Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Research Article(ISSN: 2644-1403) 
Propofol - In One-Day Surgery in Children Volume 3 - Issue 3
Nasibova EM*
- Azerbaijan Medical University, Baku
Received: May 20, 2020; Published: June 02, 2020
Corresponding author: Nasibova EM, Azerbaijan Medical University, Baku
DOI: 10.32474/GJAPM.2020.03.000161
Keywords: Propofol, One-day surgery, Premedication
Introduction
Propofol (diprivan) is the drug of choice in one-day surgery in children. The use of the drug provides rapid awakening (due to rapid redistribution and short half-life) and a minimum incidence of postoperative complications. Total intravenous anesthesia with propofol infusion or bolus administration is an easily managed anesthesiologist, anesthesia comfortable for the patient [1-13].
The aim of the study: optimization of anesthetic benefits in one-day surgery by using propofol.
Material and Research Methods
The study included 58 patients operated on for inguinal and umbilical hernias, dropsy of testicular membranes, cryptorchidism, varicocele, hemangiomas of various localization, phimosis and paraphimosis. Depending on the age of the children, this group was divided into 3 subgroups: IA (n = 12) age 0-3 years, IB (n = 33) - 4-7 years old and IC (n = 13) - 8-16 years old. This study was carried out in five stages. For intravenous anesthesia in children, you must have access to a vein. To prevent a negative attitude of the child to this procedure, the local anesthetic drug EMLA was used. EMLA - eutectic mixture of local anesthetic, is an emulsion system in which the oil phase consists of a eutectic mixture of the bases of lidocaine and prilocaine in a 1: 1 ratio. The drug is available in the form of 5% cream and patch. One gram of cream or one patch contains 25 mg of prilocaine. EMLA cream was applied 2-3 g on a selected area, which was then tightly covered with a gauze cloth. After removing the wipes, the remaining cream was removed. 40 minutes after applying the cream with the introduction of the needle, a motor reaction to the manipulation was not observed. At the initial stage of the use of propofol in our clinic, we titrated the initial and maintenance doses of it. To date, we have experience with the use of propofol in various manipulations and surgical interventions in more than 3,000 children aged 0 to 16 years. The optimal, according to clinical data, induction dose of propofol in children older than 5 years was 3.5 ± 0.3 and 4.0 ± 0.4 mg / kg in children under 5 years of age. Approximately 30-40 seconds after the start of propofol administration, rapid breathing occurred in all patients, which then turned into apnea in the majority. During induction, a decrease in oxygen saturation to 92-94% was noted. Clinically, in 5 patients, motor sweeping movements were noted and in 6 patients - shortterm hypoventilation. After oxygen hyperventilation, an increase in SpO2 of 98-99% was noted. Central analgesia was carried out with fentanyl at the rate of 1.5-2 μg/ kg.
The Results of the Study
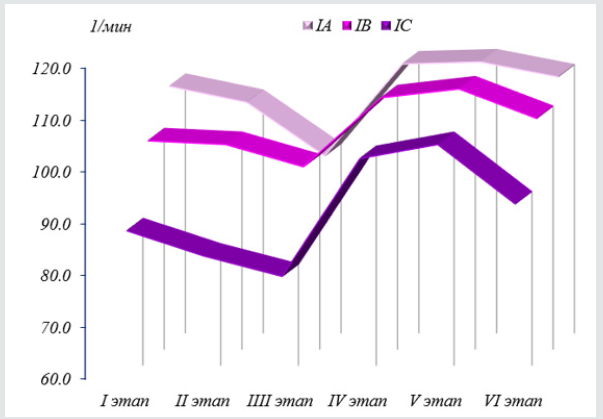
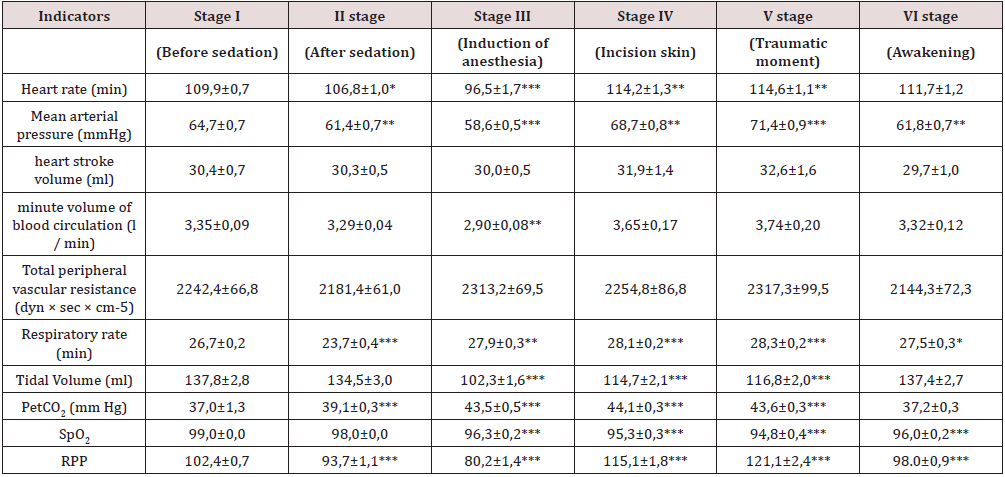
