Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Research Article(ISSN: 2644-1403) 
Study of Chemical Neurolysis, Radiofrequency Ablation and Combined Radiofrequency with Chemical Neurolysis of Lumbar Sympathetic Ganglion in Peripheral Vascular Diseases of the Lower Limbs Volume 3 - Issue 3
Kalpana R Kulkarni1* and Rajendra M Kulkarni2
- 1Prof. & HOD (Dept. of Anaesthesia and Pain Management), DY Patil Medical College, Kolhapur MH, India
- 2Prof. & HOD (Dept. of Surgery), DY Patil Medical College, Kolhapur MH, India
Received: May 27, 2020; Published: June 11, 2020
Corresponding author: Kalpana R Kulkarni, Prof & HOD (Dept. of Anaesthesia and Pain Management), DY Patil Medical College, Kolhapur MH, India
DOI: 10.32474/GJAPM.2020.03.000163
Abstract
Background: Peripheral vascular diseases (PVDs) associated with atherosclerosis, hypertension, diabetes, thromboembolism, chronic regional pain syndrome or Berger’s disease, presents with ischemic manifestations of cold limbs, claudication, ulcers, or gangrene. Chemical lumbar sympathetic block (LSGB) with alcohol/ phenol and radiofrequency ablation (RF) are well-established methods to improve the circulation.
Methods: We conducted prospective observational study in 150 cases of PVDs who underwent chemical LSGB using 5ml of phenol 8% at two levels L2 and L3 under guidance of fluoroscopy (Group CH, n=50), RF ablation of lumbar sympathetic ganglions at L2 and L3 level (Group RF, n=50) and combined RF with chemical LSGB using phenol 5ml 8% at L2and L3level following RF(Group RF+CH, n=50).
Results: There was significant difference in VAS scores at six months of follow up in Group CH Vs Group RF+CH and Group RF Vs Group RF+CH, (mean VAS 2.2 in Group CH, 1.94 in Group RF & 1.26 in Group RF+CH,P <0.001) The mean WD improved significantly at six months in Group RF and RF+CH when compared with Group CH (P<0.001). At six months the temperature rise in affected limb/toe noted was 2.6 in Group CH, 2.76 in Group RF and 2.76 ̊C in Group RH +CH, it was significant for Group CH Vs RF+CH, P<0.05.
Conclusion: We observed significant reduction in VAS score, increase in WD and rise in temperature of the limb in all the groups, but longer lasting effects seen in combined technique in Group RF+CH as compared to sole RF or chemical LSGB.
Keywords: Gangrene, Peripheral vascular diseases, Lumbar sympathetic ganglion block, Chemical neurolysis, Radiofrequency ablation
Introduction
Lumbar sympathectomy is indicated for the treatment of intermittent claudication or rest pain in legs due to ischemia of Buerger’s disease, chronic regional pain syndrome (CRPS) type I,II, thromboembolic phenomena, diabetic ulcers, diabetic neuropathic pain, acute herpes pain, Paget’s disease of bones, hyperhidrosis, chronic pancreatitis and malignant visceral pain. Buerger’s disease is an inflammatory disorder affecting medium sized vessels and adjacent nerves where tobacco plays key role for the disease process. Major presenting symptoms are moderate to severe pain in the limbs, affection of sleep and significant work disability. On Doppler ultrasonography there is reduced/absent flow in peripheral arterial system usually in iliofemoral, popliteal, tibialis posterior and dorsalis pedis artery in patients with ischemic lower limb. Lumbar sympathetic ganglia are present from L2 to L5 paravertebral region where blocking of L2-L3 ganglia blocks the sympathetic fibres of the lower extremities and produces vasodilatation. There are surgical and nonsurgical options available for the treatment of ischemic pain and non-healing ulcers.
Surgical sympathectomy causes lot of trauma and tissue damage, chemical sympathectomy may harm surrounding vital tissue due to drug diffusion but still popular method of neurolysis. LSGB with local anaesthetics (LA) or with adjuvants like alpha 2 agonists clonidine, opioids, NMDA receptor antagonist ketamine, steroids or Botox are used to prolong the pain-relieving effects. A diagnostic LSGB with LA followed by neurolysis of lumbar sympathetic chain is safe and useful method over invasive operative procedure [1,2]. During1930s-1950s chemical lumbar sympathectomy was widely used in treating occlusive arterial disease of the lower limbs as an alternative to amputation [3]. Sympathetic denervation results in increased blood flow, improves the collateral circulation and nutritive value of blood flow and thus decreases the pain transmission. [4,5] Currently RF ablation of LSG is safe and effective option that is gaining popularity for lesser incidence of complications but have concerns of high cost and availability. There are reports of the use of combined methods in the literature but very few studies are available [6,7]. We aimed to study and compare the efficacy of three techniques of LSGB i.e. chemical neurolysis, RF ablation and combined RF +chemical LSGB in successive 150 patients of PVDs. The primary outcome variables for the study were improvement in VAS score, WD and rise in temperature of the affected limb with secondary outcome to assess for immediate and late complications and progress in the wound healing up to six months proposed treatment.
