Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2690-5752
Research Article(ISSN: 2690-5752) 
Obesity and Age Trend among Rural Adults of Daspur I Block, Paschim Medinipur, West Bengal Volume 5 - Issue 1
Mahua Chanak and Kaushik Bose*
- Department of Anthropology, Vidyasagar University, India
Received:August 03, 2021 Published: August 23, 2021
Corresponding author:Kaushik Bose, Department of Anthropology, Vidyasagar University, Midnapore, West Bengal, India
DOI: 10.32474/JAAS.2021.05.000202
Abstract
Background: Obesity is considered a major health problem in both developed and developing countries. Excess weight is one of the leading causes of morbidity and mortality, and it is increasing substantially worldwide. Once considered a high-income country problem, obesity and overweight are now on the rise in low- and middle-income countries. The objective of the present study was to know the prevalence of overall obesity (BMI≥25.0) and central obesity among rural adults. The present study investigated the effect of different age groups (years) on the anthropometric and derived variables and also determined the age trend on obesity among rural adults of Daspur I block, Paschim Medinipur.
Materials and Methods: A community based cross-sectional study was conducted among 805 rural adults (Males=396; Females=409) of Daspur I block, Paschim Medinipur district, West Bengal, from August to December 2019.
Results: In the present study, the total prevalence of overall obesity was 22.4% (19.7% in males and 24.9% in females). The prevalence of central obesity was 45.3% (based on waist circumference), 73.8% (based on waist hip ratio), 65.1% (based on waist height ratio) and 72.3% (based on conicity index) among both sexes. The prevalence of both overall obesity and central obesity was much higher in case of female participants. Obesity (both) was more among females in the age group 31-49 (years) but among males it was ≥50 (years).
Conclusion: Our study revealed a high prevalence of central obesity among rural adults. In overall, the risk of obesity was greater in females. There was a significant association between age and being obese.
Keywords: Obesity; Central Obesity; Rural Adults; Age Group; Waist Circumference; Waist Hip Ratio; Waist Height Ratio; Conicity Index
Introduction
Obesity is considered a major health problem in both developed and developing countries [1-3]. Excess weight is one of the leading causes of morbidity and mortality, and it is increasing substantially worldwide [4-6]. Once considered a high-income country problem, obesity and overweight are now on rise in low- and middleincome countries [7]. In countries with low-income, obesity mostly affects middle-aged adults (especially women) from wealthy, urban environments, whereas in high income countries, it affects both sexes for all ages, but it is disproportionately more common in disadvantaged groups [6,8]. Central obesity (CO) and overall obesity has been associated with an increase in age and it is more prevalent in females [6,9-12]. One in three adults of normal weight had CO [13]. Overall obesity poses a significant threat to human health, and distribution of body fat is one of the major parameters for determining this threat [13-15]. Obesity bestows cardiometabolic diseases and CO is a better predictor of cardiovascular risk than overall obesity [13,16-17]. Overweight and obesity increases the risk of several types of cancers (especially breast cancer among females) and raise cholesterol, insulin resistance and blood pressure [18-20]. With increase in abdominal fat, the risk of CO and associated ailments increases [13,16]. Therefore, abdominal fat deposition measured by waist circumference (WC) has been recommended as a better indicator of obesity in relation to metabolic syndrome, cardiovascular diseases, and type 2 diabetes compared to body mass index (BMI) [21,6]. Along with gender, lifestyle habits like intake of high protein diet, more restaurant visits, less homemade tiffin intake, alcohol consumption were found to be significantly associated with obesity. Intake of fish, day-time sleep physical activity, high protein diet, were also found to be significantly correlated to normal-weight obesity [22]. Hypertension, diabetes and hyperlipidemia were significantly associated with CO among adults with normal BMI [23]. Increased age, urban residence, less walking per day, more time spent on television and being married were all associated with having CO among adults [11]. Family history of obesity and fatigue were risk factors for obesity [24]. Recent studies emerging from different countries of world have shown that obesity may be an independent factor to predict the risk and outcome of COVID-19 patients [25- 31].
