion-Extension Instability: Flexion-extension instability was calculated on fluoroscopic antero-posterior valgus-varus stress view images. To overcome the magnification errors, we calculated the angular joint line opening on these views rather than the linear measurements (Figures 3A & 3B).
Figure 3: Fluoroscopic images showing valgus stress or medial joint line opening (3A) and varus stress view or lateral joint line opening (3B). Representative images showing condylar lift-off at 30° (3C) and 60° (3D).

Statistical analysis
All the data was validated and checked for its veracity; including the outliers. All measurement data (discrete and continuous) was reported in terms of mean and standard deviation. All the categorical data was reported as frequency. The significance analysis was performed with a paired t-test between the arms.
Results
Patient Demographics
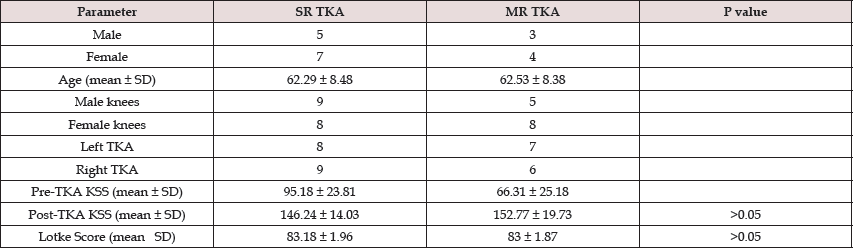
Twenty three patients were evaluated for eligibility criteria, and all the patients met the criteria. Randomly, 15 patients were randomized into SR group and 7 patients were randomized into MR group to make sure an equal number of knees were allocated to each group. MR group had lesser patients compared to SR because most of MR group patients were undergoing bilateral TKA hence the double the number of knees. Four patients were excluded from the study; 3 patients did not meet criteria and 1patient did not meet KSS score (Figure 4). Three months post TKA follow-up, 19 eligible patients (8 male, 11 female) were included in the present study. Of these patients, 11patients had bilateral and 8 patients had single knee TK Aculminating to a total of 30 knee replacements. Seventeen knees were treated with SR implants (5 male, 7 female patients) and rest of the 13 knees were treated with MR implants (3 male, 4 female patients), and none of the bilateral patients had both kinds (SR and MR) of implants. The study included 14 male (9 SR TKA, 5 MR TKA) and 16 female knees (8 SR TKA, 8 MR TKA).There were 8 left and 9 right knees in SR TKA group, whereas 7 left and 6 right knees in MR TKA group. Both the patients groups were similar in demographics and diagnosis (Table 1).
Figure 4: Consort chart of patientís randomization, allocation, and analysis.
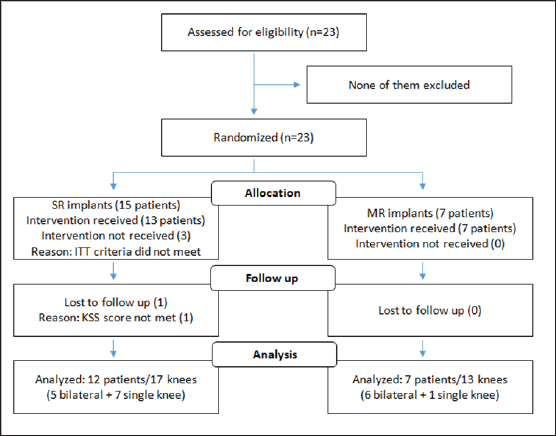
Table 1: Patients Demographics.
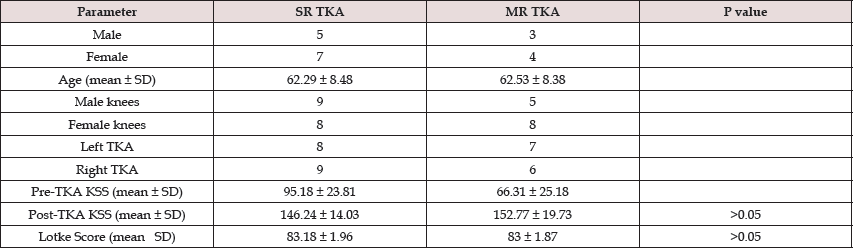
KSS-Knee Society Score; MR -Multi radii implant; SD -Standard deviation; SR -Single radius implant; TKA-Total Knee Arthroplasty
KSS and Lotke Scores: The mean post-operative KSS was improved to 146.24 ± 14.03 and 152.77 ± 19.73 from mean baseline pre-operative score 95.18 ± 23.81 and 66.31 ± 25.18 (P > 0.05) for SR and MR TKA, respectively. The post-operative radiological Lotke Score was 83.18 ± 1.96 and 83 ± 1.87 (P > 0.05) in SR and MR TKA knees, respectively (Table 1).