Material & Methods
After obtaining Institutional review board permission and
Informed consent from the patients we conducted a prospective
nonrandomized observational study on 150 patients of PVDs of
lower limbs who underwent chemical LSGB (Group CH, n=50),RF
ablation of LSG (Group RF, n=50) and RF + chemical LSGB (Group
RF+CH, n=50) at our Institution over the period of six years (
2014 to 2019).The inclusion criteria’s were Buerger’s disease
( having history of smoking, cold limbs, colour change of the
skin, hyperhidrosis) with claudication ,gangrene of toes, nonhealing
ulcers, atherosclerotic PVD, diabetic non healing ulcer or
gangrene, chronic post thrombo-embolic vascular obstruction in
lower limbs with ulcer or gangrene, scleroderma with gangrene
of toes and patients with post amputation CRPS. To assess the
circulation in the lower limb all were subjected to arterio-venous
Doppler study or CT angiography of the lower limbs and found
to have reduced or absent flow in illeal-femoral or popliteal and
anterior/posterior tibial and dorsalis pedis artery. Patients with
acute embolic obstruction, extensive multiple ulcers with abscess
or in sepsis with uncontrolled diabetes, on anticoagulant therapy
were excluded for interventional management with LSGB. All the
patients undergoing LSGB were evaluated and optimized as for any
other surgical procedure. General investigations like CBC, blood
sugar, urea, creatinine, ECG, and other specific investigations for
associated co morbidities are done.
Pre and post block visual analogue score (VAS), walking distance
(WD) in meters noted. Presence of arterial pulsations in femoral/
popliteal /posterior tibial and dorsalis pedis noted. Temperature
(Temp.) of the affected limb and non-affected limb measured. The
presence of gangrene /non-healing ulcer and discoloration of the
limbs noted. Informed consent for the procedure was obtained
following proper counselling of the patient and nil by mouth
period of 6-8 hours was observed. Intravenous access for IV fluids
and for anxiolysis midazolam 0.5-2mg with fentanyl 50 mcg was
given. Monitoring for the vitals like pulse, NIBP, ECG, SPO2 started.
Procedure was performed in prone position and a pillow was
placed below the abdomen to obliterate the lordosis. As described
by Reid and co-workers [8] we followed the single needle technique
of LSGB at L2 or L3 vertebral level in prone position. Under aseptic
precautions LA infiltration was given just above or below the tip of
transverse processes i.e. for lateral approach at 6-8cm away from
the midline at level of L2 or L3.A22 G 15cm long spinal needle was
inserted under fluoroscopic guidance in AP view advanced till it
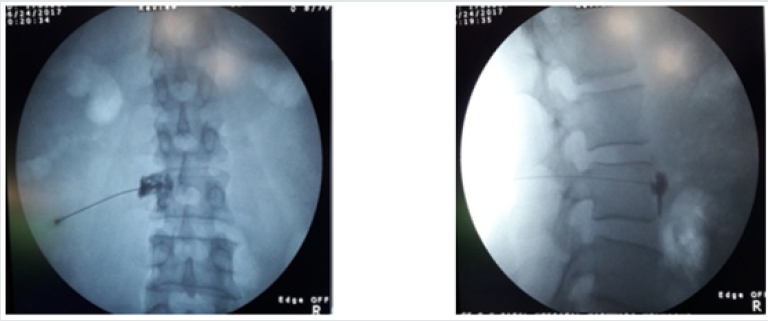
hits the vertebral body. (Figure 1A) Then needle redirected and
advanced fluoroscopy in LAT view until it reached the anterior
border of the vertebral body. (Figure 1B) Following negative
aspiration test 2ml of radio opaque dye (Iohexol, Omnipaque 300)
was injected to confirm the needle position and test dose of LA
lignocaine 1-2 %, 3ml injected and observed for the subjective signs
of pain relief and warmth in the limb (Figure 1) . Later 10-15ml
of 0.25% bupivacaine injected slowly over 10 minute and patient
was made supine. During and after the procedure patient was
monitored for the vitals and for any side effects or complication
for 30 minutes. Significant pain relief rise of temperature of the
affected limb for at least 2-3 ̊C, anhidrosis, change of colour of the
limb and vasodilatation was seen.