Approximately 39.0% of the global adult population were classified as overweight (BMI 25.0–29.9 kg/m2) or obese (BMI > 29.9kg/m2) in 2014; a doubling since 1975 [32]. Since 1975, worldwide obesity has nearly tripled in numbers [7]. In 1975, the prevalence of obesity was 6.4% among females and 3.2% among males, whereas it had risen to 14.9% and 10.8%, respectively by 2014 [32,33]. In 2016, more than 1.9 billion adults (18 years and older) were overweight and over 650 million were obese, out of which over 340 million children and adolescents aged 5-19 were overweight or obese. In 2016, the prevalence of obesity and overweight among adults were 13.0% and 39.0%, respectively. Most of the world’s population live in countries where the mortality rate due to obesity and overweight is more than underweight. In 2019, 38 million children under the age of 5 were obese and overweight. Globally there are more people who are obese than underweightthis happens in every part except parts of Sub-Saharan Africa and Asia [7]. In developing countries like India, the increasing prevalence of overweight and obesity has coincided with the demographic and epidemiological transitions, where mortality and fertility have declined, and lifestyle-related diseases have become more common [33-36]. The prevalence of overweight and obesity in India is alarmingly growing faster than the global average. For instance, the prevalence of overweight increased significantly from 8.4% to 15.5% among females between 1998 and 2015, and the prevalence of obesity increased from 2.2% to 5.1% over the same period [33,37-39]. Despite the above figures, only a few studies have attempted to estimate future trends in overweight and obesity in India. One study that reports on global trends estimated that by 2030, 27.8% of all Indians would be overweight, and 5.0% obese [33,40]. Another study estimated that around 20.0% of rural Indian adults will be either overweight or obese by 2030 [41,33]. There are fewer studies about the impact of obesity in rural adults compared to urban adults. Many national and international studies have accounted for both overall as well as CO, but such investigations are lacking from rural West Bengal. Our study reports the prevalence and age trend of obesity (overall and CO) among rural adults of Daspur I block, Paschim Medinipur, West Bengal.
Materials and Methods
It was a community based cross-sectional study conducted among rural adults of Daspur I block, Paschim Medinipur district, West Bengal. Data collection was done from August to December, 2019. The participants were selected from 4 villages (Rajnagar, Gokulnagar, Jadupur, Ramdebpur) under Daspur I block of Paschim Medinipur district, West Bengal, India. A total of 805 rural adults (Male=396, Female=409), aged above 18 years in those villages were included in this study. Consent was taken from the villagers by explaining the purpose of the study and those who had shown interest in participation were included in the present study. Verbal consent has been taken from each participant before initiating the study. None of the participants had any physical deformity. Age (years) of the participants was recorded from identity proofs issued by the Government. All anthropometric measurements were taken by the first author (MC) using standard procedures [42] (Lohman et al. 1988). Height [HT (cm)], weight [WT (kg)], waist circumference [WC (cm)], hip circumference [HC (cm)] were measured. Height (cm) was measured using Martin’s anthropometric rod to the nearest 0.10 cm. The participants were asked to stand upright without shoes, heels together and eyes directed forward. Weight (kg) was measured with a portable weighing machine that was kept on a firm horizontal flat surface. Participants were asked to wear light clothing, and weight was recorded to the nearest 0.5 kg. Waist circumference (cm) and HC (cm) were measured using a nonstretchable measuring tape. The technical error of measurement (TEM) of anthropometric measurements was calculated using the standard procedure [43]. For calculating TEM, a total of 50 adults were selected randomly from studied area. The TEM was calculated using the following standard equation:
TEM= √ (ΣD2 /2N)
where: D-difference between the measurements, N-number of individuals.
The coefficient of reliability (R) was calculated from TEM using the following standard equation: R= 1−(TEM)2/SD2 where: SDstandard deviation of the measurements. The values of ‘R’ were subsequently determined from TEM. The intra-observer and interobserver TEM values were observed to be within the cut-off value (R=0.95) as recommended [43].
Body Mass Index (BMI), WHR, WHtR and CI were calculated following these formulae:
BMI = Weight (kg) / Height (m2).
WHR = WC (cm) / HC (cm).
WHtR = WC (cm) / HT (cm).
CI = WC (m) / 0.109 × √ WT (kg) / HT (m) [44].