Anatomical Assessments: The mean antero-posterior translation of SR and MR TKA knees was 6.77 ± 2.34 mm and 9.00 ± 2.95mm (P > 0.05), respectively, at a knee flexion of 90°. Overall, about 36% TKA knees (7 SR and 4 MR TKA) showed medial condylar lift-off, whereas about 53% TKA knees (10 SR and 6 MR TKA) showed lateral condylar lift-off at 30° (Figure 3C); 10% TKA knees did not show any lift-off and all are from MR TKA knee group. At 60°, about 36% TKA knees (6 SR and 5 MR TKA) showed medial condylar lift-off, whereas about 53% TKA knees (10 SR TKA, 7 MR TKA) showed lateral condylar lift-off (Figure 3D); 2 TKA knees did not show lateral condylar lift-off, one from each group (Table 2).The average lift-off values in SR and MR TKA knees were 3.20 ± 2.19mm and 2.16 ± 2.41mm at 30° and 3.10 ± 1.69mm and 3.68 ± 2.63mm at 60°, respectively. In Valgus-varus stress test, SR and MR TKA knees showed medial joint line opening of 1.84° ± 1.14° and 2.42° ± 1.38°, and lateral joint opening of 2.12° ± 1.42° and 1.90° ± 1.31°, respectively. The Axial rotation of all the patients were evaluated after simulation/superimposition at 30°, 45°,60° and 90° and compared with the position at 0° (Figure 5A-5E). The average axial rotation was 3.63° in SR TKA group and 1.51° in MR TKA group. Ten TKA knees each from SR and MR TKA knees followed normal internal rotation of tibia at 0-90°, whereas 7 of 17 SR TKA knees and 3 of 13 MR TKA knees had external rotation of tibia in flexion (reverse rotation). The range of rotation varied from 23.31° to -27.40° and 15.76° to -15.5° for SR TKA and MR TKA knees, respectively, across all degrees of flexion (Table 2).
Figure 5: A representative images of axial rotation at 0° (5A), 30° (5B), 45° (5C), 60° (5D), and 90° (5E).
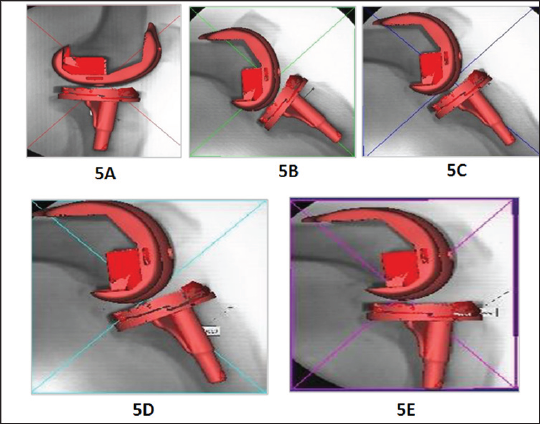
Table 2: Fluoroscopic Assessments.
MR -Multi radii implant; SD -Standard deviation; SR -Single radius implant; TKA -Total Knee Arthroplasty
* Internal rotation of tibia with flexion (normal rotation) ‘‘
**External rotation of tibia with flexion (reverse rotation).
Functional Assessments: In unloaded flexion-extension, SR TKA knees had an active and passive range of motion (ROM) of 107 ± 20.36° and 115.27 ± 21.34 compared to 120.47 ± 17.93° and 126.93 ± 23.14° for MR TKA knees, respectively. In unloaded internal-external rotations, the mean axial rotations in SR TKA knees while performing active and passive ROM was 29.78 ± 16.19° and 32.82±10.92° compared to 21.32±6.67° and 26.65±7.94° Table 3: Electrogionometry Assessments.for MR TKA knees, respectively (Table 3). While walking on a flat surface, SR TKA knees had 60.35±9.46° flexion with a mean axial rotation of 31.05±8.13°, whereas MR TKA knees had 63.83±15.20° flexion and axial rotation of 30.05±12.32°. During sitting to standing movements, SR TKA knees had a flexion of 77.8 ± 9.44° with an axial rotation of 28.03 ± 13.74°, whereas MR TKA knees had a flexion of 84.18 ± 13.35° with an axial rotation of 34.96 ± 6.31° (Table 3).
Table 3: Electrogionometry Assessments.