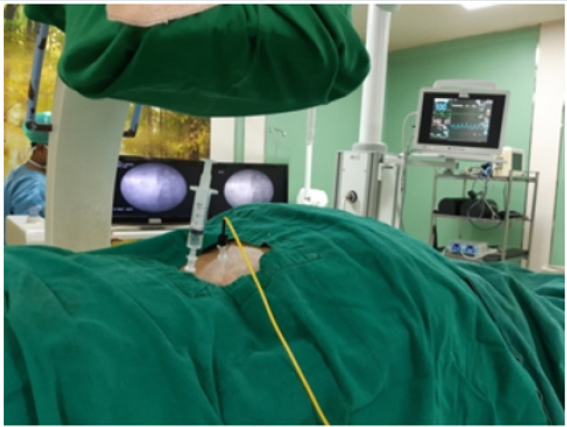
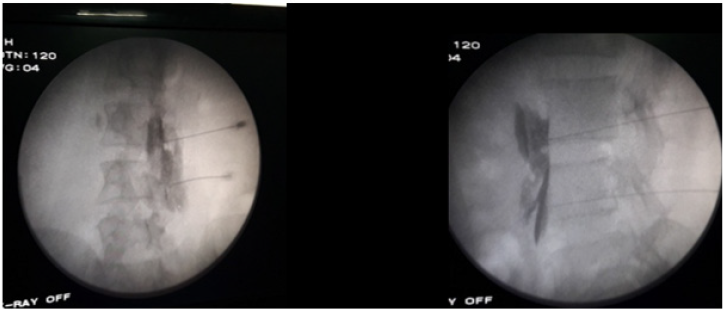
The block was repeated with similar drugs and doses for four successive days to achieve maximum vasodilatation. For chemical neurolysis as described by Rauk, we used double needle method at L2 and L3 vertebral level. [2] On fifth day following injection of test dose of LA either 5 ml of 8% phenol was used for chemical neurolysis (n=50) at two levels L2 & L3.Half ml of air injected before removal of the needles and prone position maintained for half an hour to prevent posterior spread of solution and then patient made supine. RF (NeuroTherm 2000) lesion generator was available since 2015 for use at our Institution. There are studies regarding use of RF for sympatholysis, its comparison with chemical neurolysis with superior results with lesser complications. [9-13] Based on these studies we hypothesized that RF is a better alternative and aimed to study the efficacy of RF and of combined techniques i.e. RF with chemical LSGB using 8% phenol. Thus next patients (n=50) underwent RF ablation of LSG with two needle technique at L2, L3 level using 22G 15cm RF Insulated needles having 10mm active tip. Further we combined the technique of RF ablation with chemical LSGB (n=50) with two needle technique L2 and L3 vertebral level. (Figure 2) Under fluoroscopy two RF needles were placed at the anterolateral border of L 2, L3 vertebra. After negative aspiration test the needles position again confirmed with 1ml of non-ionic contrast and its spread noted under fluoroscopy (Figure 3A, 3B). Sensory and motor testing attempted at L2 then L3 level with the active RF electrode by stimulation with 50HZ and 2 HZ with 0.5 v and 2 v respectively to check the sensory and motor response. This was followed by the injection of test dose 2ml of LA lignocaine at each point. Rise of temperature of 1-2 ̊C within 2-3 minutes in the affected limb measured to confirm the block effect. RF ablation at L2 and L3 level was done at 80-90 ̊C for 90-180 sec.
Figure 3: Figure 3A RF + Chemical LSGB with two needle technique AP view, Figure 3B RF + Chemical LSGB with two needle technique LAT view.
Three such lesions were carried out by advancement of the
tip for 2-5 mm. After initial RF treatment at L2-L3 level chemical
neurolysis of LSG with 5ml 8% phenol was carried out at each level.
Later half ml of air injected before removal of the needles and prone
position maintained for half an hour. Post block sensory and motor
functions were checked after each block in all the patients of LSGB.
IV fluids 10-20ml/kg of ringer’s lactate, antibiotic and analgesic
like IV paracetamol 1 gm, fentanyl 50-100mcg, dexmeditomidine
0.3-0.5 mcg/kg were supplemented as necessary. Post block
pentoxyphylline 400mg TID, Cilastozol 100mg BID, nifedipine
10mg OD and ecosprin 75 OD were continued and NSAIDs were
given for 5-7 days. The patients were discharged after 24 hours of
observations if associated with dry gangrene or CRPS ,some were
discharged at 1-2 weeks for the reason of wound care which was
taken with dressing, antibiotics or surgical debridement /partial
foot/ below knee amputations in severe cases. Pre-block VAS score,
WD and temperature of the limb were noted and compared with
post block scores. Follow up was done every week for a month and
then once a month for six months. Degree of pain relief increase in
WD, changes in the temperature of toe/foot/limb noted. Incidence of
immediate complications like hypotension, bradycardia, LA toxicity,
allergic reaction, signs of spinal/ epidural injection or any other and
late like post-dural puncture headache (PDPH), backache, weakness
in the limb, lateral femoral cutaneous nerve(LFCN) or genitofemoral
neuralgia (GFN) or any other till follow up at six months. Pre and
post LSGB progress of wound and limb edema, colour change
blackening to normal skin colour, gangrene of toes, gangrene of
foot ,non-healing ulcers, amputation of toes, debridements, partial
amputation of foot, below knee amputation of the limb in all the
three groups observed. Progress in terms appearance of line of
demarcation, regression in size of gangrene and ulcer, any need of
debridement or amputation noted. Complications like neuralgias
were treated with oral analgesics, steroids and gabapentinoids.
Statistical Analysis: We included 150 patients of PVDs of lower limb
for this prospective non- randomized observational study admitted
in our Institute over a period of ten years (Jan 2010 to Dec 2019)
who underwent chemical LSGB-(Group CH, n=50) , RF ablation
of lumbar sympathetic ganglion (Group RF, n=50) and combined
treatment of RF+ chemical LSGB (Group RF +CH, n=50) LSGB and
compared with each other for various parameters.