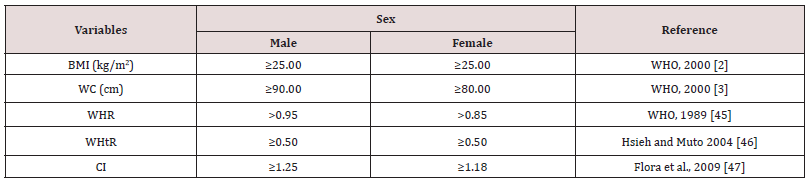
To determine the frequency of BMI (kg/m2) based obesity and central obesity the following standard cut-off values were used in Table 5. One way ANOVA test was performed to test for significant differences in anthropometric and derived variables between age groups among the studied participants. Chi- square (x2) was performed to test for sex differences in the prevalence of BMI based obesity and CO; Chi-square (x2) test was also analysed to find out the association of obesity (both overall and central obesity) with age among both sexes. Age groups were prepared using percentiles (25th and 50th). The total population was categorized into 3 age groups: lower age group: ≤ 30 years, middle age group: 31-49 years and upper age group: ≥ 50 years for further analysis. A p-value of 0.05 was considered to be statistically significant. All the statistical analyses were conducted in SPSS version 16.0.
Results
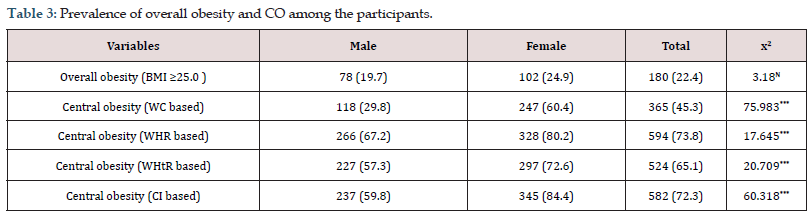
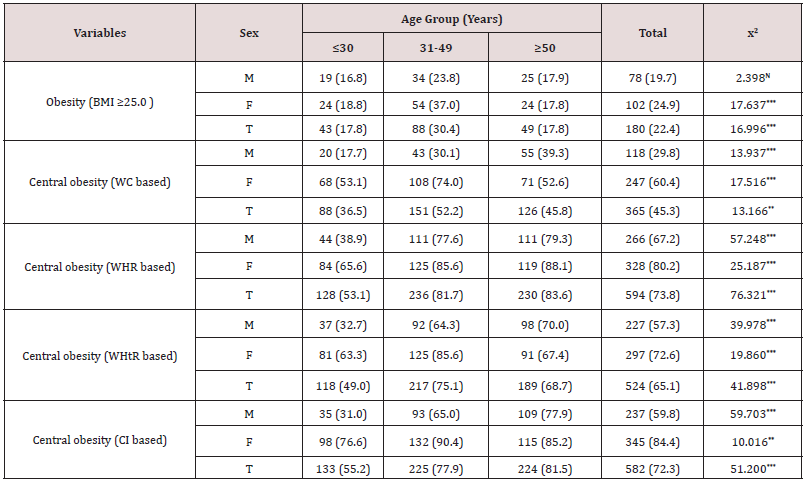
Descriptive statistics (Mean±SD) of anthropometric and derived variables among participants are presented in Table 1. Mean HT (cm), WT (kg), WC (cm) and WHR were found to be more among males than females. Mean HC (cm), BMI (kg/m2), WHtR were higher in females than in males. By using independent sample t-test, it was observed that there were significant statistical differences between both sexes in HT (cm) (p<0.001), WT (kg) (p<0.001), HC (cm) (p<0.001), BMI (kg/m2) (p<0.01), WHR (p<0.001), WHtR (p<0.001). Details of age group (years) specific anthropometric and derived variables (Mean ± SD) among the participants are presented in Table 2. Mean HT (cm) for both sexes decreased from lower (≤30 years) to upper age group (≥50 years). Mean WT (kg) and BMI (kg/m2) among both sexes was more in middle age group (31-49 years). Mean WC (cm), HC (cm), WHtR were more in middle age group (31-49 years) among female participants. Mean values of WC (cm), WHR, WHtR, CI increased from lower (≤30 years) to middle (31-49 years) and middle (31-49 years) to upper age group (≥50 years) among males. Mean HC (cm) was more among middle aged (31-49 years) males. Table 3 presents the prevalence of overall obesity and CO among the participants. It was found out that the prevalence of overall obesity (24.9% vs. 19.7) and CO was more among female participants (60.4% vs. 29.8%; 80.2% vs. 67.2%; 72.6% vs. 57.3%; 84.4% vs. 59.8%). The difference between sex and CO was highly significant (p< 0.001) however no significant (p>0.05) difference was observed between overall obesity and sex. Age group specific distribution of overall obesity and CO among the participants is presented in Table 4. The prevalence of obesity (based on BMI) among males and females were more in the age group of 31-49 years. Among males, the prevalence of CO increased with increasing age, but among females, prevalence of CO was high in middle age group (31-49 years). It was also found out that the prevalence of WHR increased with increasing age (years) for females. The association of age (years) and obesity among female participants were significantly high (p<0.001). There was a significant association between CO and age among both sexes.