Changes in the indicators of central hemodynamics and external respiration relative to the first stage during intravenous total anesthesia (propofol + fentanyl) are presented in Table 1. Basically, in all age groups, the performance of the cardiovascular system remained at the level of the initial values, however, certain hemodynamic changes characterizing the effect of propofol were revealed. During induction in anesthesia, heart rate (HR) decreased in the subgroup in patients aged 0-3 years (IA on average by 7.5% (p <0.001), and in patients aged 4-7 years (IB) by 4.8 (p <0.05), and in patients aged 7-16 years (IC) by 10.0% (p <0.01) compared with the initial stage of the study. The average blood pressure (SBP) decreased in patients aged 0-3 years by an average of 10.8% (p <0.001), and in children aged 4-8 years by 10.2% (p <0.001), and in children at the age of 8-16 years - by 13.1% (p <0.001). Changes in vascular tone were demonstrated in terms of total peripheral resistance, which decreased to a greater extent in patients of the IC subgroup (8-16 years) by 9.3% (p <0.01) during induction of anesthesia compared with the initial stage, in the IA subgroup (0-3 years) - 2.9% (p <0.01), and in the IB subgroup (4-7 years) - 3.8% (p <0.01). An increase in stroke volume of the heart (CCS) was noted by the IA subgroup by 3.3% (p <0.01), in the IB subgroup by 4.2% (p <0.01) and in patients with the IC subgroup by 0.5% (p <0.01) compared with the initial stage was noted before the skin incision. Note: the statistical significance of the differences in indicators with respect to the initial data: * - p <0.05; ** - p <0.01; *** - p <0.001.
Table 1: Hemodynamic and external respiration in patients with (propofol + fentanyl) in the age group 0-3 years.
The minute volume of blood circulation (IOC) at the induction
stage mainly remained almost at the level of indicators of the previous
stage in all groups. As can be seen from the reaction directly to the
induction of anesthesia, the reaction of the blood circulation to an
operative trauma fully corresponded to the picture of transitional
inactivity. Since the IOC has not changed almost, a change in the
main components (a decrease in heart rate and an increase in
stroke volume of the heart (UO) against a background of a decrease
in mean arterial pressure (SBP) and total peripheral resistance
(OPSS) allows us to conclude that the hemodynamic regime has
reached a more intense regulation mechanism that accompanies
increased cardiac performance to maintain overall cardiovascular
system performance in the form of physical inactivity at baseline.
This type of hemodynamic regime cannot be considered useful since it can lead to the depletion of compensatory mechanisms. The
characteristic imbalances of the main parameters of the volumetric
blood flow indicate hemodynamic stress that occurred against
the background of the action of propofol in all groups during the
induction of anesthesia. All this clearly and objectively characterizes
the vasodilating properties of propofol, as a factor that causes the
most typical changes in central hemodynamics. By the time of the
skin incision after administration of fentanyl at the rate of 3 μg/
kg, an unexpected increase in heart rate was observed by 8.7%
(p <0.001) in patients of the IA subgroup, by 8.2% (p <0.001) in
patients of the IV subgroup and by 15, 8% (p <0.001) in patients
with IC subgroups compared with the previous stage (Figure 1).