Data and graphs are prepared by using Microsoft Office Excel
2007.Statistical analysis was carried out with SPSS version 23.00.
Quantitative variables like Visual Analog score-(VAS), walking
distance – (WD), temperature (Temp.) were expressed as mean
± standard Deviation (SD) and qualitative data like incidence
of immediate (hypotension, bradycardia, LA toxicity, allergic
reaction, signs of spinal or epidural injection or any other) and late
complications (postdural puncture headache, backache, weakness
in the limb, lateral femoral cutaneous nerve (LFCN) or genitor
femoral neuralgia(GFN) or any other) till follow up at six months
are mentioned as number and proportions /percentage. Pre and
post LSGB progress of wound and limb (oedema, colour change
–blackening to normal skin colour, gangrene of toes, gangrene of
foot ,non-healing ulcers, amputation of toes, debridements , partial
amputation of foot, below knee amputation of the limb) in patients
of all the groups are also mentioned as number and proportions
/percentage The α level for all analysis was set as P<0.05 was
considered as significant. The assessment was analysed using One
Way Analysis of Variances or Kruskal-Wallis One Way ANOVA on
ranks depending on the data distribution.
Results
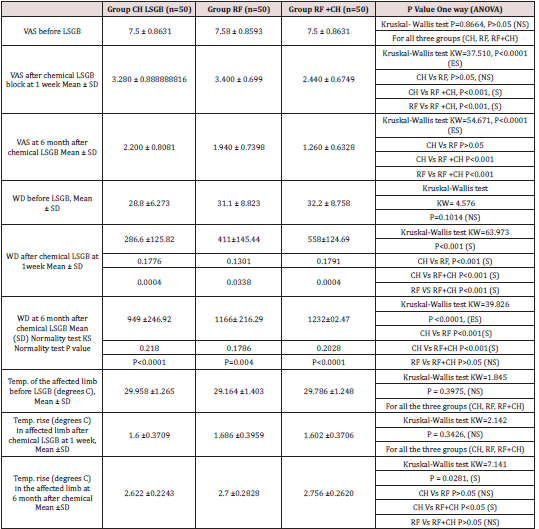
The demographic profile is given in Table 1. There were 150 patients of age ranging from 22years to 90 years, 16 females and 134 males having Buerger’s disease (n=56), atherosclerotic PVD (n=46), diabetic PVD(n=20),CRPS (n=15), post thrombo-embolic ischemia (n=10) and scleroderma associated PVD (n=3) in three groups. They were subjected to chemical LSGB using 8% phenol (Group CH, n=50), RF ablation (Group RF, n=50) and combined RF with chemical LSGB (Group RF +CH, n=50). Table 2 depicts the pre and post LSGB VAS scores, walking distances (WD) and Temp. in ̊ centigrade (degree C) of the affected limb/foot/toe in three groups. The mean VAS score, WD and Temp. of the limb were not significantly different in all the groups (CH , RF, RF+CH ,P>0.05). On follow up at one week of chemical neurolysis and RF treatment there was no significant difference in improved VAS (mean VAS of 3.28 in Group CH and 2.45 in Group RF , P>0.05) over the preblock values ( mean7.5 in Group CH,7.58in Group RF & 7.5 in Group RF+CH).However there was significant difference in VAS scores at 6 months of follow up in Group CH Vs Group RF+CH & Group RF Vs Group RF+CH,(mean 2.2 in Group CH, 1.94 in Group RF& 1.26 in Group RF+CH,P<0.001)but no significant difference when compared in Group CH Vs Group RF (P>0.05).The mean WD after 1 week of follow-up was improved in all the groups (P<0.001) but more significantly in RF & RF+CH group when compared with Group CH.(WD before LSGB =mean 28.8m in Group CH,31.1m in Group RF and 32.2 in Group RF+CH,P>0.05) at 1 week was (287m in Group CH,411m in Group RF,558m in Group RF+CH, P<0.001) Later at six month follow up (mean 949 in Group CH, 1166 in Group RF and 1232 in Group RF+CH) there was significant improvement when compared to WD before LSGB (P<0.0001), and at six months when compared Group CH Vs Group RF and Group CH Vs Group RF+CH (P<0.001) .
Table 1: Demographic profile of the patients with PVDs. Comparison of three groups (Chemical-Group CH, Radiofrequency Ablation-Group RF, combined-Group RF +CH).
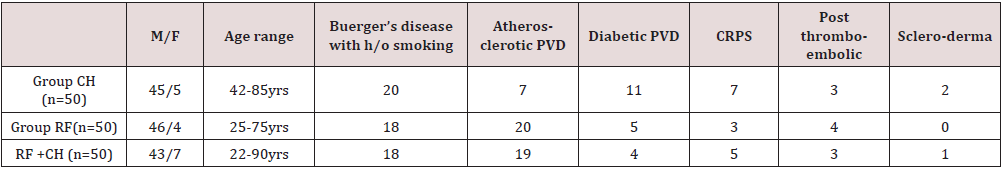
Table 2: Pre and post lumbar sympathetic block(LSGB) observations: (Visual Analog score-VAS, walking distance in meters –WD, temperature in degrees C(Temp.) of the affected limb) Comparison of three groups (Chemical-Group CH, Radiofrequency ablation- Group RF, combined-Group RF +CH).