Table 1: Descriptive statistics (Mean ± SD) of anthropometric and derived variables among the participants.
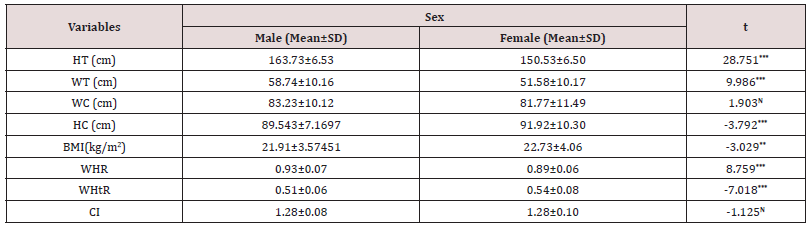
(Mean± Standard deviation; Statistically significant at *** – p< 0.001, ** – p< 0.01and N – Not significant).
Table 2: Age group specific anthropometric and derived variables (Mean ± SD) among the participants.
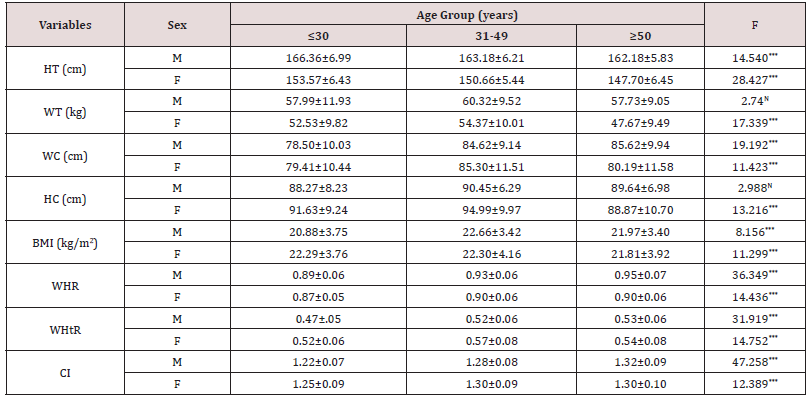
(Mean±Standard deviation; Statistically significant at *** – p< 0.001 and N – Not significant; M – Male, F – Female).
(Percentages are presented in the parentheses; statistically significant at *** – p< 0.001 and N-Not significant).
(Percentages are presented in the parentheses; statistically significant at *** – p< 0.001 and N-Not significant).
Discussion
It is obvious from the present study that females possessed a higher risk for developing obesity more than males. The prevalence of obesity (BMI≥25 kg /m2) was 22.4% (19.7% in males and 24.9% in females). The prevalence of obesity (22.4%) observed in this study was higher than some previous studies in India by [48] in Tamil Nadu (5.5%), [49] in a rural coastal area in South India (14.0%), [50] in rural Meerut (17.7%), [51] in rural Kerala (10.0%) but lower than some other studies done in Punjab (29.4%) by [12], in rural West Bengal (30.4%) by [52], in rural Andhra Pradesh (56.0%) by [53], in rural Pondicherry (27.3%) by Shrivastava et al. (2015) [54].Worldwide, (Nepal, Saudi Arabia, Ethiopia) numerous studies (Rawal et al., 2018, Al-Qahtani, 2019; Darebo et al., 2019) have been conducted by various scholars on the prevalence of obesity among adults and they have revealed a higher prevalence of obesity than our study. In China, a study by Zhang et al. (2016) has revealed a lower prevalence (14.6%) of obesity than the present study. According to our findings, the prevalence of obesity (based on BMI) was significantly higher among females. However, this finding was similar with previous studies in India [53], Ethiopia [19], Northeast China [55], and Saudi Arabia [56] as well; however, in China [57], Tanzania ([58]) the prevalence of obesity was higher in males. In India, obesity was also more common in females in Meerut [50], Punjab [12], Karnataka [59], Tamil Nadu [60], West Bengal [52]. Various scholars have found out in their studies that the prevalence of obesity was higher in males as compared to females [51,49,22].