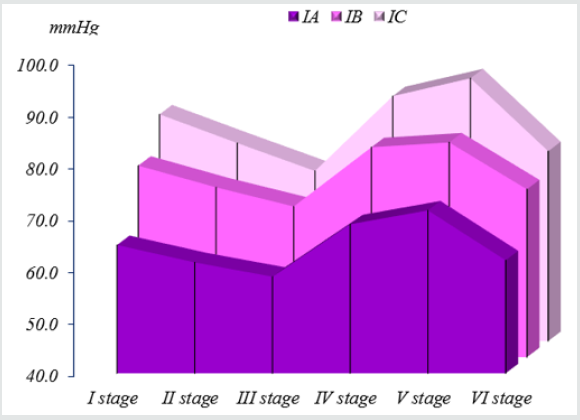
An increase in mean arterial pressure was also observed
in patients of the I A subgroup by 4.8%, in patients of the IB
in the subgroups by 4.6% and the I C subgroups by 4.2%.
These changes indicated a lack of analgesia and forced us to an
additional administration of fentanyl at a dose of 1.5 μg/kg. At
stage V (the traumatic moment of the operation), the studies,
despite the additional administration of fentanyl, did not improve
hemodynamic parameters. So, in patients with IA subgroups, heart
rate and mean blood pressure increased by 10.3% (p <0.001) and
7.2% (p <0.001), respectively, compared with the initial stage, in
group I B subgroups by 4.2% ( p <0.001) and 5.8% (p <0.001), and
in patients with IC, the subgroups were 18.8% (p <0.001) and 8.1%
(p <0.001), respectively (Figure 2). A significant increase in RPP was
also detected by 21.3% (p <0.001) in patients of the IA subgroup,
by 19.5% (p <0.001) in the IB subgroup, by 29.3% (p <0.001) in
patients of the IC subgroup compared to the previous step. And
this testified to the inadequacy of anesthesia and prompted us to
additional administration of fentanyl. Moreover, the total amount
of fentanyl introduced during the entire operation was 5-6 μg/kg.
Indices of external respiration after premedication at the
induction stage tended to decrease and indicated moderate
hypoventilation. At the traumatic stage of the study, an increase
in BH was observed, which was associated with the appearance of
pain. At this stage, a decrease in SpO2 was also observed. In 5 patients
hypoventilation was observed and required manual ventilation
of the lungs with a bag and spontaneous breathing was quickly
restored. In the period of awakening, the indicators of external
respiration tended to increase and approached the initial values.
Starting from the 15th minute from the last injection of propofol,
more than 50% of children could follow the command ″ open their
eyes ″, ″ cough ″. In some children, hypersalivation was noted. At
the 20th minute, 90% of the children could answer simple questions
and were oriented in time and space. At the 25th minute from the last
bolus of propofol and fentanyl, all patients could answer complex
(commensurate with age) questions, were oriented in time and
space, and could even share their impressions. Some patients even
expressed a desire to stand up, move independently, although they
felt muscle weakness. After 40-60 minutes, patients could walk
in the ward, although many noted moving freely and comfortably
much earlier.
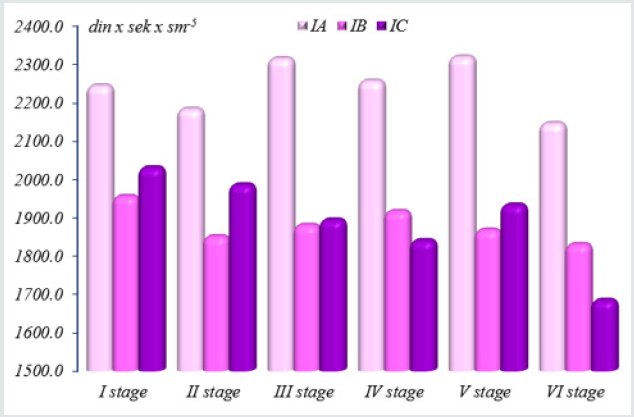
Thus, propofol induction proceeded with a hypodynamic type
of blood circulation. At the most traumatic time of the operation,
despite an increase in the dose of fentanyl, hemodynamic parameters
were hyperdynamic type of blood circulation, associated with
insufficient relief of the pain component. And an increase in the
dose of fentanyl led to the development of hypoventilation with
subsequent apnea, which required mechanical ventilation. After
mask ventilation, respiratory failure was easily corrected and SpO2
rose to 97-99%. The total time of induction into anesthesia with
propofol and fentanyl was 30-60 seconds, and a complete exit from anesthesia in patients of group I was noted at the 20th minute.