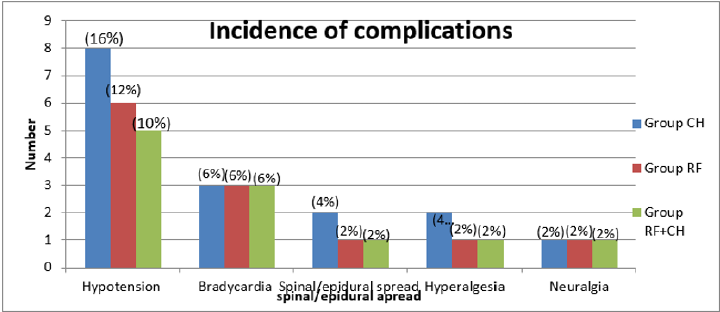
Graph 1: Incidence of immediate (hypotension, bradycardia, LA toxicity, allergic reaction, signs of spinal or epidural injection or any other)and late complications (post-Dural puncture headache, backache, weakness in the limb, lateral femoral cutaneous nerve (LFCN) or genitofemoral neuralgia (GFN) or any other till follow up at 6 months) Comparison of three groups (Chemical- Group CH, Radiofrequency ablation-Group RF, combined-Group RF +CH). Values in number & percentage %.
Graph 2: Pre and post LSGB progress of wound and limb (edema, colour change –blackening to normal skin colour, gangrene of toes, gangrene of foot ,non-healing ulcers, amputation of toes, debridements, partial amputation of foot, below knee amputation of the limb) Comparison of three groups (Chemical-Group CH, Radiofrequency ablation-Group RF, combined- Group RF +CH).Values in number & %.
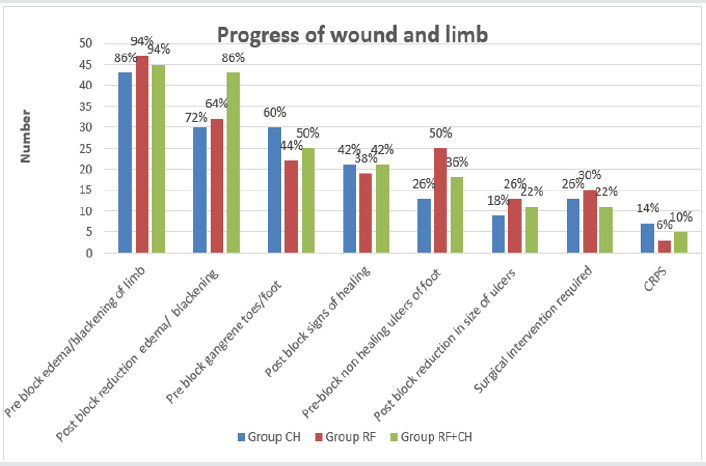
The improvement in WD was comparable in Group RF and RF+CH (P>0.05). Baseline Temp. of the affected limb/toe before LSGB was mean 29.9 in Group CH, 29.2 in Group RF and 29.8 ̊C in Group RF+CH with no difference amongst all the groups (P>0.05). At one week of LSGB there was significant rise in temperature of the affected limb /toe in all the groups when compared with CH V RF,CH Vs RF+CH and RF Vs RF+CH ( mean rise of 1.6 in Group CH,1.69 in Group RF and 1.6 ̊C in Group RF+CH (P >0.05). At six months of follow up the Temp. rise noted was 2.6 in Group CH, 2.76 in Group RF and 2.76 ̊C in Group RH +CH which showed no significant difference if compared in Group CH Vs RF and Group RF Vs RF+CH,P>0.05.Howevere the difference in Temp. rise was significant at six months when compared the Group CH Vs RF+CH, P <0.05. (Graph 1) Shows the Incidence of immediate and late complications till follow up at six months in three groups (CH,RF, RF+CH) in values as number (%).Immediate complications occurred like hypotension in 8(16%),6(12%), 5(10%) and bradycardia in 3(6%),3(6%),3(6%) cases after LSGB in Groups CH, RF, RF+CH respectively. They were managed with fluid boluses, small doses of vasopressors and anticholinergics glycopyrrolate or atropine in appropriate doses. Post block signs of spinal/epidural spread observed in 2(4%), 1(2%), 1(2%) in Groups CH, RF, RF+ CH. All of them responded to fluids and bed rest. Hyperalgesia in the affected, limb/toe was noted in 2(4%),1(2%) and 1(2%) of Group CH, RF, RF+CH respectively after block late. complication like neuralgia after the LSGB treatment observed in 1(2%, GFN), 1(2%, LFCN), 1(2%, LFCN) of Groups CH, RF, RF+CH respectively that was managed with analgesics and gabapentinoids. (Graph 2) demonstrates pre and post LSGB progress of wound and limb. Values in number (%) Pre block edema/ blackening of skin of the limb was present in 43 (86%), 47 (94%),45 (90%) of patients of Groups CH, RF, RF+CH respectively where response to the LSGB was seen in 30(60%), 32(64%), 43(86%) of Groups CH, RF, RF+CH respectively .Gangrene of toes/foot was present in 30(60%), 22(44%), 25(50%) and improvement was seen in 21(42%), 19(38%), 21(42%) of cases of Groups CH, RF, RF+CH respectively. Non-healing ulcers were present in 13(26%), 25(50%), 18(36%) and good response was seen in 9(18%), 13(26%), 11(22%) of Groups CH, RF, RF+CH patients respectively.