Obesity have significant impact with age (years) among both sexes in this study. Among males, prevalence of overall obesity and CO increased from a lower age group (≤30 years) to upper age group (≥50 years) but in case of females, the prevalence increased from lower (≤30 years) to middle age group (31-49 years). The probability of getting obese with increase in age (years) is very high among males, however in case of female participants, middle aged individuals are more likely to get obese than older females as per the present study. Our study has highlighted that more female participants belonging to middle age (31–49 years) group were obese (overall obesity and CO) which was similar to the findings of some recent studies in Iran [61], Bangladesh [62], Nepal [63], India [53,52] but higher (≥50 years) age group was comparatively more obese in China [57], Syria [64] and in Sudan [6]. Age is a very important risk factor for both types of obesity. The prevalence of CO (based on WHR) was observed to be more in females (80.2%) than males (41.7%). In different regions of the world, such gender-based differences in CO prevalence have been reported in many previous studies. Similar findings were also observed in studies [66,13, 52] from different countries of the world such as Egypt (12.4% in males and 44.9% in females), South Africa (51.7% in males and 60.7% in females), India (62.7% in males and 92.3% in females). In Indian context (Kerala, Tamil Nadu, West Bengal), previous studies [66,49,20] have illustrated that CO was more prevalent in females than males. These findings were analogous to the present study. The prevalence of CO based on WHtR was higher among adult Spanish males [67].
The observed differences between the two sexes can be due to both social and biological factors. In developing countries males are more engaged in physical activities than females and hence they may have a reduced risk of obesity. Also there were many studies which suggested that female sex hormones have a great impact on deposition of fat, and thereby increased risk of obesity [68,69,19]. However, in this study the prevalence of CO in females may be due to sedentary lifestyle and practice of less physical activity since most females who live in developing countries, including India are housewives. Thus, they may spend more time at home with less physical activities [70, 71, 72].
Conclusion
The present study has demonstrated a strong relationship between age and obesity. An interesting finding is that the prevalence of obesity was higher among middle aged females and showed no increase with increasing age. The Government policy makers and other health related stakeholders should consider obesity as a growing public issue and therefore there is an urgent need for national awareness programs among rural population to reduce obesity and associated comorbidity and mortality.
Acknowledgements
The authors gratefully acknowledged to all the participants of Daspur I block for their cooperation and patience. Authors would like to acknowledge the Department of Anthropology, Vidyasagar University, Midnapore for providing necessary support to conduct the fieldwork. The authors would also like to express their thanks to Kalyani Chanak, Madhusudan Chanak, Barun Ghosh, Tapash Ghosh, Pratim Roy for their support and cooperation. MC received the financial assistance from the University Grants Commission (Swami Vivekananda Single Girl Child Scholarship for Research in Social Sciences).
Statement of Conflict
The authors declare no conflict of interest.
Authors Contributions
MC designed the study and collected the data. Data entry and analyses were performed by her. She also prepared and edited the manuscript. KB designed the study, analysed the data and edited the manuscript.
References
- (2000) World Health Organization, Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. Geneva: World Health Organization.
- (2000) World Health Organization, International Association for the Study of Obesity, International Obesity Task Force. The Asia Pacific Perspective: Redefining Obesity and its Treatment. Sydney: Health Communications p. 229.
- (2000) WHO/IASO/IOTF, The Asia-Pacific perspective: redefining obesity and its treatment. Melbourne: Health Communications Australia.
- Al Kandari Y Y (2006) Prevalence of obesity in Kuwait and its relation to sociocultural variables. Obesity Reviews 7(2): 147-154.
- Mohieldin A K Sifeldin, D Adam, K Albassir (2015) Obesity prevalence and physical inactivity among adults of karari locality, Khartoum state Sudan, 2014. International Journal of Health Sciences 3(1): 185-190.
- Omar SM, Z Taha, AA Hassan, O Al Wutayd, I Adam (2020) Prevalence and factors associated with overweight and central obesity among adults in the Eastern Sudan. PLoS ONE 15(4): e0232624- e02334.
- (2021) World Health Organization, Obesity and overweight. Geneva: World Health Organization.
- Swinburn BA, G Sacks, KD Hall, K McPherson, DT Finegood, et al (2011) The global obesity pandemic: Shaped by global drivers and local environments. Lancet 378(9793): 804-814.
- Mirzazadeh A, B Sadeghirad, AA Haghdoost, F Bahreini, M Rezazadeh Kermani (2009) The prevalence of obesity in Iran in recent decade; a systematic review and meta-analysis study. Iranian Journal of Public Health 38(3): 1-11.