Clinically, in 4 patients, erratic epileptiform movements were noted
and in 5 patients - an attack of short-term apnea. None of the
patients in the postoperative period had apnea. During induction
in anesthesia in patients of group I (propofol + fentanyl), the
circulatory reaction fully corresponded to the picture of transitional
physical inactivity. Since the IOC has not changed almost, a change in
the main components (decrease in heart rate and increase in stroke
volume of the heart) with a decrease in mean arterial pressure and
general peripheral vascular resistance allow us to conclude that
the hemodynamic regime has entered a more intense regulation
mechanism that accompanies an increase in heart function to
maintain overall productivity of the cardiovascular system in the
mode of physical inactivity at the level of the initial values. This
type of hemodynamic regime cannot be considered useful, since
it can lead to the depletion of compensatory mechanisms. The
characteristic imbalances of the main parameters of the volumetric
blood flow indicate hemodynamic stress, which occurred against
the background of the action of propofol and inadequate pain relief
in all groups in the most traumatic stage of the operation (Figure 3).
Conclusion
Analyzing the results obtained, it should be noted that anesthesia during ″ small ″ surgical interventions with propofol and fentanyl is not an optimal method. Since at the most traumatic time of the operation, it is necessary to increase the dose of fentanyl, and this leads to hypoventilation with the subsequent development of apnea, which requires correction.
References
- Michel Foehn ER (2015) Adult and pediatric anesthesia/sedation for gastrointestinal procedures outside of the operating room. Curr Opin Anaesthesiol28:469-
- Youn AM, Ko YK, Kim YH (2015) Anesthesia and sedation outside of the operating room. Korean J Anesthesiol68:323-
- Hinkelbein J, Lamperti M, Akeson J, Santos J, Costa J, et al (2018)European Society of Anaesthesiology and European Board of Anaesthesiology guidelines for procedural sedation and analgesia in adults. Eur J Anaesthesiol35:6-24.
- American Society of Anesthesiologists. Continuum of depth of sedation: definition of general anesthesia and levels of sedation/analgesia.
- Butterworth JF, Mackey DC, Wasnick JD, editors (2018)Clinical anesthesiology. (6thEdn). New York: McGraw-Hill Education. Analgesic agentspp.187-197.
- Butterworth JF, Mackey DC, Wasnick JD, editors (2018)Clinical anesthesiology. 6th ed. New York: McGraw-Hill Education. Intravenous anesthetics pp.171-185.
- Morgan JF, Mackey DC, Wasnick JD, editors. (2018) Morgan & Mikhail's clinical anesthesiology. (6thEdn). New York: McGraw-Hill Education. Intravenous anesthetics pp.324-362.
- Machata AM, Willschke H, Kabon B, Kettner SC, Marhofer P(2008) Propofol-based sedation regimen for infants and children undergoing ambulatory magnetic resonance imaging. Br J Anaesth 101:239-243.
- Brechmann T, Maier C, Kaisler M, Vollert J, Schmiegel W, et al. (2018) Propofol sedation during gastrointestinal endoscopy arouses euphoria in a large subset of patients. United European Gastroenterol J6:536-546.
- APP Pharmaceuticals (2019)Diprivan (propofol) injectable emulsion for IV administration prescribing information.
- Michel-Macías C, Morales-Barquet DA, Reyes-Palomino AM, Machuca-Vaca JA, Orozco-Guillén A (2018) Single dose of propofol causing propofol infusion syndrome in a newborn. Oxf Med Case Reports2018:omy023.
- Furniss SS, Sneyd JR (2015) Safe sedation in modern cardiological practice. Heart101:1526-1530.
- Wheeler DS, Vaux KK, Ponaman ML, Poss BW (2003)The safe and effective use of propofol sedation in children undergoing diagnostic and therapeutic procedures: experience in a pediatric ICU and a review of the literature. Pediatr Emerg Care19:385-92.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...