In Group CH Interventions required in 13(26%) cases (6 (12%)
cases needed debridement of wounds,3(6%) cases needed partial
amputation of foot,4 (8%) cases required below knee amputation.
In Group RF intervention required in 15 (30%) cases, debridement’s
in 8(16%) cases, partial amputation in 6(12%) cases, and below
knee amputation in 4(8%) cases. In Group RF+CH intervention in
11 (22%) cases (debridement in 5(10%) cases, partial amputation
in 4(8%) cases, below knee amputation in 2(4%) cases. Incidence
of CRPS was 7(14%), 3(6%), 5(10%) of Groups CH, RF, RF+CH
patients respectively. In Group CH 7(14%) CRPS cases had 75%
relief in pain and swelling at three month and 90% at six months
of follow up. In Group RF 100 % relief in 2(4%) at three and sixmonth
1(2%) case had 50% relief at 3 & 6month follow up. In
Group RF+CH 3(6%) cases had 90% relief at 3& 6month 2 (4%) had
75% relief at 3& 6 month of follow up. Discussion Felix Mandl first
described the Selheim’s technique of lumbar sympathetic plexus
block in 1924. He used 6% phenol at cervical ganglion in cats and
suggested phenol for permanent sympathectomy [14,15]. Currently
radiofrequency (RF) ablation of sympathetic ganglion is considered
to be safe and effective option but have concerns of availability and
high cost of treatment. Hence chemical neurolysis is still a popular
method in most of the pain management centres [16-18].
Radiofrequency therapy has two modes pulsed radiofrequency
and thermocoagulation which targets nerve tissue by increasing
temperature where unmyelinated C nerve fibres get dissolved and
become necrotic resulting in vasodilatation in lower extremities
and long-term pain relief improves numbness of neuropathies.
However, accuracy of targeted structure is extremely difficult, and
range of ablation is limited [12,19]. Manjunath et al [13] conducted
a pilot study on 20 patients of CRPS type-I to compare the chemical
neurolysis with 7% phenol and RF lumbar sympathectomy.
Significant pain relief was present in both the groups without
significant difference in mean pain scores between the groups
[13]. Singh et al. conducted fluroscopic guided lumbar chemical
sympathectomy using 8% phenol 8ml at L3 and L4 level following
six successive blocks with LA in fifteen patients suffering from
Beurger’s disease with gangrene of toes. Significant improvement in
VAS scores, WD and healing of toes observed in all the patients with
each successive block. Thus, he concluded that lumbar sympathetic
block is very cost effective, safe and least invasive method for
painful ischemic leg ulcers [20]. As the Buerger’s disease progresses
it results in amputation of gangrenous toes or limbs eventually
leading to persistent post amputation pain and disability. Fifty
such patients were studied by Usmani et al. [21] with chemical
lumbar sympathectomy(n=25) and found significant reduction
in development of phantom limb pain, VAS score, quality of life
compared to control group (n=25) [21] Recently combined chemical
neurolysis and radiofrequency ablation of lumbar sympathetic
ganglion is also studied in PVDs with diabetic techniques but there
are limited studies to establish significant advantage of prolonged
effects with RF over chemical neurolysis [10,13]. Hence combined
methods are studied as by Dhafir A et al. [12] who used pulsed RF
with phenol at three levels (L2,3,4) for lumbar sympathectomy in a
case of CRPS and found satisfactory result [10]. Yuanyuan Ding et
al. [7] conducted comparative study with CT guided chemical Vs RF
Vs RF with chemical (anhydrous ethanol) lumbar sympathectomy
at L2 &L3, for 30 patients in each group in patients with diabetic
peripheral neuropathy and found it safe effective with better
results in terms pain relief and duration and patients satisfaction in
combined treatment group (RF+ chemical) [13] .We too observed
improvement inVAS scores, WD and Temp. rise at one week in all
the groups when compared with values before the LSGB. However
at six months of follow up significant difference in VAS Group CH
Vs Group RF+CH and Group RF Vs Group RF+CH, (mean VAS 2.2 in
Group CH, 1.94 in Group RF& 1.26 in Group RF+CH,P <0.001). The
mean WD improved significantly at six months more in Group RF
and RF+CH when compared with Group CH (mean 949 in Group
CH, 1166 in Group RF and 1232 in Group RF+CH, P<0.001). At six
months the Temp. rise in affected limb/toe noted (2.6 in Group CH,
2.76 in Group RF and 2.76 ̊ C in Group RH 12+CH), was significant
for Group CH Vs RF+CH, P<0.05. The incidences of immediate and
late complications were similar in all the groups. There was good
response to the treatment in all the groups but more satisfactory
in combined LSGB patients when observed for the course of wound
healing following LSGB.