- Ali Y A, A O Almobarak, H Awadalla, W M Elmadhoun, M H Ahmed (2017) Obesity among Sudanese adults with diabetes: A population-based survey. Annals of Translational Medicine 5(12): 252-260.
- Munyogwa MJ, AH Mtumwa (2018) The Prevalence of Abdominal Obesity and Its Correlates among the Adults in Dodoma Region, Tanzania: A Community-Based Cross-Sectional Study. Advances in Medicine 2018: 1-8.
- Singh S, RK Sabharwal, JK Bajaj, IR Samal, M Sood (2019) Age and gender based prevalence of obesity in residents of Punjab, India. International Journal of Basic & Clinical Pharmacology 8(5): 1038-1043.
- Owolabi EO, D Ter Goon, OV Adeniyi (2017) Central obesity and normal-weight central obesity among adults attending healthcare facilities in Buffalo City Metropolitan Municipality, South Africa: a cross-sectional study. Journal of Health, Population, and Nutrition 36(1): 54-63.
- Bhaskaran K, I Douglas, H Forbes, I Dos Santos-Silva, D A Leon, L Smeeth (2014) Body-mass index and risk of 22 specific cancers: A population-based cohort study of 524 million UK adults. Lancet 384(9945): 755-765.
- Flegal KM, BK Kit, H Orpana, BI Graubard (2013) Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 309(1): 71-82.
- Cameron AJ, DJ Magliano, JE Shaw, PZ Zimmet, B Carstensen, et al (2012) The influence of hip circumference on the relationship between abdominal obesity and mortality. The International Journal of Epidemiology 41(2): 484-494.
- Bastien M, P Poirier, I Lemieux, JP Després (2014) Overview of epidemiology and contribution of obesity to cardiovascular disease. Progress in Cardiovascular Diseases 56(4): 369-381.
- (2003) World Health Organization, Diet, nutrition and the prevention of chronic diseases: Report of the joint WHO/FAO expert consultation. Geneva: World Health Organization.
- Darebo T, A Mesfin, S Gebremedhin (2019) Prevalence and factors associated with overweight and obesity among adults in Hawassa city, southern Ethiopia: a community based cross-sectional study. BMC Obesity 6: 8-18.
- Chanak M, K Bose (2019) Central obesity and hypertension among rural adults of Paschim Medinipur, West Bengal, India. Anthropological Review 82(3): 239-252.
- Eckel RH, SM Grundy, P Z Zimmet (2005) The metabolic syndrome. Lancet 365(9468): 1415-1428.
- Hadaye RS, RM Manapurath, BP Gadapani (2020) Obesity prevalence and determinants among young adults, with special focus on normal-weight obesity; a cross-sectional study in Mumbai. Indian Journal of Community Medicine 45(3): 358-362.
- Zhang P, R Wang, C Gao, L Jiang, X Lv, et al (2016) Prevalence of Central Obesity among Adults with Normal BMI and Its Association with Metabolic Diseases in Northeast China. PLoS ONE. 11(7): e0160402- e0160412.
- Makkawy E, AM Alrakha, AF Al Mubarak, HT Alotaibi, NT Alotaibi, et al (2021) Prevalence of overweight and obesity and their associated factors among health sciences college students, Saudi Arabia. Journal of Family Medicine and Primary Care 10(2): 961-967.
- Zheng KI, F Gao, XB Wang, QF Sun, KH Pan, et al (2020) Obesity as a risk factor for greater severity of COVID-19 in patients with metabolic associated fatty liver disease. Metabolism 108:154244-154253.
- Sattar N, IB McInnes, JJV McMurray (2020) Obesity is a risk factor for severe COVID-19 infection: Multiple potential mechanisms. Circulation 142(1): 4-6.
- Kassir R (2020) Risk of COVID-19 for patients with obesity. Obesity Reviews 21(6): e13034- e13039.
- Caussy C, F Wallet, M Laville, E Disse (2020) Obesity is associated with severe forms of COVID-19. Obesity (Silver Spring) 28(7): 1174-1175.
- Mauvais Jarvis F (2020) Aging, male sex, obesity, and metabolic inflammation create the perfect storm for COVID-19. Diabetes 69(9): 1857-1863.
- Vaughan CJ, H Cronin, PM Ryan, NM Caplice (2020) Obesity and COVID-19: a Virchow's triad for the 21st century. Thrombosis and Haemostasis. 120(11): 1590-1593.