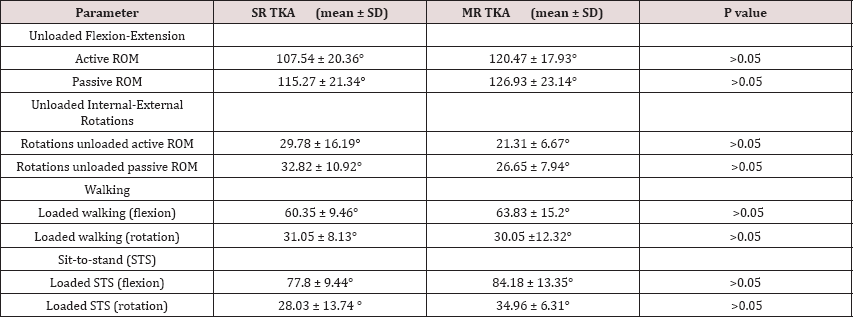
MR -Multi radii implant; SD-Standard deviation; SR-Single radius implant; TKA-Total Knee Arthroplasty.
Discussion
The present was a randomized control trial compared the anatomical and functional parameters of the single and multi-radii TKA implants in Indian patients. Based on clinical, radiological, and goniometric data our study showed no significant difference between the SR and MR knee implant designs in terms of anatomical and functional parameters, except antero-posterior translation. To ensure similar knees were included in both the groups, patients who met KSS and Lotke score, 3 months post-TKA, were included in the study assessments. Patient's KSS score was improved in the post-TKA compared to pre-TKA but was comparable between the SR and MR implant groups. Similarly, there was no statistical difference in radiological Lotke score between the groups. Hence, both the groups were adequately matched in postoperative conditions and any further differences in anatomical and functional parameters of the patient s knees could be attributed to the implant design.
To investigate the anatomical differences between SR and MR implants, we analyzed parameters like antero-posterior translation, femoral component lift-off, valgus/varus instability, and Tibiofemoral axial rotation in post-TKA knees. The MR implants had significantly higher (P>0.05) antero-posterior translation from 0-90° knee flexion than the SR implants and both groups anteroposterior translation was within the range of earlier reported studies [19-21]. Higher antero-posterior translation in MR knees indicates better replication of normal knee kinematics and more posterior roll back was possible with no instability compared to SR knees. The present study's valgus and varus instability (medial/ lateral joint line opening in extension) for SR and MR TKA knees were closer to earlier reported values of 4° and 2° [22], respectively However, there was no statistically significant difference between both the groups in either valgus or varus stress (P<0.05) test indicating that both the groups were matched in their soft tissue balancing.
Although implant design has limited role in femoral component lift-offand primarily depends on soft tissue balancing and component placement, knees from both the groups were showing either medial or lateral condylar lift-off at both 30° and 60°. The average condylar lift-off for both SR and MR implant was within the earlier reported average range of <2mm to 8mm [23]. There was no statistically significant difference between the groups in condylar lift-off. We used electro-goniometry, a previously validated technique, to compare SR and MR TKA knees functionality [24]. Although, MR TKA knees average active and passive ROM was relatively higher than the SR TKA knees, but there was no statistically significant difference between SR and MR TKA knees in term of unloaded flexion-extension active (P>0.05) or passive (P>0.05) ROM. However, both SR and MR TKA knees ROM was similar to earlier reported studies [25]. Similarly, there was no statistical difference in the axial Tibio-femoral rotation during either active or passive ROM (P>0.05 and P>0.05, respectively) between the SR and MR TKA knee groups. Knee excursion while walking and sit-to-stand were well within the earlier reported values [25-27], however there was no statistically significant difference between SR and MR TKA knee excursion.
Overall, our study corroborated earlier studies [28,29] and showed no statistical difference between SR and MR implant in terms of anatomical and functional parameters, however MR implants had better antero-posterior translation than the SR implants. In agreement with earlier reported studies [30], our analysis did not find any mid-range instability of the knees and could not demonstrate enhanced mid-range stability of the SR TKA over the MR TKA.
Conclusion
The present randomized control trial did not show any statistically significant difference between SR and MR implants in terms of knee kinematics based on the fluoroscopic, radiological and goniometrical data except antero-posterior translation. However, conclusion should be interpreted carefully as study has a limitation of fewer subjects.
References
- Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L (2000) Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta orthopaedica Scandinavica 71(3): 262-267.
- Mahomed N, Gandhi R, Daltroy L, Katz JN (2011) The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis 2011: 1-6.
- Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clinical orthopaedics and related research 468(1): 57-63.
- Riley LH (1976) The evolution of total knee arthroplasty. Clinical orthopaedics and related research 120: 7-10.
- Gunston FH (1971) Polycentric knee arthroplasty. Prosthetic simulation of normal knee movement. The Journal of bone and joint surgery British 53(2): 272-277.
- Frankel VH, Burstein AH, Brooks DB (1971) Biomechanics of internal derangement of the knee. Pathomechanics as determined by analysis of the instant centers of motion. The Journal of bone and joint surgery American 53(5): 945-962.
- Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG (1993) The axes of rotation of the knee. Clinical orthopaedics and related research 290: 259-268.
- Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clinical orthopaedics and related research 356: 111-118.
- Iwaki H, Pinskerova V, Freeman MA (2000) Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. The Journal of bone and joint surgery British 82(8): 1189-1195.
- Hawker G, Wright J, Coyte P, Paul J, Dittus R, et al. (1998) Health-related quality of life after knee replacement. The Journal of bone and joint surgery American 80(2): 163-173.
- Lima DD, Poole C, Chadha H, Hermida JC, Mahar A, et al. (2001) Quadriceps moment arm and quadriceps forces after total knee arthroplasty. Clinical orthopaedics and related research 392: 213-220.
- Ezechieli M, Dietzek J, Becher C, Ettinger M, Calliess T, et al. (2012) The influence of a single-radius-design on the knee stability. Technology and health care: official journal of the European Society for Engineering and Medicine 20(6): 527-534.
- Cook LE, Klika AK, Szubski CR, Rosneck J, Molloy R, et al. (2012) Functional outcomes used to compare single radius and multiradius of curvature designs in total knee arthroplasty. The journal of knee surgery 25(3): 249-253.
- Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Annals of the rheumatic diseases 16(4): 494-502.
- Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clinical orthopaedics and related research 248: 13-14.
- Ecker ML, Lotke PA, Windsor RE, Cella JP (1987) Long-term results after total condylar knee arthroplasty. Significance of radiolucent lines. Clinical orthopaedics and related research 216: 151-158.
- Banks SA, Hodge WA (1996) Accurate measurement of three-dimensional knee replacement kinematics using single-plane fluoroscopy. IEEE transactions on bio-medical engineering 43(6): 638-649.
- Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. Journal of biomechanical engineering 105(2): 136-144.
- Tanifuji O, Sato T, Kobayashi K, Mochizuki T, Koga Y, et al. (2011) Threedimensional in vivo motion analysis of normal knees using single-plane fluoroscopy. Journal of orthopaedic science : official journal of the Japanese Orthopaedic Association 16(6): 710-718.
- Asano T, Akagi M, Tanaka K, Tamura J, Nakamura T (2001) In vivo three-dimensional knee kinematics using a biplanar image-matching technique. Clinical orthopaedics and related research 388: 157-166.
- Pinskerova V, Iwaki H, Freeman MA (2000) The shapes and relative movements of the femur and tibia at the knee. Der Orthopade 29(suppl 1) S3: S5.
- Romero J, Stahelin T, Binkert C, Pfirrmann C, Hodler J, et al. (2007) The clinical consequences of flexion gap asymmetry in total knee arthroplasty. The Journal of Arthroplasty 22(2): 235-240.
- Dennis D, Komistek R, Scuderi G, Argenson JN, Insall J, et al. (2001) In vivo three-dimensional determination of kinematics for subjects with a normal knee or a unicompartmental or total knee replacement. The Journal of bone and joint surgery American 83A(2): 104-115.
- Walker CR, Myles C, Nutton R, Rowe P (2001) Movement of the knee in osteoarthritis. The use of Electrogoniometry to assess function. The Journal of bone and joint surgery British 83(2): 195-198.
- Myles CM, Rowe PJ, Walker CR, Nutton RW (2002) Knee joint functional range of movement prior to and following total knee arthroplasty measured using flexible Electrogoniometry Gait & posture 16(1): 46-54.
- Rowe PJ MC, Hillmann SJ, Hazlewood ME (2001) Validation of flexible electro goniometry as a measure of joint kinematics. Physiotherapy 87(9): 479-488.
- van der Linden ML, Rowe PJ, Nutton RW (2008) Between-day repeatability of knee kinematics during functional tasks recorded using flexible Electrogoniometry. Gait & posture 28(2): 292-296.
- Jo AR, Song EK, Lee KB, Seo HY, Kim SK, et al. (2014) A comparison of stability and clinical outcomes in single-radius versus multi-radius femoral design for total knee Arthroplasty. The Journal of Arthroplasty 29(12): 2402-2406.
- Liu S, Long H, Zhang Y, Ma B, Li Z (2016) Meta-Analysis of Outcomes of a Single-Radius Versus Multi-Radius Femoral Design in Total Knee Arthroplasty. The Journal of Arthroplasty 31(3): 646-654.
- Stoddard JE, Deehan DJ, Bull AM, McCaskie AW, Amis AA (2013) The kinematics and stability of single-radius versus multi-radius femoral components related to mid-range instability after TKA. Journal of orthopaedic research : official publication of the Orthopaedic Research Society 31(1): 53-58.
Editorial Manager:
Email:
biomedicalengineering@lupinepublishers.com

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...