In Group CH all CRPS (7) cases had 90% relief in pain at six
months of follow up. In Group RF 100 % relief in two at six-month,
one case had 50% relief at six month follow up. In Group RF+CH
three cases had 90% relief at six months, two had 75% relief at six
months of follow up. Besides Temp. measurement other objective
tests like ankle/brachial (ABI), sympathetic skin response (SSR)
in response to application of a sensory stimulation using EMG machine. Thus provocative tests like sweat chloride tests, SSR test
and vibratory perception threshold over affected toes and external
malleolus of both sides are methods of objective assessment [22-
24].Infrared thermographic imaging and transcutaneous oxygen
tension (TcPO2).Each test has specific utility and can be used in
combination to obtain information about functional severity of
PVD in patients with claudication. [25,26] Rooke et al. evaluated
influence of sympathetic activity on TcPO2 in ischemic limb. They
measured dorsal foot TcPO2 by oxygen-sensing electrodes with
surface temperatures of 42 degree C and 45 ̊ C. The vasodilatation
Index TcPO2 at 42 ̊C /TcPO2 at 45 ̊C as an index of vasomotor
tone was measured in normal, ischemic limb and after cooling the
limb and concluded that TcOP2 can be used to assess the degree
of vasomotor tone in the skin that increases as ischemia worsens.
Warmth improves the cutaneous circulation in ischemic limbs [27]
Angiography has been used but difficult to predict the response.
Doppler ultrasound can determine the pressure in the thigh
and ankle. Ankle systolic pressure above 60mmHg and ABI >0.3
and patency of superficial femoral artery found to be successful
predictive test.
High correlation is observed between ABI and TcPO2.
Transmetatarsal TcPO2 <30mmHg may result in amputation
[28].The patients suffering from CRPS who are refractory to
conventional treatment or chemical/ RF ablation, spinal cord
stimulation is recommended to improve pain and dysfunction
[29]. With the introduction of ultrasound (USG) many benefits
like avoidance of radiation of fluoroscopy, prevention of vascular
injection by visualizing the spread of injectate with real time
US scan thus reducing the procedure time. Ryu et al conducted
USG Vs fluoroscopy guided LSGB in fifty patients of PVDs with
sympathetically mediated pain. Procedure time and success rate
were not significantly different in two groups although procedural
time was longer with USG technique, but onset time was faster.
[30] The newer modalities like spinal cord stimulation or surgical
revascularization are claimed to better outcomes but at present
very costly and beyond reach of many centres [31]. limitation
of the study by Explanation: The chemical neurolysis and RF are
established techniques, so this prospective observational study was
conducted. As the availability of radiofrequency machine was not
sure hence, we could not randomize the patients for three different
modalities of the treatment for comparison of the efficacy with
chemical, RF and RF with chemical. The type of wounds, time of
presentation and difference in associated pathologies in groups of
patients, we have not compared the outcome in terms of progress in
healing and surgical interventions done. More studies are required
with similar comparisons to support the usefulness of combined
method of RF+ chemical over sole RF or chemical LSGB.
Conclusion
We observed significant reduction in VAS score, increase in WD and rise in Temp. of the limb in all the groups, but longer lasting effects seen in combined technique i.e.in Group RF+CH as compared to sole RF or chemical LSGB. The course of the disease was similar and satisfactory in all the groups.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication.
Source of Support
The Research work is partially funded by D Y Patil Medical College and University, Kolhapur (MH) India. (Letter No. DYPU/2014/112)
Acknowledgement
We acknowledge the support of Department of Surgery, D Y Patil Medical College & University while publishing this article.
References
- Boas RA, HatangdiVS, RichardsEG (1976) Lumbar sympathectomy: A percutaneous chemical technique. Adv Pain Res Ther 1:685.
- Richard Rauck. Sympathetic Nerve Blocks: Head, Neck and trunk. In P Prithvi Raj. Practical Management of Pain.MOSBY,INC(3rdEdn) pp.673-678.
- Fyfe T, Quin RO (1975) Phenol sympathectomy in the treatment of intermittent claudication: a controlled clinical trial. Br J Surg 62: 68-71.
- Herman BE, Dworecka F, Wisham L (1970) Increaseof dermal blood flow after sympathectomy as measured by radioactive sodium uptake. VascSurg4: 161-166.
- Christopher J (1981) Aspects of Treatment.Chemical lumbar sympathectomy withRadiological assessment. Annals of the Royal College of Surgeons of England 63: 420-422.
- Waldman SD, Winnie AP (1996) Interventional Pain Management Philadelphia, WB Saunders.
- Yuanyuan Ding, Peng Yao, hongxi li, Rongjie Zhao, guangyi Zhao (2018) Evaluation of combined radiofrequency and chemical blockade of multi-segmental lumbar sympathetic ganglia in painful diabetic peripheral neuropathy. Journal of Pain Research11: 1375-1382.