- Mohammad S, R Aziz, Al Mahri, S S Malik, E Haji, et al (2021) Obesity and COVID-19: what makes obese host so vulnerable?. Immunity & Ageing 18(1): 1-10.
- Di Cesare M, J Bentham, G A Stevens, B Zhou, Y Lu, et al (2016) Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 387(10026): 1377-1396.
- Luhar S, IM Timæus, R Jones, S Cunningham, SA Patel, et al (2020) Forecasting the prevalence of overweight and obesity in India to 2040. PLoS ONE 15(2): e0229438- e0229457.
- Tandon N, MR Anjana, V Mohan, T Kaur, A Afshin, et al (2018) The increasing burden of diabetes and variations among the states of India: the Global Burden of Disease Study 1990–2016. Lancet Global Health 6(12): e1352-e1362.
- Dandona L, R Dandona, G A Kumar, D K Shukla, V K Paul, et al (2017) Nations within a nation: variations in epidemiological transition across the states of India, 1990–2016 in the Global Burden of Disease Study. Lancet. 390(10111): 2437-2460.
- Prabhakaran D, P Jeemon, M Sharma, GA Roth, C Johnson, et al (2018) The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990-2016. Lancet Global Health 6(12): e1339-e1351.
- (2000) International Institute for Population Sciences (IIPS) and ORC Macro. National Family Health Survey (NFHS-2), 1998-99: India. Mumbai: IIPS.
- (2007) International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005-06: India: Volume I. Mumbai: IIPS.
- (2017) International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4), 2015-16: India. Mumbai: IIPS.
- Kelly T, W Yang, CS Chen, K Reynolds, J He (2008) Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond) 32(9): 1431-1437.
- Swain S, S Chowdhury (2018) Trends of nutritional status among rural adults in six states of India: findings from national survey data. Clinical Epidemiology and Global Health 6(2018): 181-187.
- Lohman TG, AF Roche, R Martorell (1988) Anthropometric Standardization Reference Manual. Chicago: Human Kinetics Books.
- Ulijaszek SJ, DA Kerr (1999) Anthropometric measurement error and the assessment of nutritional status. British Journal of Nutrition. 82(3): 165-177.
- Valdez R, JC Seidell, YI Ahn, KM Weiss (1993) A new index of abdominal adiposity as an indicator of risk for cardiovascular disease. A cross-population study. International Journal of Obesity and Related Metabolic Disorders 17(2): 77-82.
- (1989) WHO, Measuring obesity: classification and description of anthropometric data. Report on a WHO consultation on the epidemiology of obesity, Warsaw, 21–23 October 1987. Copenhagen: World Health Organization Regional Office for Europe.
- Hsieh SD, T Muto (2004) A simple and practical index for assessing the risk of metabolic syndrome during the routine health checkups. Nippon Rinsho 62(6): 1143-1149.
- Flora MS, CGN Mascie Taylor, M Rahman (2009) Conicity index of adult Bangladeshi population and their socio-demographic characteristics. Ibrahim Medical College Journal 3(1): 1-8.
- Easwaran MR, P Sivasubramanian, G Kannan (2019) Prevalence of central obesity and its association with socio demographic profile among young adults attending Outdoor Patient Department of Community Health Centre in Madurai, Tamil Nadu. International Journal of Medical Science and Public Health 8(12): 1023-1028.
- Chauhan RC, NS Chauhan, Manikandan, AJ Purty, AK Mishra, et al (2015) Obesity among adult population of a rural coastal area in South India. International Journal of Scientific Reports 1(3): 155-158.
- Kumar S, SK Garg, JV Singh, M Bhatnagar, H Chopra, et al (2014) Socio demographic correlates of overweight and obesity among adults in rural Meerut. Indian Journal of Community Health 26(4):385-389.
- Binu J, R Harnagle (2014) A study on the prevalence of overweight and obesity and its influencing factors among rural geriatric population in Kerala. International Journal of Current Microbiology and Applied Sciences 3(9): 284-293.
- Karmakar N, U Pradhan, I Saha, S Ray, R Parthasarathi, et al (2019) Overweight and obesity among adults in rural Bengal: A community-based cross-sectional study. CHRISMED Journal of Health and Research 6(1): 23-29.
- Undavalli VK, SC Ponnaganti, H Narni (2018) Prevalence of generalized and abdominal obesity: India’s big problem. International Journal of Community Medicine and Public Health 5(4): 1311-1316.