- Reid W, Watt JK, Gray TG (1970) Phenol injection ofthe sympathetic chain.Br J Surg57:45-50.
- Pernak, J (1988)Percutaneous radiofrequency thermal lumbar sympathectomy and its clinical use. Eburon.
- Haynsworth RF Jr, Noe CE (1991) Percutaneous lumbar sympathectomy: A comparison of radiofrequency denervation versus phenol neurolysis. Anesthesiology 74:459-463.
- Kline MT, Yin W (2001) Radiofrequency techniques in clinical practice. In: Waldman SD, editor. Interventional pain management (2ndEdn). Philadelphia: W.B. Saunders pp. 243-293.
- Dhafir A Alkhudhairi,Mohamed M Hashim,Ahmed A Oriba, Iftikhar Ali (2013) Complete Pain Relief after Combining Radiofrequency and Phenol for Lumbar Sympathectomy. Bahrain Medical Bulletin 35(1).
- Manjunath PS, Jayalakshmi TS, Dureja GP, et al. (2008) Management of Lower Limb Complex Regional Pain Syndrome Type 1: An Evaluation of Percutaneous Radiofrequency Thermal Lumbar Sympathectomy Versus Phenol Lumbar Sympathetic Neurolysis--A Pilot Study. Anesth Analg106(2): 647-649.
- BrunnF, MandlF (1924) Die Paravertebral Injection.ZurBekaempfungvisceralerSchmerzen.WienKlinAschsch37:511.
- Huang J (2002) Letter to the Editor: The History Of Chemical Lumbar Sympathectomy. The Internet Journal of Anesthesiology7:1.
- Kha Tran, Steven Frank, Srinivasa Raja, Hossam El-Rahmany, Lauren Kim, et al. (2000) Lumbar sympathetic block for sympathetically maintained pain: Changes in cutaneous temperatures and pain perception. AnaesthAnalg 90(6): 1396-1401.
- Bhattarai BK, Rahman TR, Biswas BK, Sah BP, Agarwal B (2006) Fluoroscopy guided chemical lumbar sympathectomy for lower limb ischaemic ulcers.JNMA45: 295-299.
- Agarwal P, Sharma D (2009) Lumbar Sympathectomy Revisited: Current Status in Management of Peripheral Vascular Diseases. The Internet Journal of Surgery18(1): 1-5.
- Manchikanti L (2000) The role of radiofrequency in the management of complex regional pain syndrome. Curr Rev Pain4(6): 437-444.
- Rampal Singh, Aparna Shukla, Lakhwinder Singh Kang, Anand Prakash Verma (2014) Chemical lumbar sympathetic plexus block in buerger’s disease: Current scenario. Indian Journal of Pain28 (1): 24-28.
- Usmani H, Hasan M, Alam MR, Harris SH, Mansoor T, et al. (2016) Effect of preamputation lumbar sympathectomy on stump pain of lower limbs in patients of thromboangitisobliterans (Buerger's disease). Indian J Pain 30:132-137.
- Stevens RA, Stotz A, Kao TC, Powar M, Burgess S, et al. (1998) The relative increase in skin temperature after stellate ganglion block is predictive of a complete sympathectomy of the hand. Reg Anesth Pain Med 23: 266-270.
- Schmid MR, Kissling RO, Curt A, Jaschko G, Hodler J (2006) Sympathetic skin response: Monitoring of CT-guided lumbar sympathetic blocks. Radiology 241: 595-602.
- Park SY, Nahm SG, Kim YC, Lee SC (2009) The cutoff rate of temperature to interpret the successful lumbar sympathetic block. The Korean Pain Society The forty-nine Scientific Meeting (11), Seoul.
- Kim YC, Bahk JH, Lee SC, Lee YW (2003) Infrared thermographic imaging in the assessment of successful block on lumbar sympathetic ganglion. Yonsei Med J44:119-124.
- Creager MA (1997) Clinical assessment of the patient with claudication: the role of the vascular laboratory. Vasc Med2(3):231-237.
- Rooke TW, Hollier LH, Osmundson PJ (1987) The influence of sympathetic nerves on transcutaneous oxygen tension in normal and ischemic lower extremities. Angiology 38(5):400-410.
- Van EijsF, Stanton-HicksM, Van ZundertJ, et al. “Complex regional pain syndrome.” Pain Practice11(1): 70-87.
- Ryu JH, Lee CS, Kim YC, Lee SC, Shankar H, et al. (2018) Ultrasound-assisted versus fluoroscopic-guided lumbar sympathetic ganglion block: A prospective and randomized study. AnesthAnalg126:1362-1368.
- Kumar K, Toth C, NathrK, VermaaK, Burgess JJ (1997) Improvement of limb circulation in peripheral vascular disease using epidural spinal cord stimulation in prospective study. J Neurosurg 86: 662-699.
- Mekhail NA, Mathews M, Nageeb F, Guirguis M, Mekhail MN, et al. (2011) “Retrospective review of 707 cases of spinal cord stimulation: indications and complications.” Pain Practice 11(2): 148-153.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...