- Shrivastava SR, AG Ghorpade, PS Shrivastava (2015) Prevalence and epidemiological determinants of obesity in rural Pondicherry, India-A community based cross sectional study. Al Ameen Journal of Medical Sciences 8: 3-10.
- Yu S, L Xing, Z Du, Y Tian, L Jing, et al (2019) Prevalence of Obesity and Associated Risk Factors and Cardiometabolic Comorbidities in Rural Northeast China. Biomed Research International 2019: 6509083-6509089.
- Al Qahtani (2019) prevalence and Predictors of Obesity and Overweight among Adults Visiting Primary Care Settings in the Southwestern Region, Saudi Arabia. Biomed Research International 2019: 1-5.
- Wang R, P Zhang, C Gao, Z Li, X Lv, et al (2016) Prevalence of overweight and obesity and some associated factors among adult residents of northeast China: a cross-sectional study. BMJ Open 6(7): e010828- e010837.
- Zubery D, J Kimiywe, HD Martin (2021) Prevalence of Overweight and Obesity, and Its Associated Factors Among Health-care Workers, Teachers, and Bankers in Arusha City, Tanzania. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy 14: 455-465.
- Nagendra K, C Nandini, M Belur (2017) A community based study on prevalence of obesity among urban population of Shivamogga, Karnataka, India. International Journal of Community Medicine and Public Health 4(1): 96-99.
- Murugan R, M Therese (2016) Prevalence and associated factors of obesity among adults in Tamil Nadu state, South India. International Journal of Current Research 8(9): 38193-38200.
- Ghadiri Anari A, M Jafarizadah, A Zare, H Mozaffari Khosravi, M Afkhami Ardekani, et al (2014) Prevalence of Obesity and Overweight among Adults in Iranian Population (Yazd Province). Iranian Journal of Diabetes and Obesity 5(2): 67-70.
- Siddiquee T, B Bhowmik, NCDV Da Vale Moreira, A Mujumder, H Mahtab, et al (2015) Prevalence of obesity in a rural Asian Indian (Bangladeshi) population and its determinants. BMC Public Health 15: 860-869.
- Rawal LB, K Kanda, RA Mahumud, D Joshi, S Mehata, et al (2018) Prevalence of underweight, overweight and obesity and their associated risk factors in Nepalese adults: Data from a Nationwide Survey, 2016. PLoS ONE 13(11): e0205912- e0205926.
- Bakir MA, K Hammad, L Mohammad (2017) Prevalence of obesity, central obesity, and associated socio-demographic variables in Syrian women using different anthropometric indicators. Anthropological Review 80(2): 191-205.
- Abolfotouh M A, LA Soliman, E Mansour, ME Farghaly, AA Dawaiaty (2008) Central obesity among adults in Egypt: prevalence and associated morbidity. Eastern Mediterranean Health Journal 14(1): 57-68.
- Bindhu A, K Thankam, R Jose, P Benny, N Beevi, J Haran (2019) Prevalence of obesity and overweight among adults in a rural area in Trivandrum-a cross sectional study. IMA Kerala Medical Journal 12: 31-34.
- López Sobaler AM, A Aparicio, J Aranceta Bartrina, A Gil, M Gonzalez Gross, et al (2016) Overweight and general and abdominal obesity in a representative sample of Spanish adults: findings from the ANIBES study. BioMed Research International 2016: 8341487-8341498.
- Law J, I Bloor, H Budge, M E Symonds (2014) The influence of sex steroids on adipose tissue growth and function. Hormone Molecular Biology and Clinical Investigation 19(1): 13-24.
- Kautzky Willer A, J Harreiter, G Pacini (2016) Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocrine Reviews 37(3): 278-316.
- Belavý D, M Möhlig, A Pfeiffer, D Felsenberg, G Armbrecht (2014) Preferential deposition of visceral adipose tissue occurs due to physical inactivity. International Journal of Obesity 38: 1478-1480.
- Rathnayake KM, T Roopasingam, MJ Dibley (2014) High carbohydrate diet and physical inactivity associated with central obesity among premenopausal housewives in Sri Lanka. BMC Res Notes 7: 564-569.
- Molla M D, HF Wolde, A Atnafu (2020) Magnitude of Central Obesity and its Associated Factors Among Adults in Urban Areas of Northwest Ethiopia. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy 13: 4169-4178.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...